Current management of visceral venous aneurysms
Athanasios D. GIANNOUKAS
Giorgos S. SFYROERAS
Department of Vascular Surgery, University
Hospital of Larissa, University of Thessaly
Medical School, Larissa, Greece
ABSTRACT
Visceral venous aneurysms are considered rare clinical entities with not variable pathogenesis, clinical presentation, natural history, and management. In an electronic search of the pertinent English and French literature, ninety-three reports were identified, including 176 patients with 198 visceral venous aneurysms. Patients’ ages ranged from 0 to 87 years, and there was no apparent male/female preponderance. The commonest location was the portal venous system (87 of 93 reports, 170 of 176 patients, 191 of 198 aneurysms). Portal system venous aneurysms were present with abdominal pain (44.7%), gastrointestinal bleeding (7.3%), or were asymptomatic (38.2%). Portal hypertension was present in 30.8% and liver cirrhosis in 28.3%. Thrombosis and rupture occurred in 13.6% and in 2.2%, respectively. Adjacent organ (common bile duct, duodenum, inferior vena cava) compression was reported in 2.2% The management ranged from watchful waiting to intervention. Indication for operation was symptoms and complications. In 94% of the cases, aneurysm diameter remained stable with no complications during follow-up. Aneurysms of the renal veins and inferior mesenteric vein were also reported. Of six cases of renal vein aneurysm, three were treated surgically and the remaining three were asymptomatic.
Venous aneurysms are reported in the popliteal, jugular, and saphenous veins, but rarely occur in other veins. Visceral venous aneurysms have been increasingly described in recent years probably because of the increasing availability of advanced radiologic imaging in clinical practice. Their prevalence, clinical presentation, and complications have not been adequately reviewed. Most visceral aneurysms are reported in the form of case reports, and there are few published case series that specifically address indications for surgery and optimal surgical techniques.
In a systematic Medline search undertaken to identify all reported cases of visceral venous aneurysms using the keywords “visceral vein”, “splachnic vein” “portal vein”, “intrahepatic portal vein”, “extrahepatic portal vein”, “splenic vein”, “superior mesenteric vein”, “umbilical vein”, inferior mesenteric vein”, “renal vein”, and “aneurysm” ninety-three reports were identified, including 198 visceral venous aneurysms in 176 patients.
Patients’ ages ranged from 0-87 years and there was no apparent male/female preponderance. The most frequent location of visceral venous aneurysms was the portal venous system (87/93 reports, 170/176 patients 191/198 aneurysms).1-87 Aneurysms of the renal vein (6 reports, 6 patients, 6 aneurysms)88-93 and inferior mesenteric vein (1 aneurysm)66 were also described. Figure 1 summarizes the incidence of the visceral venous aneurysms.
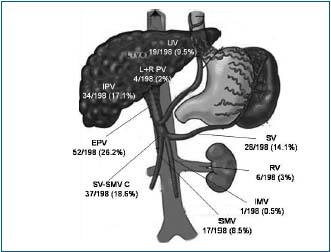
Figure 1. Incidence of the visceral venous aneurysms.
PV: portal vein EPV: extrahepatic portal vein ,
IPV: intrahepatic portal vein, SMV: superior mesenteric vein, SV:
splenic vein, SV-SMV C: splenic vein- superior mesenteric vein
confluence, IMV: inferior mesenteric vein RV: renal vein
Portal venous system
The most frequent location of visceral venous aneurysms is the portal venous system and represents 3% of all venous aneurysms.46 Koc reported a 0.43% prevalence of portal venous aneurysm among 4186 patients.81 As there are variations in the diameters of both normal and cirrhotic portal veins, an aneurysm of the portal venous system is considered to be present if the vessel diameter is larger than 20 mm, especially if the morphology is saccular or fusiform.44,48,81,94 Aneurysms are usually located at the main portal vein, the junction of the superior mesenteric vein and the splenic vein, or at the hepatic hilus.42,46 Intra-hepatic venous aneurysms are rare.81
In the portal venous system the aneurysm was located in the main extrahepatic portal vein in 52 cases, splenic vein in 28 cases, superior mesenteric vein in 17 cases, splenic–superior mesenteric vein confluence in 37 cases, right portal vein in 3 cases, left portal vein in 1 case, intrahepatic portal vein in 34 cases, and umbilical portion of the left portal vein in 19 cases. Extrahepatic portal venous aneurysms ranged from 2.0 to 8.0 cm in diameter and intrahepatic from 1.0 to 7.0 cm.
