Chronic venous disease is highly prevalent in hospital employees
Medical University of Vienna,
Austria
SUMMARY
Chronic venous diseases (CVD) comprise primary/idiopathic abnormalities of the venous system and secondary sequels after deep venous thrombosis. Known risk factors include endogenous and environmental parameters. The aim of the present study was to prove the hypothesis that the development of CVD might also be triggered by occupation-related risk factors. We determined the prevalence and social relationship of CVD in a wide cross-section of a total of 209 hospital employees, including doctors, nurses, medical technicians, secretaries, scientific staff, cleaners, and general staff, all without predocumented CVD. In addition, the restriction in quality of life due to symptoms of CVD was evaluated. CVD was classified according to the CEAP classification and was present in 34% of all employees, predominantly in females. The highest prevalence of CVD was found in general staff and cleaners, and the lowest in medical technicians, secretaries, and scientific workers. Standing at work was a predisposing factor. It can be concluded that within the workforce of a large hospital, females, who are working in a standing position or under hot-humid conditions, are at particular risk for the development of CVD, and should therefore consider to undergo primary prophylactic treatment of CVD.
INTRODUCTION
Chronic venous disease (CVD) of the lower extremities is of multifactorial etiology,1-4 including primary risk factors, such as genetic predisposition, gender, obesity,5-10 and secondary possible risk factors, such as dietary habits, use of contraceptives, or hormone replacement therapy, but also workplace conditions of certain professions, such as poor mobility, orthostasis, load-carrying, and/or hot-humid temperatures.10-17 Every 6th man and every 5th woman are suffering from chronic venous insufficiency. The prevalence of crural ulcers is 0.7%.18 All reports consistently describe a positive correlation between presence of CVD and increased age.19 CVD results from venous hypertension caused by venous valve insufficiency, and is characterized by clinical signs or symptoms, such as swelling, skin changes, and ulceration in its most severe form.20 Figure 1a-c shows lower extremities of patients, suffering from various severity degrees of CVD. Patients are subjectively affected in their quality of life due to leg tiredness, heaviness, aching, cramps, itching, and also the restless leg syndrome. A large step forward in research into CVD was the presentation of the so-called CEAP classification which addresses the clinical (C), etiological (E), anatomic (A) and pathophysiological (P) mechanisms of CVD21-23 (Table I). This accurate classification scheme concerning the pathophysiology and anatomic distribution of the disease is the basis for an optimal treatment, and serves as a basis for scientific studies comparing different treatment regimens.
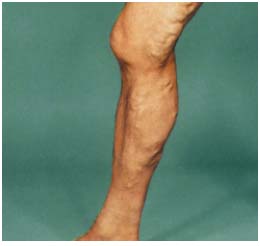
Figure 1a: lower extremity of a patient, suffering from CVD, C2.

Figure 1b: lower extremity of a patient, suffering from CVD, C3.

Figure 1c: lower extremity of a patient, suffering from CVD, C4.
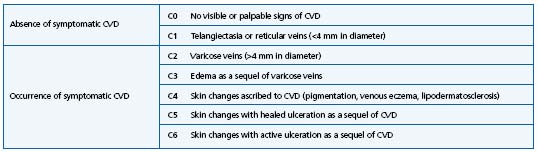
Table I. Clinical part of the CEAP classification.
The aim of the present study was to determine the prevalence of CVD in a cross-section of the workforce population of a hospital, and to investigate possible correlations between endogenous, environmental, and occupational risk factors for CVD and the occurrence of this disease.24,25 As the field of activity of most hospital employees differs from that of other professions, because of certain conditions, such as long standing periods, working night shifts, or hot-humid workplace temperatures, we tested the hypothesis that these workplace conditions might increase the risk of developing CVD.
SUBJECTS AND METHODS
During 6 months all consecutive subjects who consulted the outpatient department of the Department of Occupational Health Medicine of the Medical University of Vienna for routine medical checkups were asked to participate in the investigation. Twenty people refused to participate; finally 209 employees (49 men and 160 women with a mean age of 38 years) were included. None of the participants had recently seen a doctor because of primary complaints related to venous disorders. Three groups were defined: group 1: doctors and nurses (n = 71; 34%), group 2: medical technicians, secretaries, and scientific staff (n = 68; 33%), and group 3: cleaners and general staff (n = 70; 33%).
