Prevalence of venous leg ulcer: the importance of the data collection method
Vascular Surgery
Skaraborg Hospital/KSS
Skövde, Sweden
ABSTRACT
Many epidemiological studies have been performed to assess leg ulcer prevalence, but not all have given reliable results due to weaknesses in the methodology. A proper prevalence assessment is not easily done and requires time and effort. Most studies have just focused on prevalence of leg ulcers of all causes and only a few have really validated the leg ulcer diagnosis objectively by use of hand-held Doppler, color Doppler ultrasound, or plethysmography. There are many pitfalls in performing a prevalence study of venous leg ulcers which introduce a risk of misinterpretation of the true prevalence. Some of these pitfalls and their likely effects are presented. Based on the available and most qualitative studies the overall prevalence of venous ulcers (healed + open) is, astonishingly stable between different countries and over time, around 1% in most populations. The point prevalence of open ulcers is more variable and is likely to be in the region of 0.1-0.3% depending on whether or not people who self-treat are included.
INTRODUCTION
Leg ulcers have plagued mankind since ancient times and still pose a considerable burden for both patients and carers in most countries of the world. With more elderly in the populations this problem is likely to increase unless effective actions are taken to treat the various diseases that cause leg ulcerations. Venous disease is the most common causative factor for leg ulcers, but has to be properly diagnosed in order to establish a reliable diagnosis. This has been overlooked in several epidemiological studies attempting to establish the prevalence of leg ulcers and venous ulcers in particular. There are different assessments of prevalence, which is a measurement of the occurrence of a disease or disorder within a certain population, namely point prevalence and period prevalence estimates. The latter is most often used for a lifetime period and gives an overall prevalence, as opposed to point prevalence, which measures the number of patients with open ulcers during a narrow time period, usually one to three months. One can quite often see misuse of prevalence data in reviews by mixing overall prevalence figures with point prevalence data, causing an inaccurate wide range that leads to incorrect interpretations of prevalence data between countries and studies. To analyze the methods used in various studies is therefore of utmost importance in order to generate accurate comparisons and to provide the most reliable data in order to assess the magnitude of the problem. The aim of this article is to point out the variations in methodology in previous epidemiological studies and how these differences can affect the result, and to present available data on venous leg ulcer prevalence. In reality very few studies can really be used to give reliable data on venous ulcer prevalence.
WHAT IS A VENOUS LEG ULCER?
What may be obvious to some is not clear to others, even within the medical profession. It is even more difficult for patients or relatives, who frequently misidentify erosions caused by venous eczema as an ulcer.1 A definition of a leg ulcer or a venous leg ulcer is frequently missing in many prevalence studies.2 A venous ulcer is usually considered as a “chronic” disorder, although we now know that it does not have to be, and therefore a venous ulcer has to have been present for 4-6 weeks in order to distinguish it from an “acute” ulcer. A reliable diagnosis is mandatory, especially if you attempt to sort out venous ulcers from all other causes of leg ulceration. We have previously shown that simple reliance on clinical examination, and signs and symptoms of probable venous disease, without the support of noninvasive diagnostics (Doppler), will result in misdiagnosis every fourth ulcer.3 Today it is reasonable to require objective data proving venous dysfunction and excluding other major diseases, such as arterial insufficiency, before diagnosing a venous ulcer. The most used diagnostic tool today is color Doppler ultrasound (CDU), which is the gold standard in diagnosing venous dysfunction. Alternative techniques sometimes used are plethysmography and hand-held Doppler assessments both of which give more limited and less detailed information. That this is a reasonable requirement is perhaps more easily understood if you realize that the diagnostic spectrum regarding leg ulcers is much diversified, with a number of diagnoses apart from venous and arterial ulcers.4,5 Not least it is important to realize that mixed arterial and venous ulcers and multifactorial ulcers are becoming more and more common, probably because of aging populations. Today it is no longer valid to diagnose a venous ulcer based on signs and symptoms, without the aid of noninvasive diagnostics.
WHY ARE PREVALENCE DATA IMPORTANT?