There are two main theories regarding the etiology of portal vein aneurysms: congenital and acquired. During embryonic development, three anastomoses form between right and left vitelline veins around the future duodenum. A complex process of involution and interconnection of these vitelline veins results in the portal vein. Abnormal development of the portal venous system during this critical period may give rise to an extrahepatic portal vein aneurysm.95 Incomplete regression of the distal right primitive vitelline vein,46,95,96 or a variant branching pattern of the portal vein54 may later form a portal vein aneurysm. Incomplete regression of the distal right vitelline vein leads to a diverticulum that would develop into an aneurysm in the proximal superior mesenteric vein.95 Portal vein anomalies including the right anterior segmental portal vein or the right anterior and posterior segmental portal veins originating from the umbilical portion of the portal vein, and a rightward deviation of the umbilical portion of the portal vein, are associated with aneurysms of the umbilical portion of the left portal vein.54 An inherent weakness of the vessel wall is another potential explanation of a congenital origin. The congenital theory implies a developmental defect of the vein wall as the main cause of aneurysm development. Congenitally or developmentally defective segments may give rise to an aneurysm.47 The congenital theory is based on the presence of aneurysms in children and young adults without portal hypertension.4,5,10,17,33,35 In utero diagnosis of a portal vein aneurysm is evidence in support of the congenital theory.34 The acquired lesions are secondary to chronic liver disease, mainly cirrhosis, portal hypertension, trauma, and pancreatitis.14,42,44,46,81,94 Data regarding these possible etiological factors are available for 162 patients. Portal hypertension was reported in 30.8% (50/162) and liver cirrhosis in 28.3% (46/162) of the patients. Thrombophilia was recently suggested to be an etiologic factor of portal aneurysms. Recurrent thrombosis can cause portal vein occlusion, which results in acute or chronic symptoms of portal hypertension and aneurysm formation.81
The clinical importance of a portal vein aneurysm is related to its size. A small aneurysm usually does not produce symptoms, while large ones are described as the cause of duodenal compression,43,80 inferior vena cava compression,43 biliary tract obstruction,33 and portal vein thrombosis.1,5,19,24,31,46,55,57,61,62,66,74,75,77,81 Data regarding clinical presentation are available for 123 patients. Abdominal pain was reported in 44.7% (55/123) and gastrointestinal bleeding in 7.3% (9/123) of the patients. The aneurysm was asymptomatic and discovered incidentally during abdominal scanning, usually abdominal CT scan and abdominal ultrasound, in 38.2% of the patients (47/123). Other symptoms such as fever, abdominal distension, nausea, loss of appetite, weight loss, vomit, malaise, and jaundice were infrequently reported.
Congenital portal venous aneurysms are generally considered stable lesions and regular follow-up is usually sufficient. Acquired portal venous aneurysms, mainly when they are combined with liver cirrhosis and portal hypertension, can have a more unpredictable clinical course and require closer follow-up, and intervention when complications occur.9 Portal venous system aneurysms require no treatment in most cases. Serial follow-up of patients with abdominal ultrasound is usually sufficient.46,81 In 88% of the patients who were followed up, aneurysm diameter remained stable and no complications occurred. Portal vein thrombosis may necessitate anticoagulation therapy or percutaneous intervention with thrombectomy or thrombolysis.81
Reported complications of untreated visceral venous aneurysms are thrombosis, rupture, and compression of adjacent structures. Complete thrombosis occurred in 24 patients (13.6%) and nonocclusive thrombus in six patients. Rupture was described in four patients (2.2%), one of them during the postpartum period. Two of these four ruptures were splenic vein aneurysms, one intrahepatic and one aneurysm of the right portal vein. Ruptured aneurysm diameter was 2 cm in three of the four cases. The aneurysm compressed the common bile duct in two cases, the duodenum in two cases, and the inferior vena cava in one case.
Management ranged from watchful waiting to intervention.5 There are data for 87 patients, 53 of whom were followed up for between 1 to 72 months (mean 21.15). Follow-up was most commonly performed using abdominal ultrasound. In 50 (94%) of the 53 patients, aneurysm diameter remained stable and no complications occurred. In two patients the aneurysm diameter increased and one underwent cavernous transformation. Thirty-four patients in total underwent surgery. In most cases, the indication for surgery was the occurrence of a complication (thrombosis and rupture) or the presence of symptoms. Operations performed included splenectomy (7 patients), aneurysmorrhaphy (8), aneurysmectomy (3), aneurysmectomy and splenectomy (1), aneurysmectomy with splenectomy and shunt (1), aneurysmorrhaphy and splenectomy (1), distal pancreatectomy and splenectomy (2), aneurysmorrhaphy and portocaval shunt (1), splenectomy, distal pancreatectomy and lienorenal shunt (1), splenectomy and splenorenal shunt (1), portocaval shunt (2), splenorenal shunt (1), liver transplantation (2), and transhepatic thrombectomy and thrombolysis (3).
