Current management of superficial thrombophlebitis of the lower limb
University of Thessalia Medical School
Chairman of Vascular Surgery Department,
University Hospital of Larissa, Larissa,
Greece
ABSTRACT
Superficial thrombophlebitis is a manifestation of thrombosis that involves the superficial venous system of the lower limb. It is frequently underreported and is considered an insignificant entity. In some cases it may coexist with deep vein thrombosis, or may extend from the superficial system to the deep veins, increasing the risk of complications such as pulmonary embolism. Diagnosis by ultrasound scanning is essential to exclude deep venous thrombosis and confirm the extent of the superficial thrombophlebitis. When superficial thrombophlebitis coexists with deep vein thrombosis, or when the main trunk of the saphenous veins in the vicinity of the junctions is affected, treatment with low molecular weight heparins should be initiated.
EPIDEMIOLOGY, ETIOLOGY, CLINICAL PRESENTATION AND
DIAGNOSTIC APPROACHES
The incidence of superficial thrombophlebitis (STP) in the general population ranges from 3% to 11%,1-5 although this is considered to be an underestimate as only the more symptomatic cases seek medical attention. The mean age at STP presentation is 60 years3,6-12 and the older the patient is the fewer the risk factors required for its development.11,13 STP is more common (50%-70%) in women and prevalence increases with age.3,6,7,11,12,14-21
STP involves the greater saphenous system more often (60-80%) than the lesser saphenous system (10%-20%).3,11,22,23 When STP develops in patients with varicose veins it is confined to the varicose tributaries rather than the saphenous trunks.3,14 The prevalence of STP in patients with varicose veins ranges from 4%-59%;3,11,14,15,23 bilateral SPT is reported in 5%-10% of patients.3,6,11,23,24 Several factors including obesity,3,25-31 age, and protein-S deficiency are associated with SPT in patients with varicose veins.32
The development of STP in the absence of varicose veins is relatively rare (5%-10% of all cases)11,12,33 and various conditions have been implicated in its etiology including autoimmune disease (Behcet’s, Buerger’s, and Mondor’s disease),5,6,16 malignancy,5,6,16,25,34-36 thrombophilia,4-6,8,16,17,26,37-45 mechanical or chemical trauma or injury (venous infusion, catheter introduction),16 radiation injury,16 and bacterial or fungal infections.16 Risk factors are the same as those for the development of deep vein thrombosis (DVT)17,27 and include a history of thrombotic events,46-48 pregnancy,49,50 use of oral contraceptives and hormone replacement therapy, immobilization,18,29,30,31,51 obesity, recent surgery18,52 and trauma,18,51 and sclerotherapy.53,54
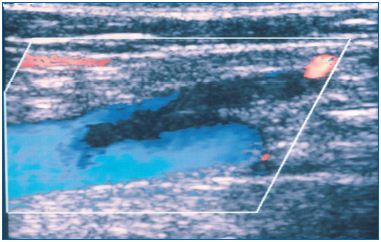
As STP may coexist with DVT in 6%-53% of patients presenting with STP5,9,11,14,15,19,23,55-66 it is important to perform a duplex scan to exclude DVT and to confirm the presence of STP and its extent. Thrombus extension from the superficial system into the deep veins may occur through the saphenofemoral and saphenopopliteal junctions and the perforating veins (Figure 1). Extension from the greater saphenous vein (GSV), particularly when the above knee segment is involved, into the femoral vein is the most common scenario23 and occurs in 17%-19% of cases. When STP affects the below knee segment of the GSV (Figure 2) an association with DVT has been reported in only 4-5% of cases.10,27,57 It should be noted that STP may be a risk factor for the development and recurrence of DVT.3,5,11,22,67,68
 <
<
Figure 1. Thrombus in the greater saphenous vein extending to
the common femoral vein through the saphenofemoral junction.
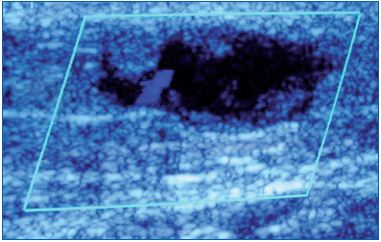
Figure 2. Thrombosed varicosity in the calf.