Based on physical examination by the same physician, patients were diagnosed as suffering from signs and symptoms of CVD (CEAP classes C2, C3 and C4) or as being free of CVD (CEAP classes C0 and C1). Endogenous risk factors, ie, family history of venous disease, history of deep venous thrombosis, current oral contraceptive treatment, and exogenous risk factors, ie, frequency of sauna or tanning visits and standing periods in hours per day during work, were surveyed by questionnaire. A body mass index (BMI) >30 was defined as overweight (dietary guidelines for Americans, 2000).
To evaluate the restriction in quality of life, subjects were asked about temporary or permanent occurrence of heavy legs, edema, pruritus, pigment alterations, restless legs, burning legs, paresthesia, and cramps of the lower extremities.
The intensity of these symptoms was graded into four classes (none, mild, moderate, severe). The number of days absent from work in relation to CVD during the last year was documented.
RESULTS
Demographics and venous risk factors of 209 participants are given in Table II. 139 subjects presented without CVD (104 subjects with C0, and 35 subjects with C1, who were not taken into consideration for symptomatic CVD). A total of 70 subjects (34%) could be classified as having occurrence of CVD, 17% C2 (n = 36), 12% C3 (n = 24) and 5% C4 (n = 10). No C5 or C6 class could be found. The mean age of subjects with occurrence of CVD was not different from that of subjects without CVD (41 years versus 37 years; P < 0.77). Signs and symptoms of CVD were present in 39% of females (n = 63) but only in 15% of males (n = 7), whereby the study population consisted of 3 times more females than males. Within the different professional subgroups group 2 had the lowest severity grading of CVD, and group 3 the highest risk profile for the development of severe CVD (P < 0.02; Table III). Concerning the investigated endogenous risk factors, the only correlation with occurrence of CVD was found for history of deep venous thrombosis. The three subjects who had suffered from earlier deep venous thrombosis were suffering from CVD symptoms, defined as “post-thrombotic syndrome.” Neither intensive sauna nor artificial tanning treatment, nor oral contraceptives (n = 45) were found to be associated with higher incidence of CVD. Subjects with occurrence of CVD spent a significantly longer mean standing period at work than subjects without signs and symptoms of CVD (8.3 hours per day versus5.9 hours per day; P < 0.02). Fifty subjects reported feeling restricted in their quality of life due to diverse symptoms of CVD, including cramps, edema, pruritus, and restless legs, whereby 31 subjects (group 1: n = 10; group 2: n = 7; group 3: n = 14) felt temporary restricted, predominantly in the evening; 19 patients (group 1: n = 2; group 2: n = 3; group 3: n = 14) stated that they suffered permanently from these symptoms. None of the 209 subjects had stayed absent from work during the past last year due to complaints of CVD.
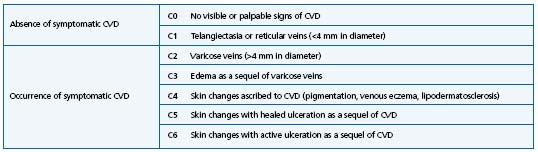
Table II. Demographics and risk profile for chronic venous disease for the 3 professional subgroups.*
* Group 1: doctors and nurses (n = 71)
Group 2: medical technicians, secretaries, and scientific staff (n = 68)
Group 3: cleaners and general staff (n = 70)
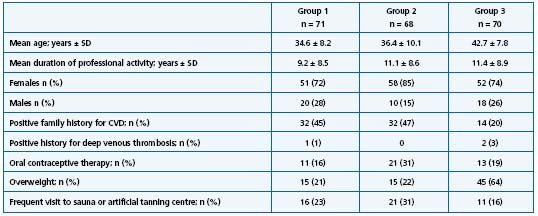
Table III. Correlation of classification of CVD and 3 different professional subgroups* (P < 0.02).
* Group 1: doctors and nurses (n = 71)
Group 2: medical technicians, secretaries, and scientific staff (n = 68)
Group 3: cleaners and general staff (n = 70)
DISCUSSION
In the present study we report a prevalence of 34% of CVD in a wide cross-section of hospital employees (n = 209), varying between 22% and 46% among the different subgroups. The major finding was that longterm standing periods during professional activity were a predisposing factor for CVD. Subjects, with signs and symptoms of CVD exposed their venous system to orthostatic burdens 30% more per day compared to asymptomatic subject. This relationship was particular evident in males, though the overall prevalence of CVD was lower in males than in females.