Epidemiological studies are used to assess the prevalence (occurrence) of diseases or disorders within populations in order to establish the magnitude of a certain problem. Usually cross-sectional studies have been used to assess the number of patients with a certain disease within the health care system. Large random samples have been used to assess populations and have the advantage of including people who self-treat. Prevalence data from such studies will serve as a valuable basis for the planning of appropriate actions to deal with the problem, in this case venous leg ulcers. By repeating a prevalence study within a defined geographical area, we have a unique opportunity to assess the effect of treatment changes.6
A matter often creating some confusion is that there are various prevalence estimates and that the difference between incidence and prevalence is not always understood. The definitions of these terms are found in Table I. When venous ulcers are concerned we often speak of either point prevalence or overall prevalence, the first meaning the proportion with open ulcers over a certain short period of time and the second meaning the proportion of people who have ever had a venous leg ulcer, thus including both open and healed ulcers. The incidence of venous leg ulcers is estimated to be one tenth of the current point prevalence, meaning that only one out of ten venous ulcers is newly developed.5
In Skaraborg we used data from our first epidemiological studies (1988-1992)1,3,4,7-9 to improve leg ulcer management in general and venous ulcer treatment in particular. By a repeat study in 2002 we found that the prevalence of venous ulcers had been decreased by 46% within the health care system, giving a strong indication that our changed management strategy was successful.6 In short, the management strategy was based on multidisciplinary cooperation, training of carers in the community, improved proper use of bandaging and compression stockings and, maybe most important, increased use of varicose vein surgery. Without the repeat study in 2002 it would have been much more difficult to detect the result of this change of management strategy.
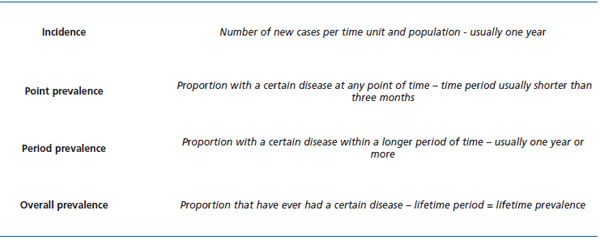
Table I. Definitions of incidence and the various form of prevalence estimates.
METHODOLOGICAL PITFALLS
To perform an epidemiological study properly takes time and effort in order to get a reliable result. Prevalence is easily underestimated if the study is inadequately prepared. Overestimation is also possible, but generally for other reasons, which will be discussed later. Methodology is crucial and should be studied first when reading an article dealing with prevalence data, in order to be able to evaluate the results presented. Even in a meticulously performed study one should be aware that the results are often based on assumptions and that the result is not always representative of the general population in, for example, the whole country. Cautious generalization may be appropriate.
Prevalence data are often harvested from cross-sectional studies or large population samples. The former investigate a defined cohort, generally all patients receiving treatment from health care professionals within a relatively short time frame, usually 1-3 months. The latter usually consist of randomly selected people of a certain age range, not necessarily previously in contact with the health care system. The benefit of population samples is that people who self-treat are included, unlike in cross-sectional studies. The drawback of a population sample is that usually not all age groups are represented.
What are the pitfalls of a cross-sectional study? As mentioned above it is necessary to contact all potential carers within the health care system in an area where leg ulcer patients are likely to be treated and persuade them to participate and to contribute patient data. A lot of time is needed to ensure that most carers are providing accurate responses. Failing this, underestimation is likely. As an example, we found in the Skaraborg study in 20026 that only 361 individual patients were initially reported from 79 units. Following several reminders this figure rose to 802 patients reported from 250 units, so reminders are necessary to get a reliable result. To facilitate recruitment it is important to avoid approaching carers and patients with lengthy questionnaires. Such forms take time to fill in and introduce a risk of dropout because of lack of time for the carer or patient or both. Make the primary recruitment form as simple as possible, including only age, gender, identification number, and address. More detailed information can be gathered later. To avoid erroneous inclusions, the carer may mark the location of the ulcer on a drawing of a leg. There are examples of very low point prevalence reported from studies using extensive questionnaires,10 which raises doubts about the reliability of such estimates.
