A retrospective study of 100 patients with varicose veins treated with radiofrequency ablation and stripping
Stoyan G. Genadiev,
Svetoslav G. Dimitrov,
Todor T. Zahariev,
Gencho K. Nachev
“St. Ekaterina” University Hospital
Sofia, Bulgaria
ABSTRACT
The management of varicose veins has changed rapidly in recent years. Saphenofemoral ligation and stripping of the great saphenous vein (GSV), which once used to be the standard treatment for GSV reflux, has been challenged–and in some areas replaced–by endovenous therapies. We retrospectively analyzed the records of 100 consecutive patients with chronic saphenofemoral insufficiency. Between 2009 and 2011, 50 patients underwent endovenous ablation using radiofrequency with ClosureFAST™ catheter (Group 1) and 50 underwent classic stripping of the GSV (Group 2). In both groups, phlebectomies with microincisions of varicose veins below the knee were performed simultaneously with the selected procedure. The present study shows improved results using the new ClosureFAST™ technique leading to good venous closure with minimal complications and with improved patient comfort. The outcomes with radiofrequency obliteration of saphenous vein reflux were comparable to those of traditional stripping and ligation at 1-year follow up. Radiofrequency ablation is associated with fewer complications and when they do occur they are time limited and usually of minor consequence.
INTRODUCTION
Chronic venous insufficiency of the lower limbs is a common condition afflicting 25% of women and 15% of men, with venous reflux at the saphenofemoral junction (SFJ) being the most common cause leading to varicose veins.1 The management of varicose veins has changed rapidly in recent years. Saphenofemoral ligation and stripping of the great saphenous vein (GSV) was once the standard treatment for GSV reflux, but more recently it has been challenged–and in some areas replaced–by endovenous therapies (EVT).2-5 Over the last decade, technological progress has enabled the development and application of new minimally invasive therapies such as VNUS Closure endovenous radiofrequency ablation (RFA) and endolaser.5-7 In the last 2 years, developments in the technology related to the use of RFA catheters have led to the introduction of the ClosureFAST™catheter. Evidence supports the use of endovenous modalities in terms of reduced postoperative hospital stay, early return to work, and low complication rates.8
PATIENTS AND METHODS
We retrospectively analyzed the records of 100 consecutive patients with chronic saphenofemoral insufficiency. Between 2009 and 2011, a total of 50 patients underwent endovenous ablation using RFA with the ClosureFAST™ catheter (Group 1) and 50 underwent classic stripping of the GSV (Group 2). In both groups, phlebectomies with microincisions of varicose veins below the knee were performed simultaneously with the selected procedure (Figure 1). Follow-up visits performed at 2 weeks, 3 months, and 1 year were also analyzed. All patients had symptomatic varicose veins and the inclusion criteria for the study were based on the clinical, etiological, anatomical, pathophysiological (CEAP) classification. All patients with C1-C5 disease (C1: spider veins, C2: varicose veins, C3: ankle edema, C4: lipodermatosclerosis, and C5: healed ulcer) were included in the study. Patients in C6 stage with active ulcers and those with postthrombotic etiology were excluded. The diagnosis was based on both clinical and color Doppler examination. Patients who demonstrated venous reflux in the long saphenous vein with a duration equal to or more than 0.5 seconds were included in the study. Exclusion criterium for RFA was a GSV diameter of more than 16 mm.
Venous Clinical Severity Score (VCSS) was calculated for each patient. The VCSS scores characteristic features of venous disease on a severity scale from 1 to 3 (mild, moderate, and severe) and the scores are then added to score a maximum of 30.9 The disease characteristics are: pain, varicose veins, venous edema, pigmentation, inflammation, induration, fatigue, cramps, compression use, and overall response. We also looked for and recorded the following complications: hyperpigmentation, thrombophlebitis, saphenous paresthesias, ecchymosis, hematoma, infection, and thermal injury.

Figure 1. Final stage of radiofrequency ablation.
Follow-up clinical and Doppler examinations were performed at 2 weeks, 3 months and 12 months to determine both short- and long-term outcomes, and the final VCSS was determined at 1 year. Any patient with recanalization of a closed vein, recurrent reflux or neovascularization was noted. All patients were advised to take a venoactive drug (micronized purified flavonoid fraction, MPFF*) twice daily for 3 months and to use compression stockings for at least 1 month.
*Registered as: MPFF at a dose of 500 mg, Alvenor®, Ardium®, Arvenum® 500, Capiven®, Detralex®, Elatec®, Flebotropin®, Variton®, Venitol®.
RESULTS
We conducted a retrospective analysis of data from 100 consecutive patients with saphenofemoral junction incompetence who underwent RFA and stripping. Of these patients, 64 (64%) were female and 36 were male (36%) with a mean age of 36.4 ± 9 and 48.3 ± 12 years, respectively. The mean length of the RFA-treated GSV segment was 35 cm (range, 20 to 60 cm).
