Combination of transdermal laser and sclerotherapy in treating reticular veins: an evidence-based approach to modern phlebology
Anelise Rodrigues, MD
Clinica Dra Anelise Rodrigues, Cuiaba, MT, Brazil
ABSTRACT
Chronic venous disease is a widespread condition, with telangiectasias and reticular veins (C1 disease according to the CEAP classification) among its most frequent and cosmetically concerning early manifestations. Whereas sclerotherapy remains the gold standard for their treatment, newer approaches have emerged aiming to optimize results and reduce complications. Among them, the combination of transdermal long-pulsed 1064-nm Nd:YAG laser with sclerotherapy has gained growing attention, particularly in the form of the cryo-laser cryo-sclerotherapy (CLaCS) technique, which merges laser-induced vessel damage with sclerotherapy, enhanced by cryo-cooling and augmented reality guidance. Additionally, the sequential use of transdermal laser following foam sclerotherapy has also shown clinical value in improving outcomes.
Evidence from randomized trials and long-term follow-up cases points to higher clearance rates, better aesthetic outcomes, and fewer adverse effects when laser and sclerotherapy are used in tandem. The evolving literature, supported by international guideline mentions, reflects increasing clinical acceptance of these multimodal strategies.
Drawing from both personal clinical experience and recent studies, this review takes a closer look at the growing evidence behind CLaCS and other laser-sclerotherapy combinations, exploring their mechanisms, clinical data, and practical advantages as a patient-centered evolution in phlebology, offering effective minimally invasive solutions that align with what today’s patients are really looking for.
Introduction
Chronic venous disease (CVD) includes a broad spectrum of vascular conditions affecting millions worldwide. Reticular veins, bluish subdermal vessels between 1–3 mm in diameter, often coexist with telangiectasias and feed superficial venous networks. Although often perceived as cosmetic, these conditions may significantly impact a patient’s quality of life, and their aesthetic prominence often motivates treatment, demanding effective, low-risk interventions.1,2 The prevalence of CVD is increasing, with lifestyle factors such as prolonged standing or sitting, obesity, and lack of physical activity contributing to its development, making patient education and awareness vital components of management strategies.
Sclerotherapy—liquid or foam—remains the gold standard for treating reticular veins.3-5 Though effective, it is not without drawbacks, especially with foam: the risk of postsclerotherapy hyperpigmentation (PSH), session volume limitations, variable results depending on vein size and operator experience, and reports of major systemic complications. Additionally, patients may experience discomfort during the procedure and require multiple sessions to achieve optimal results.6,7 Microphlebectomy also yields satisfactory results but requires surgical expertise and, though minimally invasive, involves a longer downtime and is not free from the risk of scarring, which makes it not suitable for some patients.8
Over the past few years, transdermal laser therapy has become a significant adjunct, which can enhance treatment efficacy and cosmetic results, when associated with sclerosing agents. This hybrid approach provides a treatment option with a lower risk of complications and quicker recovery times. Laser precise treatment of reticular veins gives better patient satisfaction and results. As research continues, the combination of laser therapy and traditional treatments shows great potential for the development of new and improved treatments of reticular veins.
Evolving use of transdermal lasers
The concept of transdermal lasers for vascular medicine focused initially on the treatment of port-wine stains and has expanded to include conditions such as telangiectasias and reticular veins. Initial clinical observations showed that the long-pulsed (LP) 1064-nm Nd:YAG (neodymium:yttrium-aluminum-garnet) laser was successful in treating deeper vascular lesions, for its wavelength allows deeper penetration at the same time that it targets deoxyhemoglobin (principles of selective photothermolysis), but risks were also identified. Bruising, edema, blistering, and scarring were the most reported complications and have been primarily attributed to the high-energy settings necessary for optimal treatment, particularly in the absence of adjunctive cooling mechanisms designed to reduce epidermal damage.9,10
With the development of dynamic cooling devices such as contact coolers and cold air blowing equipment, it became easier to preserve the epidermis and lower the incidence of thermal-related adverse effects, increasing the range of those who can benefit from this kind of treatment. Also, as the cold can cause numbing of the skin, it significantly improves patients’ comfort during the treatment.11,12 These continued innovations in laser technology emphasize the importance of both efficacy and safety when searching for ideal treatment of vascular lesions.