For prevalence data to be reliable, the study has to be large enough. By calculating the 95% confidence interval, certainty is possible when examining a smaller population. Validation of all or a randomly selected sample of the reported patients is mandatory to determine the number of false positives and to establish the diagnosis, which is usually done nowadays by performing CDU in combination with clinical examination. It is not appropriate to rely on a venous ulcer diagnosis by the carer without verification from a previous objective noninvasive assessment. Without objective validation there is a high risk of overestimating venous leg ulcer prevalence. One example is a study from Ireland11 that only assessed ankle pressures to diagnose arterial ulcers and most other ulcers were considered as being venous, clearly resulting in an overestimation of venous ulcer point prevalence. Leg ulcer diagnosis is more complicated than that.4,5
A cross-sectional study involves selection bias since only patients treated within the health care system will be included. Such a study will give the workload for health care professionals, but there are in addition people caring for their ulcers on their own. A population sample will overcome this by including all people within the selected sample. What are the problems of population sample study? The biggest problem is that they need to be fairly large (~10 000 people or even more) in order to detect enough patients with ulcers so that a reliable prevalence estimate can be made. These studies are expensive, timeconsuming, and difficult to perform. To overcome this we selected patients using a very simple questionnaire to identify those who really had a history of leg ulcer.1 Other studies have examined all patients, but then the main object was to look at venous disease in general and not specifically venous ulcers and the samples were therefore smaller.12,13 resulting in more uncertain estimates of venous ulcer prevalence. The youngest and oldest age groups are usually excluded in such surveys, because ulcers are seldom found below the age of 30 and the eldest are likely to have difficulty in attending. However, most elderly people are treated by health care professionals and the prevalence can be adjusted by using information from previous cross-sectional studies. Furthermore, it is important to use random selection when the sample is defined to avoid introducing unnecessary selection bias. Samples based on cohorts attending outpatient departments are often heavily selected and can not generally be used to assess the magnitude of the problem within the population, but merely show the workload for that specific department. The need for validation is high and usually all or a randomly selected sample of patients reporting ulcers are invited for more detailed examination with the aid of objective noninvasive techniques, usually Doppler and CDU and sometimes also plethysmographic methods.2 Getting people to attend for the detailed examination can be a problem, which is generally bigger in population sample studies where many are likely to be quite healthy. In fact, all studies have shown attendance rates lower than 60%.12,13 In our own, slightly differently designed, study the attendance rate among those who claimed a history of leg ulceration was even lower (46%), but we were able to validate a random sample of the dropouts and to verify leg ulcer history in a percentage similar to that among those examined.1 We learned that people in general have difficulty in discriminating an ulcer from erosions due to venous eczema. The false-positive response rate was high (43%), mostly due to venous eczema. This underlines the importance of validating studies of patients claiming a history of ulceration to avoid overestimation of prevalence of venous ulceration. Table II summarizes the most common pitfalls in prevalence studies.
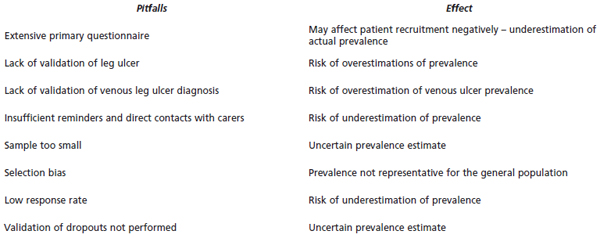
Table II. Pitfalls in performing prevalence studies and their effects on the results.
VENOUS ULCER PREVALENCE
Numerous studies have assessed leg ulcers regardless of etiology, but very few give details of venous ulcer prevalence, since not many have validated the diagnoses.2,5 One of the most uniform prevalence estimations regards overall prevalence of venous ulcers. Around 1% of the adult population has a history of healed or open venous leg ulcers,14,15 an estimate that seems astonishingly stable over the years and in many different countries (Table III). Based on data from Skaraborg in Sweden, we found that a roughly equal proportion had chronic lower limb ulceration of causes other than venous (Table IV).
There are few published point prevalence estimates of venous ulcers (Table III). In six studies the diagnosis of a venous ulcer was validated with noninvasive methods.1,3,6,8,10,17 Four studies of cross-sectional design assessed prevalence among venous ulcer patients receiving professional treatment,3,6,10,17 and the other two were based on a random population sample1 and a selected population sample,8 respectively. The lowest point prevalence, 0.024%, was found in the latest published study from the UK.10 That prevalence was, however, based on a study with a questionable methodology using an extensive questionnaire, which is likely to bias recruitment of patients negatively, and therefore probably underestimates the true point prevalence. The highest prevalence was not surprisingly found in the two studies that were based on large random population samples and thus also included people who self-treat. Both in Germany16 and Sweden1 the point prevalence was 0.29%, but in the German study no objective diagnostics were used. The recently performed population studies in Edinburgh12 and Bonn13 found very few actual ulcer cases and therefore have not generated any reliable data regarding point prevalence. The observed overall prevalences from these studies were, however, in line with the expected 1%, albeit slightly lower due to the chosen age ranges (Table III). Reported prevalences for patients receiving professional care range from 0.06% to 0.20%.3,6,8,17 It seems reasonable to expect the point prevalence in the total population to be somewhere in the region of 0.1% to 0.3% in most Western populations, although local variations are likely to exist. The highest point prevalences were found in population studies including people who self-treat.1,16 As a result of our previous three epidemiological studies in Skaraborg County (population 270 800), we have been able to weigh the separate results in a more detailed estimate shown in Table IV.
CAN VENOUS ULCER PREVALENCE BE REDUCED?