All patients were symptomatic for their venous problems, with or without skin changes. The majority were in the C2 group of the CEAP classification (26 patients in Group 1 and 22 in Group 2), followed by C3 (20 patients in Group 1 and 18 in Group 2), and C4-C5 (4 patients in Group 1 and 10 in Group 2) (Figure 2). Figure 2 also illustrates the distribution of patients at 1-year follow-up: C0-C1 (42 patients in Group 1 and 41 in Group 2), C2 (5 patients in both Groups), C3 (2 patients in both Groups), and C4-C5 (1 patient in Group 1 and 2 patients in Group 2).
VCSS scores are displayed in Figure 3. The largest number of patients was seen in the moderate group (10-20) with 36 patients from Group 1 and 30 patients from Group 2, followed by the severe group (20-30) with 8 patients from Group 1 and 16 from Group 2, and then the mild group (0-10) with 6 patients from Group 1 and 4 from Group 2. Posttreatment VCSS assessment was performed at 12 months and showed significantly reduced scores: only 4 patients from Group 1 and 8 from Group 2 were in the moderate group, followed by 1 patient from Group 1 and 3 patients from Group 2 in the mild group (Figure 3).
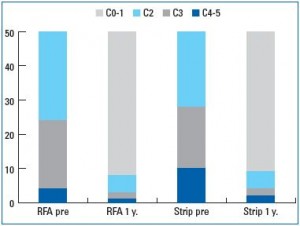
Figure 2. Comparison of clinical CEAP classes distribution in
patients who underwent either radiofrequency (RFA) or stripping
(Strip), before and 1 year after the procedure.
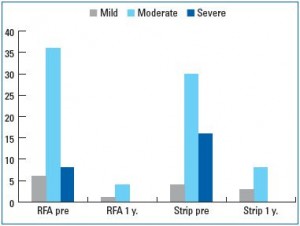
Figure 3. Comparison of VCSS scores in patients who
underwent either radiofrequency (RFA) or stripping (Strip),
before and 1 year after the procedure.
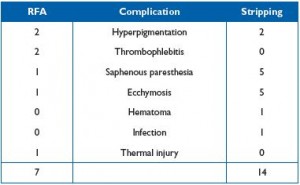
Table I. Distribution of complications in both radiofrequency
ablation (RFA) and stripping groups.
The complications observed at 2 weeks of follow-up are shown in Table I. The most common complications were saphenous paresthesias (1 patient from Group 1 and 5 patients from Group 2), followed by ecchymosis (1 patient from Group 1 and 5 patients from Group 2), hyperpigmentation (2 patients from both Groups), thrombophlebitis in distal varicosities (2 patients from Group 1), hematoma (1 patient from Group 2), and infection of the inguinal-femoral area (1 patient from Group 2). Postprocedural Doppler examinations showed complete vein closure in 100% of patients from Group 1. Reflux-free and vein occlusion rates at 1 year were 100% in Group 1. One patient from Group 2 showed neovascularization and in another patient a de novo reflux was observed in the anterolateral vein, which opened separately into the common femoral vein.
The cumulative rate of recurrence of varicose veins at 1 year was 2% (1 patient) in Group 1 and 4% (2 patients) in Group 2.
DISCUSSION
RFA of the GSV is an alternative treatment option to venous stripping, which can lead to a painful and prolonged postoperative recovery with a high incidence of hematoma formation, nerve injury, and infection.10-12 Early RFA studies used a slow, incremental, catheter pullback technique, which was associated with a higher incidence of clot formation, early vessel recanalization, and thermal injury. The overall reported success in these studies was 83%-100%.13,14 The present analysis reports improved results with good venous closure and minimal complications using the new ClosureFAST™ technique, which has overcome the limitations of previous RFA techniques as well as improving patient comfort. The present technique did not require the use of any postprocedure analgesics with the patient being ambulatory the same day, which is a great advantage for early patient recovery. VCSS results at 2 weeks, 3 months and 1 year also showed a significant reduction in scores thus showing an excellent symptomatic recovery with better results in Group 1.
Nerve damage is one of the most common causes of litigation after varicose vein surgery.15 Paresthesia or numbness may arise following RFA and stripping, but in most cases improves over the course of a few weeks.16 RFA has been shown to cause less pain and bruising than surgery as well as taking less time.17 Our study showed a 2% neovascularization rate in Group 2 and no recanalization in Group 1 at 1-year follow-up. The open surgery technique was associated with a recurrence rate of 4% compared with 2% in Group 1. In comparison, the EVOLVeS trial reported a neovascularization rate of 3% with a conventional closure technique and 17% with stripping.18
Recanalization of a vein may be due to either reflux from a tributary or an incompetent perforator. Similarly, if the main lumen is patent, reflux from the groin due to an accessory vein can also lead to failure and recurrence.19 Technical problems such as difficult access, problems in advancing the catheter, or a tortuous GSV can also all play a role in failure of the procedure or incomplete occlusion of the vein and ultimately result in recurrence.19
Deep vein thrombosis can develop in the deep veins of the calf, or a thrombus can circulate from the treated superficial veins following RFA and stripping. In our study we observed no thrombus formation in the deep venous system. Deep vein thrombosis after endovenous ablation is extremely rare and most case series and trials show no evidence of it.2,20
All patients in Group 1 and 56% of patients in Group 2 returned to normal activities within 1 day of the procedure. This outcome is even better than that observed in the EVOLVeS trial,18 which used the conventional closure technique and where 80% of patients resumed their normal activities 24 hours after the procedure, compared with only 47% after stripping.