Despite technology’s constant development, it was noted that the results for laser treatment of reticular veins were not consistent and were sometimes unsafe. As the quest to treat reticular veins with laser alone was met with limited success, the stage was set for techniques like cryo-laser cryo-sclerotherapy (CLaCS), in which the laser is not a standalone, but a partner to enhance the action of sclerosant, promoting synergic thermal and chemical treatment effects, thus redefining the role of transdermal lasers in vein treatment: from replacement to enhancement.
Synergistic approach: laser plus sclerotherapy
Recognition that lasers alone could not consistently or safely treat reticular veins led to hybrid approaches. Transdermal laser therapy used in combination with sclerosing agents provided higher efficacy and cosmetic outcomes, while offering reduced risk of complications and quicker recovery times.
The CLaCS method was born in Brazil, developed by Dr Kasuo Miyake and his team at Miyake Clinic. The approach was innovative—using low-energy LP 1064-nm Nd:YAG laser pulses followed by small-volume injections of 75% dextrose (a mild osmotic sclerosant agent), all performed under continuous cryotherapy. In 2003, the technical foundation of CLaCS and their 1-year follow-up were presented in a Joint International Laser Conference in Edinburgh, confirming that the approach offered long-lasting cosmetic results with fewer complications compared with monotherapy. In 2019, the white paper describing the details of the technique was published.13 The laser parameters, typically a 6-mm spot size, 15-ms pulse, and 50–70 J/cm² fluence, were carefully selected to achieve the perfect balance between depth and safety. Cryo-cooling made it possible to deliver enough energy to target the vein wall while protecting the skin from burns. The goal: improve cosmetic results while minimizing complications.
The sequence used in CLaCS (Figure 1) allows the laser to promote thermal lesion and edema of the vein wall, causing immediate vasospasm and partial collapse of the vessel. The smaller internal diameter of the vessel then prolongs the contact time of the sclerosant with the endothelium— enhancing its effect even at lower doses. This dual action leads to efficient closure with fewer side effects like pigmentation or inflammation.
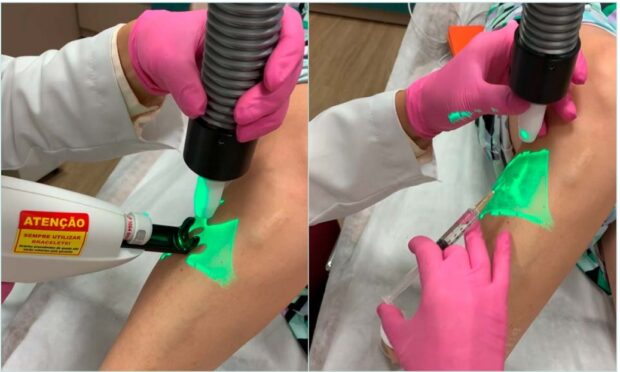
Figure 1. Cryo-laser cryo-sclerotherapy (CLaCS) sequence.
• Skin cooling (- 20 ºC cold air)
• Nd:YAG 1064 LP
• 50-70 J/cm2 – Spot size 6 mm / 15-ms pulse duration / 1-2 shots / 5 mm
• Dextrose 75% injection
• Blood stop with cotton balls and tape
The photo documentation of treatment progress is a steppingstone in CLaCS, and its importance has been reinforced by a 2018 publication that showed the shift of patients’ perception of cosmetic outcomes after being shown before and after pictures (Figure 2). 14
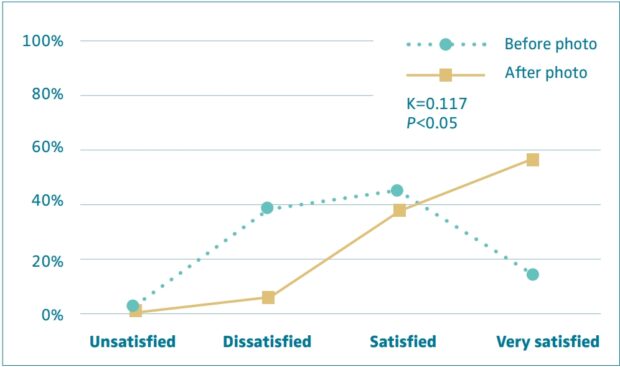
Figure 2. Patients’ satisfaction before and after viewing a photograph at the 2-month
follow-up. After reference 14: Santiago et al. Phlebology. 2018;33(4):282-287. © 2017, The Author(s).