The type of the procedure is based on the location and size of the aneurysm, the presence of complications, and the comorbidities (portal hypertension and liver cirrhosis). Aneurysmorraphy is the easiest procedure for excision of the aneurysm, mainly when it is saccular, and restores normal luminal diameter of the portal vein. In cases of fusiform aneurysms, if an aneurysmectomy is performed, the conduit used to replace the portal vein can be an allograft from a cadaveric donor, or a synthetic graft.80 The location of the aneurysm is significant for the choice of the procedure. The location was determined in 30 of the 34 operated patients: in 29 it was the extrahepatic portal system. In 4 of them the aneurysm was located in the splenic vein. All patients underwent splenectomy, combined with distal pancreatectomy in three cases.49,59,79,86 Two of the four patients with superior mesenteric vein aneurysm underwent aneurysmorraphy, one aneurysmectomy, and one arterial thrombolysis and transhepatic thrombus aspiration.19,20,41,66 Patients operated for an aneurysm of the extrahepatic main portal vein or superior mesenteric-splenic vein confluence underwent various procedures, most frequently aneurysmorrhaphy.1,31,43,55,58,69,77,80 A single patient with intrahepatic portal aneurysm was operated: he had documented portal hypertension and underwent splenectomy.57 Several patients with documented portal hypertension underwent surgical shunt procedures, alone4,5 or combined with various other procedures.3,24,76,77 These shunt procedures are performed to decompress portal hypertension and do not specifically treat the venous aneurysm. Patients with liver cirrhosis present increased perioperative risk and two out of the five who underwent surgery died during follow-up. Because of the low reported rate of rupture and the risk of surgery in the presence of portal hypertension and liver cirrhosis, there is no strong evidence that prophylactic resection of the portal vein aneurysm is beneficial in these patients.80
Nine patients with portal venous aneurysm died during follow-up, resulting in 10.3% mortality. Three of them presented with complications; rupture or thrombosis. Five of these nine patients were operated, two underwent liver transplantation because of liver cirrhosis, and two had a coexisting malignancy.
Renal vein
Renal vein aneurysms are very rare, with only six cases reported in the English-language literature.88-93 Patient ages ranged from 33-73 years. Five patients were male and three presented with abdominal pain. The remaining three aneurysms were discovered incidentally or during laparotomy.93 Aneurysm diameter ranged from 4 to 5.5 cm. The aneurysm was located in the left renal vein in four cases. The left renal vein is considered to be affected more often by aneurysm formation because of its more complicated embryologic development.88 Renal vein aneurysms must be differentiated from a distended left renal vein, which is recognized as a normal variant.
The nutcracker phenomenon is attributed to compression of the left renal vein as it courses between the superior mesenteric artery anteriorly and the aorta posteriorly.97 Renal vein aneurysms should also be differentiated from idiopathic renal vein varices, especially solitary ones. Renal vein varices are usually smaller than aneurysms and typically are accompanied by a dilated venous network adjacent to the renal pelvis and upper ureter.98 Because of the small number of renal vein aneurysms reported, there are insufficient data regarding optimal treatment. Three of the six patients were treated surgically, two underwent renal vein reconstruction, and one nephrectomy.89,92,93
Inferior mesenteric vein
The only case of inferior mesenteric vein aneurysm is described in a 31-year-old woman who also had a superior mesenteric vein aneurysm and presented with thrombosis.66 She presented aneurysmal dilatation of the inferior vena cava, the hemiazygos vein, the right ovarian vein, and the right iliac internal vein. She underwent arterial thrombolysis and transhepatic thrombus aspiration that resulted in recanalization of the superior mesenteric vein aneurysm. The inferior mesenteric vein aneurysm remained occluded.
A summary of types of treatments of patients with visceral venous aneurysms is displayed in Figure 2.