In the literature, pulmonary embolism in patients with STP has been reported at rates varying from 1.5% to 33%.5,7,11,12,19,23,62,65,69,70 STP is also a risk factor for the recurrence of pulmonary embolism.3,5,11,22,68 Pulmonary embolism is more common when thrombosis is confined to the GSV above the knee (18%) as compared with thrombosis confined to the short saphenous vein (4%).23 However, it is unclear whether pulmonary embolism associated with STP results from a thrombus in the superficial veins, or after its progression to the deep venous system.3
STP may develop during pregnancy, but because the prevalence is very low (0.05-0.1%) it is unclear whether there is any etiological link.3,17,49,50,71-73 However, the problem may be underestimated as the published literature only includes symptomatic patients.49,50
The typical clinical presentation of STP includes local pain, warmth, erythema, and swelling, with the superficial vein becoming solid like a cord.3,6,33,74 It is important to reiterate here the value of Duplex ultrasound for the confirmation of STP, estimation of thrombus extent (Figures 3 and 4), exclusion of DVT and for follow-up.5,6,9,10,20,23,35,55,58-63,75
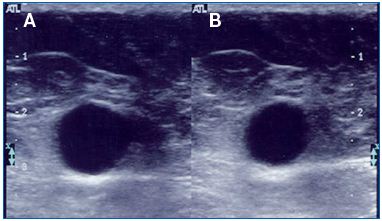
Figure 3. Thrombosed greater saphenous trunk at the thigh:
A. without compression, B. with compression. The vein is
incompressible and dilated containing echolucent material (fresh
thrombus).
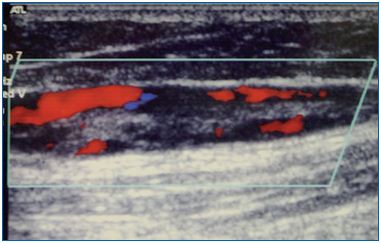
Figure 4. Greater saphenous vein with an old thrombus as
characterized by the presence of recanalization and echogenic
material inside its lumen.
TREATMENT
The treatment of STP varies greatly in clinical practice. Among 634 patients in the POST study, a prospective epidemiologic study conducted in France, treatments included anticoagulation in therapeutic or prophylactic doses, vitamin K antagonists, elastic stockings, topical or oral use of nonsteroidal anti-inflammatory drugs (NSAIDs) and surgery.11
In a randomized study of 562 patients, unfractionated heparin, low-molecular-weight heparin (LMWH) and vitamin K antagonists were found to have equal efficacy and were superior to elastic compression or flush ligation combined with elastic compression in terms of STP extension at 3 months.16
A randomized, double-blind trial of 427 patients52 that compared LMWH (enoxaparin 40 mg and 1.5 mg/ kg) with an NSAID (tenoxicam) or elastic stockings alone for 10 days showed that the prophylactic dose of LMWH (enoxaparin 40 mg) was the most effective treatment. Similar findings were reported in another open randomized trial involving 117 patients.76
The use of high doses of unfractionated heparin twice daily seems to be superior to prophylactic doses, but is inferior to LMWH in prophylactic or therapeutic doses.77-79 A systematic review has shown that both LMWH and NSAIDs significantly reduced the incidence of extension or recurrence of STP by approximately 70% compared with placebo, and both had similar efficacy and safety.80
The CALISTO trial was an international, randomized, double-blind, placebo-controlled trial of 3,002 patients12 that compared subcutaneous fondaparinux 2.5 mg once daily for 45 days with placebo. Participants included hospitalized or nonhospitalized patients 18 years or older, with acute, symptomatic lower limb STP, at least 5 cm long, as confirmed by compression ultrasonography. Exclusion criteria were an interval between the onset of symptoms and planned randomization of more than 3 weeks; treatment for cancer within the previous 6 months; presence of symptomatic or asymptomatic DVT; symptomatic documented pulmonary embolism; STP associated with sclerotherapy or placement of an intravenous catheter; STP located within 3 cm of the saphenofemoral junction; and DVT or pulmonary embolism within the previous 6 months. Patients were also excluded if they had received an antithrombotic agent (other than aspirin at a dose of ≤325 mg per day) for more than 48 hours or a NSAID for more than 72 hours as treatment for the current episode; if in the investigator’s opinion a saphenofemoral junction ligation was required; if they had had major surgery within the previous 3 months; if there were conditions that could confer predisposition to bleeding including creatinin clearance <30 ml/min, platelet count <100,000/mm3; and any women that were pregnant.