CONCLUSION
The results from our series of patients suggest that RFA with the ClosureFAST™ technique is a safe and promising tool for the treatment of saphenofemoral junction insufficiency. Outcomes 1-year after RFA obliteration of saphenous vein reflux were comparable to those of traditional stripping and ligation. When complications did occur they were time limited and usually of minor consequence. The significant advantages of RFA over stripping in this series of patients were less pain, early return to normal activities, fewer days off work, and better cosmetic results and qualityof- life scores. Confirmation of whether RFA deserves to be the treatment of choice should be studied in further randomized trials.
1. Callan MJ. Epidemology of varicose veins. Br J Surg. 1994;81:167-173.
2. Rasmussen LH, Lawaetz M, Bjoern L, Vennits B, Blemings A, Eklof B. Randomized clinical trial comparing endovenous laser ablation, radiofrequency ablation, foam sclerotherapy and surgical stripping for great saphenous varicose veins. Br J Surg. 2011;98:1079-1087.
3. Lane TR, Pandey VA, Davies AH. Superficial venous disease treatment – is there still a role for open surgery in 2011? Acta Chir Belg. 2011;111:125- 129.
4. Chandler JG, Pichot O, Sessa C, Schuller-Petrovicć S, Kabnick LS, Bergan JJ. Treatment of primary venous insufficiency by endovenous saphenous vein obliteration. Vasc Endovascular Surg. 2000:34:201-214.
5. Puggioni A, Kalra M, Carmo M, Mozes G, Gloviczki P. Endovenous laser therapy and radiofrequency ablation of the great saphenous vein: analysis of early efficacy and complications. J Vasc Surg. 2005;42:488-493.
6. Creton D, Pichot O, Sessa C, Proebstle TM; ClosureFast Europe Group. Radiofrequency-powered segmental thermal obliteration carried out with the ClosureFast procedure: results at 1 year. Ann Vasc Surg. 2010;24:360-366.
7. Roth SM. Endovenous radiofrequency ablation of superficial and perforator veins. Surg Clin North Am. 2007;87:1267-1284.
8. Anwar MA, Lane TA, Davies AH, Franklin IJ. Complications of radiofrequency ablation of varicose veins. Phlebology. 2012;27(suppl 1):34- 39.
9. Vasquez MA, Wang J, Mahathanaruk M, Buczkowski G, Sprehe E, Dosluoglu HH. The utility of the Venous Clinical Severity Score in 682 limbs treated by radiofrequency saphenous vein ablation. J Vasc Surg. 2007;45:1008- 1014.
10. Dietzek AM. Endovenous radiofrquencly ablation for treatment of varicose veins. Vascular. 2007;15:255-261.
11. Leopardi D, Hoggan BL, Fitridge RA, Woodruff PW, Maddern GJ. Systematic review of treatments for varicose veins. Ann Vasc Surg. 2009;23:264-276.
12. Merchant RF. Radiofrequency ablation of the incompetent saphenous vein – lessons learned. Phlebolymphology. 2009;16:237-245.
13. Merchant RF, Pichot O. Endovenous radiofrequency ablation of superficial and perforator veins. Vasc Surg. 2005;42:502-509.
14. Brown DB. Concepts, considerations, and concerns on the cutting edge of radiofrequency ablation. J Vasc Interv Radiol. 2005;16:597-613.
15. Markides GA, Subar D, Al-Khaffaf H. Litigation claims in vascular surgery in the United Kingdom’s NHS. Eur J Vasc Endovasc Surg. 2008;36:452-457.
16. Gandhi A, Froghi F, Shepherd AC, et al. A study of patient satisfaction following endothermal ablation for varicose veins. J Vasc Endovasc Surg. 2010;44:274-278.
17. Rautio T, Ohinmaa A, Perälä J. Endovenous obliteration versus conventional stripping operation in the treatment of primary varicose veins: a randomized controlled trial with comparison of the costs. J Vasc Surg. 2002;35:958-965.
18. Lurie F, Creton D, Elkof B, et al. Prospective randomised study of endovenous radiofrequency obliteration (Closure procedure) versus ligation and stripping in a selected population (EVOLVeS study). J Vas Surg. 2003;38:207-214.
19. Lohr J, Kulwicki A. Radiofrequency ablation: evolution of a treatment. Semin Vasc Surg. 2010;23:90-100.
20. Proebstle TM, Alm J, Göckeritz O, et al; European Closure Fast Clinical Study Group. Three-year European followup of endovenous radiofrequencypowered segmental thermal ablation of the great saphenous vein with or without treatment of calf varicosities. J Vasc Surg. 2011;54:146-152.
21. Rasmussen LH, Lawaetz M, Bjoern L, et al. Randomized clinical trial comparing endovenous laser ablation, radiofrequency ablation, foam sclerotherapy and surgical stripping for great saphenous varicose veins. Br J Surg. 2011;98:1079-87.