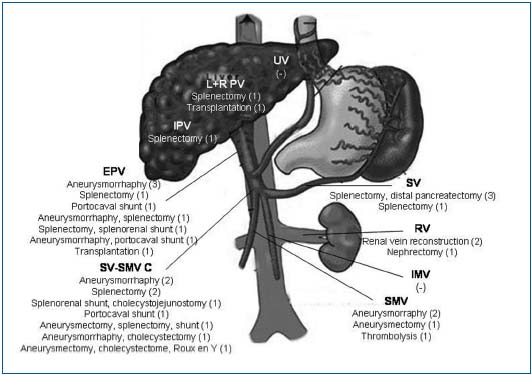
Figure 2.
Types of treatments of
patients with visceral
venous aneurysms.
PV: portal vein EPV:
extrahepatic portal vein ,
IPV: intrahepatic portal
vein, SMV: superior
mesenteric vein, SV: splenic
vein, SV-SMV C: splenic
vein- superior mesenteric
vein confluence, IMV:
inferior mesenteric vein RV:
renal vein
CONCLUSION
Visceral venous aneurysms may not be as uncommon as previously thought and their most frequent location is the portal system. They are often associated with cirrhosis and portal hypertension and their presentation includes abdominal pain and other nonspecific symptoms, or they are discovered incidentally. Watchful waiting is an appropriate treatment, except when complications occur. Most common complications include thrombosis and rupture.
REFERENCES
1. Barzilai R, Kleckner MS. Hemocholecyst following ruptured aneurysm of portal vein. Arch Surg. 1956;72:725-727.
2. Leonsins AJ, Siew S. Fusiform aneurysmal dilatation of the portal vein. Postgrad Med J. 1960;36:570-574.
3. Sedgwick CE. Cisternal dilatation of portal vein associated with portal hypertension and partial biliary obstruction. Lahey Clin Bull. 1960;11:234-237.
4. Hermann RE, Shafer WH. Aneurysm of the portal vein and portal vein hypertension, first reported case. Ann Surg. 1965;162:1101-1104.
5. Thomas TV. Aneurysm of the portal vein: Report of two cases, one resulting in thrombosis and spontaneous rupture. Surgery. 1967;61:550-555.
6. Liebowitz HR, Rousselot LM. Saccular aneurysm of portal vein with agnogenic myeloid metaplasia. N Y State J Med. 1967;67:1443-1447.
7. Vine HS, Sequeira JC, Windrich WC, Sacks BA. Portal vein aneurysm. Am J Roentgenol. 1979;132:557-560.
8. Ishikawa T, Tsukune Y, Ohyama Y, Fujikawa M, Sakuyama K, Fujii M. Venous abnormalities in portal hypertension demonstrated by CT. AJR Am J Roentgenol. 1980;134:271-276.
9. Kane RA, Katz SG. The spectrum of sonographic findings in portal hypertension: a subject review and new observations. Radiology. 1982;142:453- 458.
10. Schild H, Schweden F, Braun B, Lang H. Aneurysm of the superior mesenteric vein. Radiology. 1982;145:641-642.
11. Ohnishi K, Nakayama T, Saito M, Nomura F, Koen H, Tamaru J, et al Aneurysm of the intrahepatic branch of the portal vein. Report of two cases. Gastroenterology. 1984;86:169-173.
12. Sernagor M, Lemone M. Ultrasound and CT studies of an aneurysm of the left portal vein branch. J Belge Radiol. 1985;68:464-465.
13. Cholankeril JV. Superior mesenteric venous aneurysm. Am J Gastroenterol. 1985;80:624-626.
14. Lopez-Rasines GJ, Alonso JR, Longo JM, Pagola MA. Aneurysmal dilatation of the superior mesenteric vein: CT findings. J Comput Assist Tomogr. 1985;9:830-832.
15. Crolla D, Depuyt F, Bruneel M, Rutgeerts L, Van Aelst F, Vermeulen J. Aneurysm of the superior mesenteric vein. J Belge Radiol. 1986;69:447-449.
16.v Boyez M, Fourcade Y, Sebag A, Valette M. Aneurysmal dilatation of the portal vein: A case diagnosed by real-time ultrasonography. Gastrointest Radiol. 1986;11:319-321.
17. Thompson PB, Oldham KT, Bedi DG, Guice KS, Davis M. Aneurysmal malformation of the extrahepatic portal vein. Am J Gastroenterol. 1986;81:695-697.
18. Fanney D, Castillo M, Monatalvo B, Casillas J. Sonographic diagnosis of aneurysm of the right portal vein. J Ultrasound Med. 1987;6:605-607.