The conditions and evidence have never been better than they are today provided that the right actions are taken. In Skaraborg we have been able to reduce the point prevalence of venous ulcer from 0.16% to 0.09% within the health care system, representing a reduction of 46% within a 14-year period.6 This is the first, but surely not the last, study that will show that a change of management will result in a detectable reduction in leg ulcer point prevalence. In 2005 we repeated a large population sample study (10 000 people aged 30-89 years) and a preliminary analysis has shown no more ulcer patients in that study, a result that points in the same positive direction. Overall prevalence is likely to be lowered over the long term, but at a slightly slower speed. Why were we able to reach this result? We feel that the creation of organized care pathways has been important in the multidisciplinary cooperation and teamwork around these patients. A very important step has been to point out the value of a proper early diagnosis by offering patients with presumed venous ulcers a diagnostic CDU. In this way we detect early patients with superficial venous insufficiency and incompetent perforators that may be correctable surgically. Our policy has been to offer patients this kind of surgery early and to follow up healing by proper bandaging and later with custom fit compression stockings in case of any persisting deep or superficial venous insufficiency. That this was a wise policy has been supported by results from the ESCHAR study in the UK where surgery significantly reduced the risk of leg ulcer recurrence compared with conservative compression treatment alone.18,19 It is likely that the early surgical intervention was the most important component in reducing the number of patients with open venous ulcers in our population. This is validated by the good long-term healing and recurrence results from a prospective study on subfascial endoscopic perforator surgery performed for venous ulcers in Skaraborg during the same period.20 However, it is important to point out that surgery would probably not have been so successful without all the other improved more conservative components of leg ulcer management. Together all of the actions raised leg ulcer management to a higher level to the benefit of both patients and carers. For society the result indicates yearly cost savings of around 1.7 to 2.3 million Euros in Skaraborg alone.6 This emphasizes the enormous yearly spending mainly on providing dressings and bandaging for venous ulcer patients.21 One varicose vein operation equals the cost of approximately three to four months of dressing changes and is money well spent when considering the savings involved.
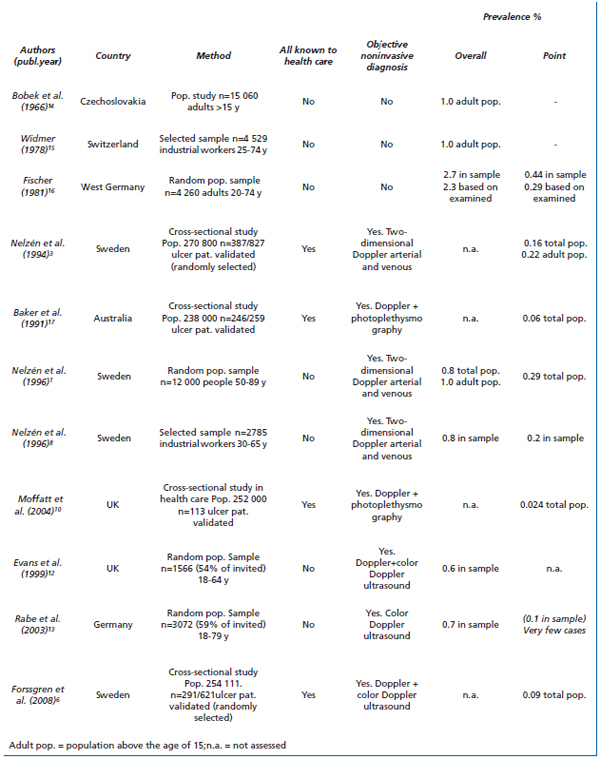
Table III. Estimates of venous leg ulcer prevalence.
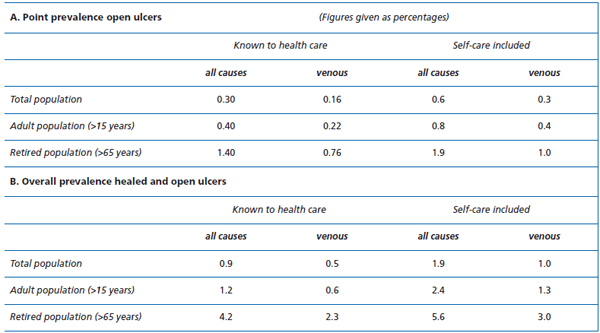
Table IV. Combined prevalence estimates, from Skaraborg county, of leg ulcers of all causes and of venous ulcers.5
CONCLUSION
Reliable epidemiological data regarding point prevalence and overall prevalence of venous ulcers are hard to come by and there are few representative studies where objective methods have been used. It is important to be aware of the pitfalls in methodology so as to judge the reliability of results and to compare them with findings from other studies. If certain pitfalls are not avoided, overestimation or underestimation is likely. The most reliable studies suggest that both point prevalence and overall prevalence of venous ulcers are still quite high and there appears to be room for management improvements in reducing the size of the problem of venous leg ulcers. That this is possible has been shown from Skaraborg in Sweden where leg ulcer point prevalence has been reduced by 46% within a 14-year period. If this can be achieved in Sweden, it ought also to be possible elsewhere. The future for leg ulcer patients has never been brighter.