The primary efficacy outcome (a composite of death from any cause or symptomatic pulmonary embolism, symptomatic DVT, or symptomatic extension to the saphenofemoral junction or symptomatic recurrence of superficial vein thrombosis at day 47) occurred in 0.9% of patients in the fondaparinux group and 5.9% in the placebo group (P<0.001). The rate of pulmonary embolism or DVT was 85% lower in the fondaparinux group. Similar risk reductions were observed at day 77. No difference was observed in major bleeding between the two groups. However, several concerns were expressed in relation to this trial, especially when applying such treatment to any STP, because of the high cost of the therapy.81
Surgical treatment combined with elastic stockings is associated with a lower rate of venous thromboembolism and progression of STP compared with elastic stockings alone.80 Another review in which surgical therapy was compared with anticoagulation therapy showed similar rates of STP progression, but the incidence of venous thromboembolism and complications were higher with surgery.82 In another study, no difference was observed between surgery and 4 weeks of enoxaparin therapy.83
The role of antibiotics is of no benefit in the management of STP33,84 unless the cause of thrombosis is secondary to an indwelling intravenous catheter.
Hirudoids and some topical agents (piroxicam cream, piroxicam patch) improve local symptoms, alleviating pain and local inflammatory signs, but there is no information on progression to DVT.80,85-87 Local application of heparin was reported to have effects on symptoms comparable to LMWH.88 If tolerated, elastic stockings are traditionally used as an adjunctive treatment together with anticoagulation6,16,33,52,89
In summary, all patients with STP should have bilateral duplex scanning to exclude DVT. As far as treatment is concerned, LMWH in intermediate doses for at least 1 month or fondaparinux 2.5 mg daily for at least 4 weeks are effective therapies. Surgery is no more effective than LMWH, but when the thrombus is close to the saphenofemoral or saphenopopliteal junctions, both are acceptable options depending on the patient’s characteristics and the treating physician’s preference. For isolated STP at the below knee segment confined to varicosities, local application of heparinoids, NSAIDs and elastic stockings form an acceptable treatment option.
1. Widmer LK, Stahelin HB, Nissen C, et al. Venen-Arterienkrankheiten, koronare Herzkrankheit bei Berufstatigen: Prospektiv epidemiologishe Untersuchung. Basler studie I-III 1953-1978. Bern, Swizerland: Huber; 1981.
2. Coon WW, Willis PW III, Keller JB. Venous thromboembolism and other venous disease in the Tecumseh community health study. Circulation. 1973;48:839-846.
3. Leon L, Giannoukas A, Dodd D, et al. Clinical significance of superficial vein thrombosis. Eur J Vasc Endovasc Surg. 2005;29:10-17.
4. Schonauer V, Kyrle PA, Weltermann A, et al. Superficial thrombophlebitis and risk for recurrent venous thromboembolism. J Vasc Surg. 2003;37:834-838.
5. Decousus H, Bertoletti L, Frappé P, et al. Recent findings in the epidemiology, diagnosis and treatment of superficial-vein thrombosis. Thromb Res. 2011;127(suppl 3):S81-S85.
6. Decousus H, Epinat M, Guillot K, Quenet S, Boissier C, Tardy B. Superficial vein thrombosis: risk factors, diagnosis and treatment. Curr Opin Pulm Med 2003;9:393-397.
7. Zollinger RW, Williams RD, Briggs DO. Problems in the diagnosis and treatment of thrombophlebitis. Arch Surg. 1962;85:34-40.
