Calf muscle pump dysfunction in the patients with severe chronic venous insufficiency
Pszczyna, Poland
ABSTRACT
Severe chronic venous insufficiency is often caused by calf muscle pump failure. Proper outflow of venous blood from the lower extremities depends on three factors: vein patency, competence of valves, and proper calf muscle function. All disturbances in these three components result in venous hypertension and chronic venous insufficiency. Failure of the muscle pump seems to be the most under-estimated pathophysiological factor, as Doppler sonography and phlebography cannot assess its function. To assess calf muscle pump function in patients with venous leg ulcers, 59 legs were examined by means of air plethysmography. The examination was performed in the supine and standing position. Insufficiency of the muscle pump in the supine position was revealed in 49% of cases, and in the standing position in 38%. In 24.5% of legs, an impaired muscle pump was found both in the supine and standing position. It was also found that in 73% of legs the venous outflow was compromised, and in 34% there was pathological reflux. However, in 18% of examined legs, the calf muscle pump impairment was the only abnormality. Patients with an insufficient calf muscle pump were older compared with those without this abnormality, and there were more longstanding ulcers in this group. Moreover, it was found that ulcers in legs with an insufficient muscle pump were larger, and their healing time was longer. It could be concluded that calf muscle pump failure is common in patients with venous leg ulcers, and this pathology can result in delay of healing of the ulceration.
INTRODUCTION
Venous return from the leg depends primarily on the emptying of the venous plexus in the muscles of the calf during the plantar flexion of the ankle in the presence of competent valvular system and the absence of obstruction of main veins. If these three parameters of proper functioning are intact, the blood is propelled inward (from superficial veins via perforators to the deep venous system) and toward the heart. Lack of physiological emptying of veins results in ambulatory venous hypertension, which finally can even lead to development of ulceration. Nowadays, most therapeutic decisions in phlebology are based on clinical and anatomic data. The role of functional tests remains underestimated.1 Furthermore, most patients with severe forms of chronic venous insufficiency have incompetence in many systems.
The aim of this study was to evaluate functional disturbances revealed in air-plethysmographic examination, as well as to estimate the clinical relevance of these abnormalities.
PATIENTS
Fifty-nine legs with open ulcerations in 48 patients, were examined. Patients were aged 33 to 87 years, mean 67 years. There were 35 female and 13 male patients (73% versus 27%). All ulcerations were regarded as “venous” due to their typical localization and other signs of chronic venous insufficiency: edema, varicosities, corona phlectatica, hyperpigmentation, etc. However, in some patients, ulcers were of mixed origin, eg, also related to arterial occlusive disease, diabetes mellitus, or rheumatoid arthritis.
METHODS
To assess function of venous system in these patients, air-plethysmographic method has been chosen, as this examination could be performed even in patients with profound skin changes, and several functional tests – assessing different components of venous physiologycould be done. As it was found (details are discussed further) that as far as proper healing of the ulcer was concerned, calf muscle pump function was of major clinical importance, this paper is focused on this part of plethysmographic examination.
Routinely – air-plethysmographic examination consists of some independent tests. Each of them serves purpose of assessment of different part of the proper venous blood flow. Changes of volume of veins are measured calculating the changes of pressure in the cuffs placed on the examined leg. Cuffs are filled with air under the pressure 6-8 mmHg (pressure in cuffs should not be higher to prevent compression of the veins). After the calibration, changes of pressure can be transferred to changes of volume. As veins are the only system in the leg, which can significantly and quickly change its volume, every change of pressure in cuffs is correlated with dilation or collapse of the veins.