General staff and cleaners were at higher risk for the occurrence of CVD than other professional groups. This elevated risk may result from hot-humid workplace conditions, under which people in this group usually work. Socioeconomic reasons may also be implicated: whereas some studies report a higher prevalence of venous disease in the relatively underprivileged sectors of the population,26-28 no relationship between the epidemiology of CVD and social class could be found in the Edinburgh Vein Study.29 We found the lowest prevalence of CVD in medical technicians, secretaries, and scientific staff. Since the field of activity of such professions is related to the lowest mean periods of working in a standing position, these results correspond well with our hypothesis of working position being a main risk factor for the development of CVD.
Walking improves the efficiency of the calf muscle pump by lowering the capillary pressure and thereby avoiding venous reflux. In addition, we would recommend, especially for subjects who are predisposed to develop venous disorders (ie, those with a history of deep venous thrombosis) the daily wearing of compression stockings, class II, to prevent venous reflux and the subsequent development of CVD. In addition to its prophylactic effect, compression therapy has important impact on preventing deterioration of existing disease. The presence of peripheral artery disease has to be excluded before prescribing compression therapy.
Even if only 5% of subjects were suffering from skin changes ascribed to CVD, class C4, and none suffered from recent or healed trophic lesions due to severe CVD, class C5 or C6, it should be mentioned that this population was very young (mean age 38 years) and the prevalence and severity grade of CVD rises with age.9
The unexpected lack of correlation between oral contraceptive therapy and the risk of development of CVD in our investigation can be explained by the fact that only a third of the female study population reported the intake of hormones.
Quality of life is increasingly considered as an important outcome measure in diagnostic and treatment studies. Among the high number of studies on quality of life in correlation with disease, only a few deal with CVD.18,30 Subjects suffering from CVD did not report time lost from work, most of them stated their quality of life considerably restricted due to discomfort and complaints from part of their venous disorders.
In conclusion, the high prevalence of CVD in selected workforce populations indicates that CVD might be triggered by occupation-related risk factors. Occupationrelated risk factors could be even more relevant than endogenous risk factors for CVD. The study underlines the requirement for screening interventions in the workplace such as recommendations for primary prophylactic treatment of CVD, in particular for subjects, spending long periods in a standing position and/or working under hot-humid conditions.
ACKNOWLEDGEMENT
This study was supported by a research grant from Servier Austria.
This article is a modification of the original article published in the journal Wien Klin Wochenschr: Ziegler S, Eckhardt G, Stoger R, Machula J, Rudiger HW. High prevalence of chronic venous disease in hospital employees. Wien Klin Wochenschr. 2003 (Sept 15);115(15-16):575-579. It is published here with the kind permission of Karine PECH, Springer Verlag France.

REFERENCES
2. Sobaszek A, Domont A, Frimat P, et al. L’insuffisance veineuse chronique des membres inférieurs en entreprise: enquête realisée auprès de trois populations de salariés français. Arch Mal Prof. 1996;57:157-167.
3. Sobaszek A, Frimat P, Tiberguent A, et al. Venous insufficiency of the lower limbs and working conditions. Phlebologie. 1998;13:133-141.
4. Krijnen RMA, De-Boer EM, Ader HJ, Bruynzeel DP. Venous insufficiency in male workers with a standing profession. Part 1: Epidemiology. Dermatology. 1997;194:111-120.
5. Krijnen RMA, De-Boer EM, Ader HJ, Bruynzeel DP. Venous insufficiency in male workers with a standing profession. Part 2: Diurnal volume changes of the lower legs. Dermatology. 1997;194:121-126.
6. Ziegler T, Winkler C. Unusual cause of leg venous thrombosis in a 20-year-old man. Wi Kli Wo. 2000;112:1039.
7. Scott TE, LaMorte WW, Gorin DR, Menzoian JO. Risk factors for chronic venous insufficiency: a dual case-control study. J Vasc Surg. 1995;22:622-628.
8. Stvrtinova V, Kolesar J, Wimmer G. Prevalence of varicose veins of the lower limbs in women working at a department store. Int Angiol. 1991;10:2-5.