8. Hanson JV, Ascher E, DePippo P , et al. Saphenous vein thrombophlebitis (SVT): a deceptively benign disease. J Vasc Surg. 1998;27:677-680.
9. Ascer E, Lorensen E, Pollina RM, et al. Preliminary results of a nonoperative approach to sapheno-femoral junction thrombophlebitis. J Vasc Surg. 1995;22:616-621.
10. Chengelis DL, Bendick PJ, Glover JL, et al. Progression of superficial venous thrombosis to deep veins. J Vasc Surg. 1996;24:745-749.
11. Decousus H, Quere I, Presles E, et al. POST (Prospective Observational Superficial Thrombophlebitis) Study Group. Superficial vein thrombosis and venous thromboembolism: a large prospective epidemiological study. Ann Intern Med. 2010;152:218-224.
12. Decousus H, Prandoni P, Mismetti P, et al. CALISTO Study Group. Fondaparinux in the treatment of lower-limb superficial vein thrombosis. N Engl J Med. 2010;363:1222-1232.
13. Rosendaal FR. Thrombosis in the young: epidemiology and risk factors. A focus on venous thrombosis. Thromb Haemost. 1997;78:1-6.
14. Lofgren EP, Lofgren KA. The surgical treatment of superficial thrombophlebitis. Surgery. 1981;90:49- 54.
15. Husni EA, Williams WA. Superficial thrombophlebitis of lower limbs. Surgery. 1982;91:70-74.
16. Belcaro G, Nicolaides AN, Errichi BM, et al. Superficial thrombophlebitis of the legs: a randomised, controlled, follow-up study. Angiology. 1999;50:523-529
17. Martinelli I, Cattaneo M, Taioli E, et al. Genetic risk factors for superficial vein thrombosis. Thromb Haemost. 1999;82:1215-1217.
18. Gillet JL, Perrin M, Cayman R. Thromboses veineuses superficielles des membres inférieurs: étude prospective portant sur 100 patients. J Mal Vasc. 2001;26:16-22.
19. U nno N, Mitsuoka H, Uchiyama T, et al. Superficial thrombophlebitis of the lower limbs with varicose veins. Surg Today. 2002;32:397-401.
20. Marchiori A, Mosena L, Prandoni P. Superficial vein thrombosis: risk factors, diagnosis, and treatment. Semin Thromb Hemost. 2006;32:737-743.
21. Binder B, Lacker HK, Salmhofer W, et al. Association between superficial vein thrombosis and deep vein thrombosis of the lower extremities. Arch Dermatol. 2009;145:753-757.
22. Decousus H, Leizorovicz A. Superficial thrombophlebitis of the legs: still a lot to learn. J Thromb Haemost. 2005;3:1149-1151.
23. Lutter KS, Rerr TM, Roedersheimer R, et al. Superficial thrombophlebitis diagnosed by duplex scanning. Surgery. 1991;100:42-46.
24. Barrelier MT. Thromboses veineuses superficielles des membres inférieurs. Actualités Vasculaires Internationales. 1993,17:7-9.
25. Cesarone MR, Belcaro G, Agus G, et al. A. Management of superficial vein thrombosis and thrombophlebitis: status and expert opinion. Angiology. 2007;58:7S-15S.
26. De Moerloose P, Wutschert R, Heinzmann M, et al. Superficial vein thrombosis of the lower limb: influence of factor V Leiden, factor II G20210A and overweight. Thromb Haemost. 1998;80:239-241.
27. Quenet S, Laporte S, Decousus H, et al. Factors predictive of venous thrombotic complications in patients with isolated superficial vein thrombosis. J Vasc Surg. 2003;38:944- 949.
28. Rosito GA, D’Agostino RB, Massaro J, et al. Association between obesity and a prothrombotic state: the Framingham Offspring Study. Thromb Haemost. 2004; 91:683-689.
29. Hansson PO, Eriksson H, Welin L, et al. Smoking and obesity. Risk factors for venous thromboembolism among middle-aged men: “The study of men born in 1913”. Arch Inter Med. 1999;159:1886-1890.