The addition of augmented reality devices, such as VeinViewer, allowed more precise targeting of feeder veins, further refining the technique. In fact, the development of this technology was itself linked to the evolution of CLaCS. In 2006, Miyake and colleagues introduced a novel near-infrared imaging system that projects real-time processed images of subdermal veins directly onto the patient’s skin. At that time, the device was proven to easily show veins that were too deep for the naked eye and too shallow for ultrasound detection.15 By allowing both laser application and sclerosant injections to be guided in real time, without the device being put in direct contact with the skin, this technology helped transform CLaCS into a more controlled and anatomically precise method.
As clinical experience expanded, so did scientific support. In 2012, Moreno-Moraga and colleagues demonstrated that combining polidocanol with repeated low-fluence laser pulses provided superior results, reducing the risk of pigmentary changes in Fitzpatrick IV patients, who are known to be more prone to postsclerotherapy pigmentation due to increased melanocyte activity.16 Two years later, a large randomized trial by the same group involving 517 legs confirmed that Nd:YAG laser used after foam sclerotherapy significantly improved long-term clearance.17 The sequence here is different from CLaCS, as the laser is applied after the sclerosant. The reasons for success of this approach aren’t totally understood yet, but the fact that the foam enhances the light scattering in the tissue and then the beam absorption becomes larger18 plays an important role in it.
Cryotherapy became especially valuable for patients with higher Fitzpatrick skin types.12 Later insights from Miyake’s team emphasized that cryo-cooling enhanced thermal selectivity and procedural safety, supporting the method’s broader application in diverse patient populations.
Recognizing the growing interest and supporting evidence, a 2020 publication laid out the state-of-the-art on CLaCS. This expert summary contextualized the technique as a major advancement in venous treatment and highlighted its efficacy for reticular veins and telangiectasias, especially in patients seeking less invasive and low-risk procedures, with high aesthetic payoff. It also upholds the importance of standardizing laser parameters, sclerosant concentration, cryotherapy settings, and imaging tools, advocating for a reproducible and globally adoptable approach.19
In 2023, a triple-blind randomized clinical trial added to that evidence comparing 2 sclerosants—75% dextrose and 0.3% polidocanol diluted in dextrose—under the same CLaCS protocol. Both agents were effective, but lower posttreatment pain and slightly better clearance at augmented reality analysis were achieved with polidocanol diluted in dextrose. The findings highlight the flexibility of the method, with both agents performing well under controlled, standardized conditions.20
That same year, the long-term promise of CLaCS was confirmed in a case report from Miyake et al, detailing an 11-year follow-up of a patient treated with augmented reality– guided CLaCS. The results were sustained vein clearance, minimal recurrence, and high satisfaction, supporting the technique’s durability and the added value of image-guided precision.21
In 2024, a randomized controlled trial compared CLaCS against foam sclerotherapy alone. In this trial, CLaCS achieved complete clearance in 100% of treated limbs versus 85.3% in the foam group, with significantly fewer pigmentation events (36.9% vs 78.7%), further solidifying the method’s safety and aesthetic outcomes.22
A recent case report introduced the “Cryo Laser after Foam” (CLAF) technique,23 expanding the scope of combination therapy to include larger-caliber reticular veins. In this approach, foam sclerotherapy with polidocanol is also administered first, followed by immediate application of 1064-nm Nd:YAG laser along the same vein pathway, all under continuous cold air cooling, targeting veins greater than 2.5 mm—and up to 5 mm in diameter. The reported patient had excellent clearance of the targeted reticular varicosities with good cosmetic results. The authors note that combining modalities helped mitigate common sclerotherapy side effects like hyperpigmentation and matting. This single-case experience aligns with emerging evidence that foam plus laser in one session can improve efficacy and minimize side effects, particularly in blue reticular veins that often show suboptimal response to monotherapy.