9. Mekky S, Schilling RSF, Walford J. Varicose veins in women cotton workers. An epidemiologic study in England and Egypt. BMJ. 1969;2:591-595.
10. Tuchsen F, Krause N, Hannerz H, et al. Standing at work and varicose veins. Scand J Work Environ Health. 2000;26:414-420.
11. Schobersberger W, Hauer B, Sumann G, et al. Traveler’s thrombosis: incidence, etiology, prevention. Wi Kli Wo. 2002;114:14-20.
12. Fowkes FG, Lee AJ, Evans CJ, et al. Lifestyle risk factors for lower limb venous reflux in the general population: Edinburgh Vein Study. Int J Epidemiol. 2001;30:846-852.
13. Evans CJ, Fowkes FG, Ruckley CV, Lee AJ. Prevalence of varicose veins and chronic venous insufficiency in men and women in the general population: Edinburgh Vein Study. J Epidemiol Community Health. 1999;53:149-153.
14. Porter JM, Moneta GL. Reporting standards in venous disease; an update. J Vasc Surg. 1995;21:635-645.
15. Kistner RL. Classification of chronic venous disease. Vasc Surg. 1997;31:217- 218.
16. Beebe HG, Bergan JJ, Bergqvist D, et al. Classification and grading of chronic venous disease in the lower limbs: a consensus statement. VASA. 1995;24:313- 318.
17. Widmer LK, Stähelin HB, Nissen C, Da Silva A. Venen-Arterienkrankheiten, Koronare Herzkrankheit bei Berufstätigen. Prospektivepidemiologische Untersuchung, Basler Studie I-III (1959-1978). Bern, Stuttgart, Wien: Huber;1981.
18. Rabe E, Pannier-Fischer F, Bromen K, et al. Bonn Vein Study by the German Society of Phlebology. Epidemiological study to investigate the prevalence and severity of chronic venous disorders in the urban and rural residential populations. Phlebologie. 2003;32:1-14.
19. Beebe-Dimmer JL, Pfeifer JR, Engle JS, Schottenfeld D. The epidemiology of chronic venous insufficiency and varicose veins. Ann Epidemiol. 2005;15:175-184.
20. Herrick SE, Treharne LJ, Degiorgio-Miller AM. Dermal changes in the lower leg skin of patients with venous hypertension. Int J Low Extrem Wounds. 2002;1:80-86.
21. Fowkes FG, Evans CJ, Lee AJ. Prevalence and risk factors of chronic venous insufficiency. Angiology. 2001;52 (suppl 1):5-15.
22. Nicolaides AN. Investigation of chronic venous insufficiency: A consensus statement (France, March 5-9, 1997). Circulation. 2000;102:126-163.
23. Samama MM. An epidemiologic study of risk factors for deep vein thrombosis in medical outpatients: the Sirius study. Arch Intern Med. 2000;160:3415-3420.
24. Ziegler S, Eckhardt G, Stoger R, Machula J, Rudiger HW. High prevalence of chronic venous disease in hospital employees. Wien Klin Wochenschr. 2003;115:575-579.
25. Guberan E, Widmer LK, Glaus L, et al. Causative factors of varicose veins. Myths and facts. An epidemiologic study of 610 women. VASA. 1973;2:115-120.
26. Levy E, Los F, Chevalier H, Levy P. The 1999 French Venous Disease Survey: epidemiology, management, and patient profiles. Angiology. 2001;52:195-199.
27. Uber A. The socio-economic profile of patients treated by phlebotropic drugs in Germany. Angiology. 1997;48:595-607.
28. Schmeiser-Riede A, Kunze U, Mitsche N, et al. Self-reported prevalence of venous disease in the general population of Austria-results of the SERMO (Self- Reported Morbidity) Study. Acta Med Austriaca. 1998;25:65-68.
29. Evans CJ, Fowkes FG, Ruckley CV, Lee AJ. Prevalence of varicose veins and chronic venous insufficiency in men and women in the general population. Edinburgh Vein Study. J Epidemiol Community Health. 1999;53:149-153.
30. Kurz X, Lamping DL, Kahn SR, et al. Do varicose veins affect quality of life? Results of an international population-based study. J Vasc Surg. 2001;34:641-648.