30. Stein PD, Beemath A, Olson RE. Obesity as a risk factor in venous thromboembolism. Am J Med. 2005;118:978-980.
31. Darvall KA, Sam RC, Silverman SH, et al. Obesity and thrombosis. Eur J Vasc Endovasc Surg. 2007;33:223-233.
32. Karathanos CH, Sfyroeras G, Drakou A, et al. Superficial vein thrombosis in patients with varicose veins: role of thrombophilia factors, age and body mass. Eur J Vasc Endovasc Surg. 2012;43:355-358.
33. Gilet JL, Allaert FA, Perrin M. Superficial thrombophebitis in non varicose veins of the lower limbs. A prospective analysis in 42 patients. J Mal Vasc. 2004;29:263-272.
34. Naschitz JE, Kovaleva J, Shaviv N, et al. Vascular disorders preceding diagnosis of cancer: distinguishing the causal relationship based on Bradford- Hill guidelines. Angiology. 2003;54:11- 17.
35. Barrellier MT. Superficial venous thromboses of the legs. Phlebologie. 1993;46:633-639.
36. Krause U, Kock HJ, Kroger K, et al. Prevention of deep venous thrombosis associated with superficial thrombophlebitis of the leg by early saphenous vein ligation. Vasa. 1998;27:34-38.
37. Samlaska CP, James WD. Superficial thrombophlebitis. I. Primary hypercoagulable states. J Am Acad Dermatol. 1990;22:975-989.
38. De Godoy JM, Batigalia F, Braile M. Superficial thrombophlebitis and anticardiolipin antibodies—report of association. Angiology. 2001;52:127- 129.
39. Engesser L, Broekmans AW, Briet E, et al. Hereditary protein S deficiency: clinical manifestations. Ann Int Med. 1987;106:677-682.
40. Pabinger I, Schneider B. Thrombotic risk in hereditary antithrombin III, protein C, or protein S deficiency. A cooperative, retrospective study. Gesellschaft fur Thrombose- und Hamostasefroschung (GTH) Study Group on Natural Inhibitors. Arterioscler Thromb Vasc Biol. 1996;16:742-748.
41. De Godoy JM, Braile DM. Protein S deficiency in repetitive superficial thrombophlebitis. Clin Appl Thromb Henost. 2003;9:61-62.
42. Gorty S, Patton-Adkins J, DaLanno M, et al. Superficial venous thrombosis of the lower extremities: analysis of risk factors, and recurrence and role of anticoagulation. Vasc Med. 2004;9:1-6.
43. Caprini JA, Goldshteyn S, Glase CJ, et al. Thrombophilia testing in patients with venous thrombosis. Eur J Vasc Endovasc Surg. 2005;30:550-555.
44. Leon LR, Labropoulos N. Superficial vein thrombosis and hypercoagulable states: the evidence. Persp Vasc Surg Endovasc Ther. 2005;17:T1-T4.
45. Milio G, Siragusa S, Mina C, et al. S. Superficial venous thrombosis: prevalence of common genetic risk factors and their role on spreading on deep veins. Thromb Res. 2008;123:194- 199.
46. Scurr JH, Machin SJ, Bailey-King S, et al Frequency and prevention of symptomless deep-vein thrombosis in long-haul flights: a randomised trial. Lancet. 2001;357:1485-1489.
47. Cesarone MR, Belcaro G, Nicolaides AN, et al. Prevention of venous thrombosis in long-haul flights with Flite Tabs: the LONFLIT-FLITE randomized, controlled trial. Angiol. 2003;54:531-539.
48. Clarke M, Hopewell S, Juszczak E, et al. Compression stockings for preventing deep vein thrombosis in airline passengers. Cochrane Database Syst Rev. 2006; Apr 19; (2):CD004002.
49. James KV, Lohr JM, Deshmukh RM, et al. Venous thrombotic complications of pregnancy. Cardiovasc Surg. 1996;4:777- 782.
50. McColl MD, Ramsay JE, Tait RC, et al. Superficial vein thrombosis: incidence in association with pregnancy and prevalence of thrombophilic defects. Thromb Haemost. 1998;79:741-742.