Guidelines and future directions
In the past few years, scientific validation has aligned with clinical enthusiasm regarding the combination of transdermal lasers and sclerotherapy for treating reticular veins and telangiectasias, with a growing body of studies supporting the efficacy and safety of this multimodal approach, particularly CLaCS, and International Guidelines have started to acknowledge the potential of this association in managing superficial venous disorders.
The European Society for Vascular Surgery (ESVS) 2022 Clinical Practice Guidelines3 state that “Cryo-Laser Cryo-Sclerotherapy guided by augmented reality (CLaCS) is a new option for treating telangiectasias, reticular and feeder veins, with promising results, although more studies are required.”
Additionally, the same guidelines highlight that “combining 1064 nm Nd:YAG long-pulse laser with foam sclerotherapy has demonstrated improved efficacy over foam sclerotherapy alone. Specifically, studies have shown that this combination leads to better clearance rates and sustained results over time.” This inclusion reflects the growing recognition of CLaCS and other combined treatments as valid alternatives for the aesthetic and functional management of superficial venous conditions. This multimodal approach aligns with patient expectations for faster, more complete results, with fewer complications.
The 2020 update to the CEAP (Clinical-Etiology-Anatomy-Pathophysiology)24 classification system further encourages standardized assessment of venous disease classification in clinical trials of new techniques, enhancing the system’s precision and applicability in research and clinical practice.
The demand for evidence-based, efficient, and cosmetically favorable outcomes makes it likely that these hybrid techniques will continue to gain prominence in clinical practice.
A bit of my own perspective
Having incorporated the LP 1064-nm Nd:YAG transdermal laser into my practice in 2011—initially as a cosmetic touch-up tool for treating small telangiectasias, after reticular veins sclerotherapy or phlebectomy—it was not until 2017 that I began performing the full CLaCS technique.
The most striking difference I observe with combined techniques is the consistent delivery of faster and more refined results, with significantly fewer sessions required. Figure 3 illustrates an example of a patient that underwent a single session of CLaCS, before and 3 months after treatment.
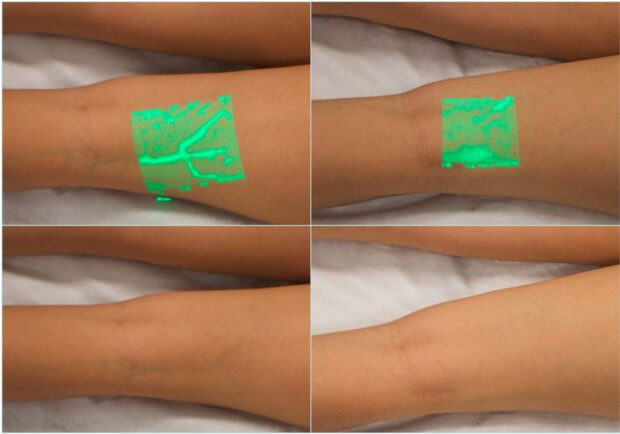
Figure 3. Example of a patient that underwent a single session of cryo-laser cryo-sclerotherapy (CLaCS), before and 3 months after treatment.
Also, there is no surgical downtime and, notably, much less pigmentation in patients with darker skin types. Even when treating larger veins with foam, the contrast in outcomes between using foam alone and combining it with laser is easy to spot.