References
2. Graham ID, Harrison MB, Nelson EA, Lorimer K, Fisher A. Prevalence of lower-limb ulceration: a systematic review of prevalence studies. Adv Skin Wound Care. 2003;16:305-316.
3. Nelzén O, Bergqvist D, Lindhagen A. Venous and non-venous leg ulcers: Clinical history and appearance in a population study. Br J Surg. 1994;81:182-187.
4. Nelzén O, Bergqvist D, Lindhagen A. Leg ulcer etiology — a cross-sectional population study. J Vasc Surg. 1991;14:557-564.
5. Nelzén O. Patients with chronic leg ulcers: Aspects of epidemiology, aetiology, clinical history, prognosis and choice of treatment. Comprehensive Summaries of Uppsala dissertations from the Faculty of Medicine 664. Uppsala: Acta Universitatis Upsaliensis. 1997;1:1-88.
6. Forssgren A, Fransson I, Nelzén O. Leg ulcer point prevalence can be decreased by broad-scale intervention: a follow-up cross-sectional study of a defined geographical population. Acta Derm Venereol. 2008;80:252-256
7. Nelzén O, Bergqvist D, Hallböök T, Lindhagen A. Chronic leg ulcers: An underestimated problem in primary health care among elderly patients. J Epidemiol Community Health. 1991;45:184-187.
8. Nelzén O, Bergqvist D, Fransson I, Lindhagen A. Prevalence and aetiology of leg ulcers in a defined population of industrial workers. Phlebology. 1996;11:50-54.
9. Nelzén O, Bergqvist D, Lindhagen A. Long term prognosis for patients with chronic leg ulcers: a prospective cohort study. Eur J Vasc Endovasc Surg. 1997;13:500-508.
10. Moffatt CJ, Franks PJ, Doherty DC, Martin R, Blewett R, Ross F. Prevalence of leg ulceration in a London population. Q J Med. 2004;97:431-437.
11. O´Brian JF, Grace PA, Perry IJ, Burke PE. Prevalence and aetiology of leg ulcers in Ireland. Ir J Med Sci. 2000;169:110-112.
12. Evans CJ, Fowkes FGR, Ruckley CV, Lee AJ. Prevalence of varicose veins and chronic venous insufficiency in men and women in the general population: Edinburgh Vein Study. J Epidemiol Community Health. 1999;53:149-153.
13. Rabe E, Pannier-Fischer F, Bromen K, et al. Bonner Venenstudie der Deutschen Gesellschaft für Phlebologie. Phlebologie. 2003;32:1-14.
14. Bobek K, Cajzl L, Cepelak V, Slaisova V, Opatzny K, Barcal R. Étude de la fréquence des maladies phlébologiques et de l´influence de quelques facteurs étiologiques. Phlebologie. 1966;19:227- 230.
15. Widmer LK. Peripheral Venous Disorders. Basle Study III. Bern, Switzerland: Hans Huber; 1978.
16. Fisher H. Venenleiden: Eine Repräsentative Untersuschung in der Bevölkerung der Bundesrepublk Deutschland (Tübinger-studie). München: Urban Schwartsenberg, 1981.
17. Baker SR, Stacey MC, Jopp-McKay AG, Hoskin SE, Thompson PJ. Epidemiology of chronic venous ulcers. Br J Surg. 1991;78:864-867.
18. Barwell JR, Davies CE, Deacon J, et al. Comparison of surgery and compression with compression alone in chronic venous ulceration (ESCHAR study): randomised controlled trial. Lancet. 2004;363:1854-1859.
19. Gohel MS, Barwell JR, Taylor M, et al. Long term results of compression therapy alone versus compression plus surgery in chronic venous ulceration (ESCHAR): randomised controlled trial. BMJ. 2007;335:83-88.
20. Nelzén O, Fransson I. True long term healing and recurrence of venous leg ulcers following SEPS combined with superficial venous surgery: a prospective study. Eur J Vasc Endovasc Surg. 2007;34:605-612.
21. Nelzén O. Leg ulcers: economic aspects. Phlebology. 2000;15:110-114.