51. Samlaska CP, James WD. Superficial thrombophlebitis. II. Secondary hypercoagulable states. J Am Acad Dermatol. 1990; 23:1-18.
52. The STENOX Study Group: A randomized double-blind comparison of low molecular- weight heparin, non-steroidal anti inflammatory agent and placebo in the treatment of superficial-vein thrombosis. Arch Intern Med. 2003;163:1657-1663.
53. Ikeda M, Kambayashi J, Iwamoto, et al. Hemostasis activation during sclerotherapy of lower extremity varices. Thromb Res. 1996;82:87-95.
54. Belcaro G, Geroulakos G, Nicolaides AN. Sclerotherapy and foam sclerotherapy in venous disease: an EVF manual. Turin, Italy: Minerva Medica; 2002.
55. Pulliam CW, Barr SL, Ewing AB. Venous duplex scanning in the diagnosis and treatment of progressive superficial thrombophlebitis. Ann Vasc Surg. 1991;5:190-195.
56. Plate G, Eklof B, Jensen R, et al. Deep venous thrombosis, pulmonary embolism and acute surgery in thrombophlebitis of the long saphenous vein. Acta Chir Scand. 1985;151:241-244.
57. Bergqvist D, Jaroszewski H. Deep vein thrombosis in patients with superficial thrombophlebitis of the leg. BMJ 1986;292:658-659.
58. Skillman JJ, Kent KC, Porter DH, et al. Simultaneous occurrence of superficial and deep thrombophlebitis in the lower extremity. J Vasc Surg. 1990;11:818-824.
59. Prountjos P, Bastounis E, Hadjinikolaou L, et al. Superficial venous thrombosis of the lower extremities co-existing with deep venous thrombosis. A phlebographic study on 57 cases. Int Angiol. 1991;10:63-65.
60. Lohr JM, McDevitt DT, Lutter KS, et al. Operative management of greater saphenous thrombophlebitis involving the saphenofemoral junction. Am J Surg. 1992;164:269-275.
61. Jorgensen JO, Hamel KC, Morgan AM, et al. The incidence of deep venous thrombosis in patients with superficial thrombophlebitis of the lower limbs. J Vasc Surg. 1993;18:70-73.
62. Blumenberg RM, Barton E, Gelfand ML, et al. Occult deep venous thrombosis complicating superficial thrombophlebitis. J Vasc Surg. 1998;27:338-343.
63. Bounameaux H, Reber-Wasem MA. Superficial thrombophlebitis and deep vein thrombosis. A controversial association. Arch Int Med. 1997;157:1822-1824.
64. Murgia AP, Cisno C, Pansini GC, et al. Surgical management of ascending saphenous thrombophlebitis. Int Angiol. 1999;18:3430-3437.
65. Sobreira ML, Maffei FH, Yoshida WB, et al. Prevalence of deep vein thrombosis and pulmonary embolism in superficial thrombophlebitis of the lower limbs: prospective study of 60 cases. Int Angiol. 2009;28:400-408.
66. Galanaud JP, Genty C, Sevestre MA, et al. Predictive factors for concurrent deep-vein thrombosis and symptomatic venous thromboembolic recurrence in case of superficial venous thrombosis. The OPTIMEV study. Thromb Haemost. 2010;105:31-39.
67. Dewar C, Panpher S. Incidence of deep vein thrombosis in patients diagnosed with superficial thrombophlebitis after presenting to an emergency department outpatient deep vein service. Emerg Med J. 2010;27:758-761.
68. Samama MM, Dahl OE, Quinlan DJ, et al. Quantification of risk factors for venous thromboembolism: a preliminary study for the development of a risk assessment tool. Haematologica. 2003;88:1410-1421.
69. Gjores JE. Surgical therapy of ascending thrombophlebitis in the saphenous system. Angiology. 1962;13:241-243.
70. Verlato F, Zuccheta P, Prandoni P, et al. An unexpectedly high rate of pulmonary embolism in patients with superficial thrombophlebitis of the thigh. J Vasc Surg. 1999;30:1113-1115.