I am often asked—or even challenged—about whether lasers are necessary, with colleagues arguing that excellent results can be achieved without them. I agree that traditional approaches like sclerotherapy and microsurgery can yield solid outcomes, and I understand how difficult it may be to move away from familiar methods, even when alternative techniques begin to show clearer benefits. Still, it is impossible to overlook both the technological progress and the increasing volume of data showing that combining transdermal lasers with sclerotherapy consistently leads to fewer complications, especially when it comes to cosmetic results.
The doubts about whether to incorporate (or not) laser therapy in one’s practice tend to appear mostly when we get to the subject of the initial investment and how to return it. These novel techniques involve technology—laser equipment, cooling devices, illuminating devices and so on— and they all have a cost to be taken into consideration. That is the main reason hybrid approaches often find their place in private practice settings. When the decision is made wisely, respecting the physician’s professional and financial moment, it is very unlikely that one will later refrain from using it. On the contrary, enthusiasm will probably grow with experience and with supporting literature continuously expanding.
Considering time is by far one of our most valuable assets nowadays, treatments that offer faster outcomes, fewer clinic visits, and minimal downtime—while also reducing complications—represent a true competitive edge. Patients recognize this, and they are willing to pay for it.
Professor Kasuo Miyake, from whom I learned the CLaCS technique back in 2017, used to say to us: “CLaCS: Present is telling. Future will give the evidence.” And as evidence keeps building, what was once considered an innovation surrounded by skepticism is steadily redefining what we now expect from reticular vein treatment.
Conclusions
By combining the effects of transdermal laser, sclerotherapy, and the protective effects of skin cooling, these hybrid techniques offer a comprehensive solution tailored to modern phlebology. Providing enhanced effectiveness while minimizing adverse effects, they represent a significant evolution in the treatment of reticular and telangiectatic veins, particularly for patients seeking better aesthetic outcomes with fewer sessions and less complications. Allied with continued research and refining, they are already transforming venous disease management.
While formal recommendations remain conditional and pending further high-quality evidence, the accumulation of positive clinical outcomes is shaping the perception of laser-assisted sclerotherapy as a practical, effective, and viable alternative to traditional sclerotherapy methods, particularly in cases where standard sclerotherapy may fall short.
The question is no longer whether to choose between laser and sclerotherapy—but how best to use them together for safer, more effective, and longer-lasting results.
CORRESPONDING AUTHOR
Anelise Rodrigues, MD
Anelise Rodrigues Bezerra dos Santos, Av Andre Antonio Maggi, 487 – Centro Politico Administrativo, Cuiaba – MT, 78.049-080
e-mail: contato@draanelise.med.br
References
1. Spinedi L, Uthoff H, Partovi S, Staub D. Varicosities of the lower extremity, new approaches: cosmetic or therapeutic needs? Swiss Med Wkly. 2016;146:w14360.
2. Onida S, Davies AH. Predicted burden of venous disease. Phlebology. 2016;31(1_ suppl):74-79.
3. De Maeseneer MG, Kakkos SK, Aherne T, et al. Editor’s Choice – European Society for Vascular Surgery (ESVS) 2022 clinical practice guidelines on the management of chronic venous disease of the lower limbs. Eur J Vasc Endovasc Surg. 2022;63(2):184-267.
4. Tan M, Moreno HB, Bechter-Hugl B, et al. Sclerotherapy: indications and safety volumes. Phlebology. 2024;39(2):135- 138.
5. Gloviczki P, Lawrence PF, Wasan SM, et al. The 2023 Society for Vascular Surgery, American Venous Forum, and American Vein and Lymphatic Society clinical practice guidelines for the management of varicose veins of the lower extremities. Part II: Endorsed by the Society of Interventional Radiology and the Society for Vascular Medicine. J Vasc Surg Venous Lymphat Disord. 2024;12(1):101670.
6. Jia X, Mowatt G, Burr JM, Cassar K, Cook J, Fraser C. Systematic review of foam sclerotherapy for varicose veins. Br J Surg. 2007;94(8):925-936.
7. Bossart S, Daneluzzi C, Cazzaniga S, et al. Skin hyperpigmentation after sclerotherapy with polidocanol: a systematic review. J Eur Acad Dermatol Venereol. 2023;37(2):274-283.