To assess the presence and volume of venous reflux, the examined leg is elevated, and then – lowered. If there is venous reflux, pressure in cuffs increases; volume of reflux can be also calculated. Patency of venous system is checked by inflation and deflation of the additional cuff placed over patient’s thigh. During this examination, volume of distal part of leg increases (while the femoral cuff is inflated), and should rapidly decrease to the baseline after the femoral cuff is deflated. Prolonged return of leg’s volume to the baseline indicates venous occlusion (there are some additional tests to distinguish superficial from deep obstructions). To assess the calf muscle pump function, after the calibration of the set, patient is asked to perform some plantar flexion of the foot (tip-toe maneuvers in the upright position). In our protocol, this examination is performed in supine and upright position. During flexions of calf muscles, the blood is ejected from deep veins of the calf, thus resulting in decrease of volume of the examined leg. As the volume of leg decreases, the pressure of air in the plethysmographic cuff also goes down. These changes are recorded as a curve, and so can be measured and evaluated. The calf muscle pump was regarded as abnormal if the drop of pressure in cuffs was lower than 1 mmHg, which corresponded to approximately 20 ml of ejected blood (fig. 1-3). This value has been found to be physiological in examinations performed in healthy subjects. Presence of venous reflux does not interfere with the assessment of muscle pump. But it should be underlined, that volumes of lower leg decrease during described maneuvers only on condition that blood is expelled proximally. In some cases however, though the blood is ejected from deep veins of lower leg, it is not propelled proximally. This is due – either to profound varicosities (in these cases blood is ejected mainly to the dilated superficial veins – so, the overall volume of the extremity does not change), or to obstruction of main venous trunks (in these cases the volume of the leg can even increase). All these additional pathologies which compromise the function of muscle pump can be easier found if the examination is performed in supine position. But it seems reasonable to perform the examination in both positions (supine and upright), as the function is assessed in two different conditions, corresponding to the daily activity of the patient – when the veins are not dilated and the rest pressure is low (supine), and when veins are dilated and the rest pressure is high (upright). Therefore the method of evaluation of calf muscle pump described in this paper does not assess “pure” function of the pump (as it is done in foot volumetry), irrespective of other components of the system, but rather it helps answering the question – if the volume and pressure in venous system of lower leg decrease during the active contractions of calf muscles, and movements in the ankle joint. This, from pathophysiological point of view seems to be even more important than intact anatomical structures of muscles and skeleton. In this study Smartdop-20EX detector (Hadeco, Japan) with air-plethysmographic probe PV-20 was used. It should be emphasized that examination protocol of our plethysmographic set differs from most often described in medical papers air-plethysmography performed by means of American set (APG-1000C; ACI Medical Inc, USA).1,2
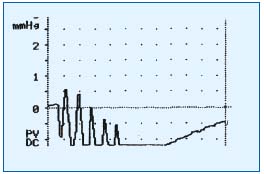
Figure 1. Normal function of calf muscle pump: drop of pressure
below the baseline.
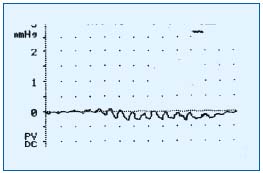
Figure 2. Failure of muscle pump: virtually no blood is expelled
during plantar flexion of the foot.
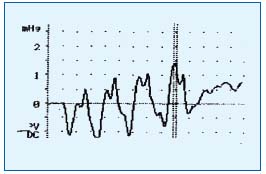
Figure 3. Volume of the leg increases during plantar flexions of the
foot due to coexisting obstruction of popliteal vein.
RESULTS
Insufficiency of the calf muscle pump in the supine position was found in 49% of legs, and in 38% of legs in the standing position. In 24.5% of legs, there was impaired muscle pump in both the supine and the standing position. Moreover, there was pathological outflow in the occlusion test in 73% of extremities, and pathological reflux was revealed in 63% of cases. Insufficiency of all three components (patency, lack of reflux, and normal pumping) was found in 34% of extremities. An insufficient calf muscle pump was the only significant venous abnormality in 18% of cases. It was also found that failure of the calf muscle pump was present more often in older patients (Figure 4); ulcerations in legs with a compromised pump were larger (Figure 5).
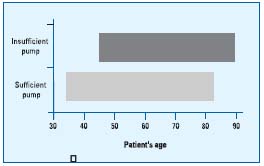
Figure 4. Patients’ age and calf muscle pump.
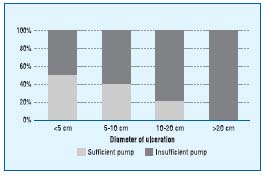
Figure 5. Percentage of patients with sufficient and insufficient calf
muscle pump in terms of ulcer diameter.
Presence of an abnormal pump correlated with poorer results of treatment of venous ulcers. Failure of the pump was found more often in patients who began the specialized care after a long period of unsuccessful home treatment (Figure 6), and the healing time in specialized leg ulcer clinic was prolonged in the legs with insufficient pumps (Figure 7).
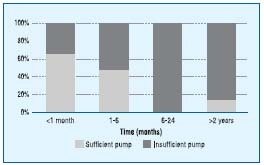
Figure 6. Percentage of patients with sufficient or insufficient calf
muscle pump in terms of time from the opening of the ulcer to the
beginning of specialized care.
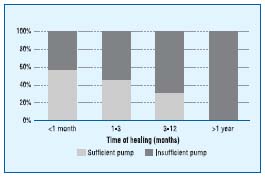
Figure 7. Percentage of patients with sufficient and insufficient calf
muscle pump in terms of time of healing of the ulceration in the
specialized leg ulcer clinic.