71. Kupelian AS, Huda MS. Pregnancy, thrombophlebitis and thromboembolism: what every obstetrician should know. Arch. 2007;275:215-217.
72. Aaro LA, Johnson TR, Juergens JL. Acute superficial venous thrombophlebitis associated with pregnancy. Am J Obstet Gynecol. 1967;97:514-518.
73. Cook G, Walker ID, McCall F, et al. Familial thrombophilia and activated protein C resistance: thrombotic risk in pregnancy. Br J Haematol. 1994;87:873- 875.
74. Kalodiki E, Nicolaides AN. Superficial thrombophlebitis and low-molecularweight heparins. Angiology. 2002;53:659-663.
75. Denzel C, Lang W. Diagnosis and therapy of progressive thrombophlebitis of epifascial leg veins. Zentralbl Chir. 2001;126:374-378.
76. Titon JP, Auger D, Grange P, et al. Therapeutic management of superficial venous thrombosis with calcium Nadroparin. Dosage testing and comparison with a non-steroidal anti-inflammatory agent. Ann Cardiol Angeiol (Paris). 1994;43:160-166.
77. Marchiori A, Verlato F, Sabbion P, et al. High versus low doses of unfractionated heparin for the treatment of superficial thrombophlebitis of the leg. A prospective, controlled, randomized study. Haematologica. 2002;87:523-527.
78. Prandoni P, Tormene D, Pesavento R. The Vesalio Investigators Group. High vs. low doses of low-molecular-weight heparin for the treatment of superficial vein thrombosis of the legs: a doubleblind, randomized trial. J Thromb Haemost. 2005;3:1152-1157.
79. Wichers IM, Di Nisio M, Buller HR, et al. Treatment of superficial vein thrombosis to prevent deep vein thrombosis and pulmonary embolism; a systematic review. Haematologica. 2005;90:672-677.
80. Di Nisio M, Wichers IM, Middeldorp S. Treatment for superficial thrombophlebitis of the leg. Cochrane Database Syst Rev. 2012; Mar 14;3:CD004982.
81. Goldman L, Ginsberg J. Superficial phlebitis and phase 3.5 trials. N Engl J Med. 2010;363:1278-1280.
82. Sullivan V, Denk PM, Sonnad SS, et al. Ligation versus anticoagulation: treatment of above-knee superficial thrombophlebitis not involving the deep venous system. J Am Coll Surg. 2001;193:556-562.
83. Lozano FS, Almazan A. Lowmolecular- weight heparin versus saphenofemoral disconnection for the treatment of above-knee greater saphenous thrombophlebitis: a prospective study. Vasc Endovasc Surg. 2003;37:415-420.
84. Hafner CD, Cranley JJ, Krause RJ, et al. A method of managing superficial thrombophlebitis. Surgery. 1964;55:201-206.
85. Bergqvist D, Brunkwall J, Jensen N, et al. Treatment of superficial thrombophlebitis. A comparative trial between placebo, Hirudoid cream and piroxicam gel. Ann Chir Gynaecol. 1990;79:92-96.
86. Mehta PP, Sagar S, Kakkar VV. Treatment of superficial thrombophlebitis: a randomized, bouble-blind trial of heparinoid cream. Br J Med. 1975;3:614-616.
87. Vilardell M, Sabat D, Arnaiz JA, et al. Topical heparin for the treatment of acute superficial phlebitis secondary to indwelling intravenous catheter. A double-blind, randomized, placebocontrolled trial. Eur J Clin Pharmacol. 1999;54:917-921.
88. Katzenschlager R, Ugurluoglu A, Minar E, et al. Liposomal heparin-spraygel in comparison with subcutaneous low molecular weight heparin in patients with superficial venous thrombosis: a randomized, controlled, open multicentre study. J Kardiol 2003;10:1- 4.
89. Gorty S, Patton-Adkins J, DaLanno M, et al. Superficial venous thrombosis of the lower extremities: analysis of risk factors, and recurrence and role of anticoagulation. Vasc Med. 2004;9:1-6.