19. Wise RH, Retterbush DW, Stanley RJ. CT findings in acute thrombosis of superior mesenteric vein aneurysm. J Comput Assist Tomogr. 1987;11:172-174.
20. Mathias KD, Hoffman J, Krabb HJ, Polonius MJ. Aneurysm of the superior mesenteric vein. Cardiovasc Intervent Radiol. 1987;10:269-271.
21. Andoh K, Tanohata K, Asakura K, Katsumata Y, Nagashima T, Kitoh F. CT demonstration of portal vein aneurysm. J Comput Assist Tomogr. 1988;12:325-327.
22. Lee HC, Yang YC, Shih SL, Chiang HJ. Aneurysmal dilatation of the portal vein. J Pediatr Gastroenterol Nutr. 1989;8:387-389.
23. Kreft B, Harder Th, Kania U. An alcoholic woman with hematemesis, nausea, and abdominal pain. Invest Radiol. 1991;26:203-205.
24. Baker BK, Nepute JA. Computed tomography demonstration of acute thrombosis of a portal vein aneurysm. Mol Med. 1990;87:228-230.
25. Aburano T, Taniguchi M, Hisada K, Miyazaki Y, Shiozaki J, Inoue H, et al. Aneurysmal dilatation of portal vein demonstrated on radionuclide hepatic scintiangiogram. Clin Nucl Med. 1991;16:862-864.
26. Dognini L, Carreri AL, Moscatelli G. Aneurysm of the portal vein: Ultrasound and computed tomography identification. J Clin Ultrasound. 1991;19:178-182.
27. Hagiwara H, Kasahara A, Kono M, Kashio S, Kaneko A, Okuno A, et al. Extrahepatic portal vein aneurysm associated with a tortuous portal vein. Gastroenterology. 1991;100:818-821.
28. Soo MS, Khoury MB, Lupetin AR. Splenic vein aneurysm: MR appearance—a case report. Angiology. 1991;42:590-593.
29. Tanaka S, Kitamura T, Fujita M, Iishi H, Kasugai H, Nakanishi K, et al. Intrahepatic venous and portal venous aneurysms examined by color flow imaging. J Clin Ultrasound. 1992;20:89-98.
30. Savastano S, Feltrin GP, Morelli I, Miotto D, Chiesura-Corona M, El Khatib AB. Aneurysm of the extrahepatic portal vein associated with segmental portal hypertension and spontaneous porto-caval shunting through the inferior mesenteric vein. J Belge Radiol. 1992;75:194-196.
31. Glazer S, Gaspar MR, Esposito V, Harrison L. Extrahepatic portal vein aneurysm: Report of a case treated by thrombectomy and aneurymorrhaphy. Ann Vasc Surg. 1992;6:338-342.
32. Yamaguchi T, Kubota Y, Seki T, Kunieda K, Ogura M, Mizuno T et al. Acquired intrahepatic portal vein aneurysm. Dig Dis Sci. 1992;37:1769- 1771.
33. Fukui H, Kashiwagi T, Kimura K, Goto M, Takei Y, Kasahara A, et al. Portal vein aneurysm demonstrated by blood pool SPECT. Clin Nucl Med. 1992;17:871-873.
34. Gallagher DM, Leiman S, Hux CH. In utero diagnosis of a portal vein aneurysm. J Clin Ultrasound. 1993;21:147-151.
35. Sedat J, Padovani B, Chanalet S. Aneurysm of the superior mesenteric vein. Am J Roentgenol. 1993;161:903- 904.
36. Kumano H, Kinoshita H, Hirohashi K. Aneurysm of intrahepatic portal vein shown by percutaneous transhepatic portography. Am J Roentgenol. 1994;163:1000-1001.
37. Ohhira M, Ono M, Ohhira M, Matsumoto A, Ohta H, Namiki M. Case report: splenic vein aneurysm— report of a lesion that progressively expanded. Br J Radiol. 1994;67:656- 658.
38. Itoh Y, Kawasaki T, Nishikawa H, Ochi J, Miura K, Moriyasu F. A case of extrahepatic portal vein aneurysm accompanying lupoid hepatitis. J Clin Ultrasound. 1995;23:374-378.
39. Shirohara H, Endo M, Sakai K, Tabaru A, Otsuki M. Enlarging splenic vein aneurysm associated with stagnation of splenic venous blood flow. Am J Gastroenterol. 1996;91:385-387.