DISCUSSION
A thorough evaluation of the patient with chronic venous insufficiency should include clinical (physical examination and history), anatomic (phlebography, color Doppler sonography), and functional (eg, plethysmography) assessment. Though the majority of patients do not require full evaluation, complicated cases with profound disability often require extensive assessment of the abnormality, also by means of functional testing. There are some functional tests of the venous system of the leg: photoplethysmography, air plethysmography, and assessment of valve closure time. Photoplethysmography is widely used; however, its clinical relevance has been shown to be limited. This examination cannot be performed in the presence of ulceration or profound skin induration and hyperpigmentation. Photoplethysmography only measures blood stasis in dermal vessels, and can only assess main veins indirectly. Doppler sonographic valve closure time measurement can only be done locally, and the assessment of the global venous function is not possible. Air or strain-gauge plethysmography can assess this function; however, this examination is not widely used, and the procedure is not yet standardized. Air plethysmography seems to be the most promising procedure. In this examination obstruction, reflux, and calf muscle pump can be quantified.3-5
It was reported in several papers that failure of the calf muscle pump interferes with healing of venous ulcers. Araki6 found that patients with active leg ulcer revealed more profound dysfunction of the calf muscle pump (investigated by means of air plethysmography) in comparison with patients with healed ulcers or with signs of severe chronic venous insufficiency, but without ulceration (CEAP-4). As it is rather improbable for the muscle pump to improve significantly after the ulcer has been healed, he hypothesized that it was associated with the fact that patients with more compromised calf muscle pump have a lower possibility of healing of the ulcer. In our patients, it was also revealed that insufficiency of the calf muscle pump was associated with prolonged time to healing, and the failure of muscle pump was more often seen in patients who began specialized treatment (probably those with correct functioning of muscle pump could heal their ulcers using home treatment only).
Failure of the calf muscle pump in some patients is related to decreased mobility of the ankle joint due to painful ulceration in this area. In these patients, the failure can be reversible. Moreover, insufficiency of the calf muscle pump mainly in the supine position can be related not only to muscular and articular disorders, but also to other problems, eg, stiffness of venous wall or even obstruction associated with previous venous thrombosis. Probably, the higher incidence of muscle pump insufficiency in the supine position in our patients could be explained by this phenomenon.
However, in longstanding ulcers, the patient’s walking pattern changes from the light standing on toes to hard, “duck-like” standing on heels. This results in permanent slight flexion of knees and ankle joints leading to focal overloading of joint cartilages and ligaments, finally resulting in ankle joint stiffness and varus deformation of the knee joint. After the contraction of the ankle joint, leading to a nonfunctioning calf muscle pump, so-called arthrogenic congestive syndrome develops.7 In these cases venous ambulatory hypertension cannot be managed with routine compression therapy only. If the chronic abnormality has led to stiffening of ankle joint, muscular atrophy of the lower leg, and atrophic changes in the articular capsule, qualified (and costly) physiotherapeutic care seems to be unavoidable. Therefore, it seems reasonable to institute exercise programs as well as appropriate compression therapy early in patients with insufficiency of the calf muscle pump.8 These however can be done only if failure of the calf muscle pump is diagnosed on plethysmographic examination.
CONCLUSIONS
Insufficiency of the calf muscle pump is the common cause of profound chronic venous insufficiency. Results of treatment of venous leg ulcers in patients with calf muscle pump failure revealed in the air-plethysmography are worse if compared with those with sufficient pump. Perhaps, routine plethysmographic assessment could predict patients with poor prognosis for proper healing of the ulceration.
REFERENCES
2. Bundens WP. Use of the air plethysmograph in the evaluation and treatment of patients with venous stasis disease. Dermatol Surg. 1995;21:67-69.
3. Haenen JH, Janssen MC, Wollersheim H, et al. The development of postthrombotic syndrome in relationship to venous reflux and calf muscle pump dysfunction at 2 years after the onset of deep venous thrombosis. J Vasc Surg. 2002;35:1184-1189.
4. Illing KA, Shortell CK, Ouri el K, et al. Photoplethysmography and calf muscle pump function after subfascial endoscopic perforator ligation. J Vasc Surg. 1999;30:1067-1076.
5. Tierney S, Burke P, Fitzgerald P, et al. Ankle fracture is associated with prolonged venous dysfunction. Br J Surg. 1993;80:36-38.
6. Araki CT, Back TL, Panberg FT, et al. The significance of calf muscle pump function in venous ulceration. J Vasc Surg. 1994;20:872-879.
7. Juenger M, Steins A, Klyscz T, et al. Physikalische Therapie bei Venenerkranken. Vasa. 1998;27:73-79.
8. Struckmann JR, Christensen SJ, Lendorf A, et al. Venous muscle pump improvement by low compression elastic stockings. Phlebology. 1986;1:97-103.