8. Scotti CM, Shing M, Comerota AJ. Microphlebectomy of varicose veins: a review of techniques, outcomes, and complications. J Vasc Surg. 2012;55(3):849-856.
9. Groot D, Rao J, Johnston P, Nakatsui T. Algorithm for using a long-pulsed Nd:YAG laser in the treatment of deep cutaneous vascular lesions. Dermatol Surg. 2003;29(1):35-42.
10. Ross EV, Domankevitz Y. Laser treatment of leg veins: physical mechanisms and theoretical considerations. Lasers Surg Med. 2005;36(2):105-116.
11. Chang CJ, Nelson JS. Cryogen spray cooling and higher fluence pulsed dye laser treatment improve port-wine stain clearance while minimizing epidermal damage. Dermatol Surg. 1999;25(10):767-772.
12. Das A, Sarda A, De A. Cooling devices in laser therapy. J Cutan Aesthet Surg. 2016;9(4):215-219.
13. Miyake K, Ramacciotti E. Cryo-laser and cryo-sclerotherapy guided by augmented reality for telangiectasias, feeder, and small varicose vein treatment – The CLaCS technique white paper report. J Phlebol Lymphol. 2019;12(1):1-7.
14. Santiago FR, Piscoya M, Chi YW. Change in perception of sclerotherapy results after exposure to pre-post intervention photographs. Phlebology. 2018;33(4):282-287.
15. Miyake RK, Zeman HD, Duarte FH, et al. Vein imaging: a new method of near infrared imaging, where a processed image is projected onto the skin for the enhancement of vein treatment. Dermatol Surg. 2006;32(8):1031-1038.
16. Moreno-Moraga J, Hernández E, Royo J, et al. Optimal and safe treatment of spider leg veins measuring less than 1.5 mm on skin type IV patients, using repeated low-fluence Nd:YAG laser pulses after polidocanol injection. Lasers Med Sci. 2012;28(3):925-933.
17. Moreno-Moraga J, Smarandache A, Pascu ML, Royo J, Trelles MA. 1064 nm Nd:YAG long pulse laser after polidocanol microfoam injection dramatically improves the result of leg vein treatment: a randomized controlled trial on 517 legs with a three-year follow-up. Phlebology. 2014;29(10):658-666.
18. Smarandache A. Laser beams interaction with polidocanol foam: molecular background. Photomed Laser Surg. 2012;30(5):262-267.
19. Miyake RK, Chi YW, Franklin IJ, Gianesini S. State of the art on cryo-laser cryo-sclerotherapy in lower limb venous aesthetic treatment. J Vasc Surg Venous Lymphat Disord. 2020;8(5):893-895.
20. Fonseca MM, Mocelin FJ, Grill MH, et al. Nd:Yag laser combined with injection sclerotherapy in the treatment of reticular veins and telangiectasias (CLaCS Method): a triple-blind randomized clinical trial comparing two sclerosing agents associated with same laser patterns. Phlebology. 2023;38(3):165-171.
21. Miyake K, Grill MH, Feitoza HSN. Case report: novel leg vein treatment CLaCS guided by augmented reality 11years follow-up. J Cosmet Dermatol. 2023;22(Suppl 2):16–20.
22. Nasser M, Ghoneim B, Eldaly W, Elmahdy H. A Comparative Study Between Cryo-Laser Cryo-Sclerotherapy and Sclerotherapy in the Treatment of Telangiectasia and Reticular Veins: a randomized controlled trial. J Vasc Surg Venous Lymphat Disord. 2024;12(4):101874.
23. Fonseca MM, Mocelin FJ, Poltronieri LR, Guimaraes Filho JL. Treatment of varicose veins using the Cryo laser after foam technique. J Vasc Surg Cases Innov Tech. 2024;10(4):101549.
24. Lurie F, Passman M, Meisner M, et al. The 2020 update of the CEAP classification system and reporting standards. J Vasc Surg Venous Lymphat Disord. 2020;8(3):342-352.