40. Feliciano PD, Cullen JJ, Corson JD. The management of extrahepatic portal vein aneurysms: Observe or treat? HPB Surg. 1996;10:113-116.
41. Lerch R, Wölfle KD, Loeprecht H. Superior mesenteric venous aneurysm. Ann Vasc Surg. 1996;10:582-588.
42. Fulcher A, Turner M. Aneurysms of the portal vein and the superior mesenteric vein. Abdom Imaging. 1997;22:287-292.
43. Brock PA, Jordan PH Jr, Barth MH, Rose AG. Portal vein aneurysm: A rare but important vascular condition. Surgery. 1997;121:105-108.
44. Ohnami Y, Ishida H, Konno K, Naganuma H, Hamashima Y, Zeniya A et al. Portal vein aneurysm: Report of six cases and review of the literature. Abdom Imaging. 1997;22:281-286.
45. Atasoy KC, Fitoz S, Akyar G, Aytac S, Erden I. Aneurysms of the portal venous system Gray-scale and color Doppler ultrasonographic findings with CT and MRI correlation. Clin Imaging. 1998;22:414-417.
46. Lopez-Machado E, Mallorquin- Jimenez F, Medina-Benitez A, Ruiz-Carazo E, Cubero-Garcia M. Aneurysm of the portal venous system; ultrasonography and CT findings. Eur J Radiol. 1998;26:210- 214.
47. Tolgonay G, Ozbek SS, Oniz H, Süzer E, Yurdakul LO. Regression of splenic vein aneurysm following resolution of splenomegaly. J Clin Ultrasound. 1998;26:98-102.
48. Ozbek SS, Killi MR, Pourbagher A, Parildar M, Katranci N, Solak A. Portal venous system aneurysms: Report of five cases. J Ultrasound Med. 1999;18:417-422.
49. Torres G, Hines GL, Monteleone F, Hon M, Diel J. Splenic vein aneurysm: is it a surgical indication? J Vasc Surg. 1999.29:719-721.
50. Blasbalg R, Yamada RM, Tiferes DA. Extrahepatic portal vein aneurysms. Am J Roentgenol. 2000;174:877.
51. Geubel AP, Maisse F, Boemer F. Images in hepatology. Aneurysm of the trunk of the portal vein. J Hepatol. 2001;34:780.
52. Yang DM, Yoon MH, Kim HS, Jin W, Hwang HY, Kim HS. CT findings of portal vein aneurysm caused by gastric adenocarcinoma invading the portal vein. Br J Radiol. 2001;74:654-656.
53. Ascenti G, Zimbaro G, Mazziotti S, Visalli C, Lamberto S, Scribano E et al. Intrahepatic portal vein aneurysm: three-dimensional power Doppler demonstration in four cases. Abdom Imaging. 2001;26:520-523.
54. Yang DM, Yoon MH, Kim HS, Jin W, Hwang HY, Cho SW et al. Portal vein aneurysm of the umbilical portion: imaging features and the relationship with portal vein anomalies. Abdom Imaging. 2003;28:62-67.
55. Santana P, Jeffrey RB Jr, Bastidas A. Acute thrombosis of giant portal venous aneurysm: Value of color Doppler sonography. J Ultrasound Med. 2002;21:701-704.
56. Lau H, Chew DK, Belkin M. Extrahepatic portal vein aneurysm: A case report and review of the literature. Cardiovasc Surg. 2002;10:58-61.
57. Mucenic M, Rocha Md Mde S, Laudanna AA, Cancado EL. Treatment by splenectomy of a portal vein aneurysm in hepatosplenic schistosomiasis. Rev Inst Med Trop Sao Paulo. 2002;44:261-264.
58. Flis V, Matela J, Gadzijev E. Portal vein aneurysm: When to operate? EJVES Extra. 2003;5:31-33.
59. Shimoda M, Kubota K, Sakuma A, Hogami T, Yamaguchi H, Tagaya N. Intra-abdominal hemorrhage due to rupture of a splenic vein aneurysm: a case report. J Gastrointest Surg. 2003;7:683-686.
60. So NM, Lam WWM. Calcified portal vein aneurysm and porto-hepatic venous shunt in a patient with liver cirrhosis. Clin Radiol. 2003;58:742-744.
61. Okur N, Inal M, Akgül E, Demircan O. Spontaneous rupture and thrombosis of an intrahepatic portal vein aneurysm. Abdom Imaging. 2003;28:675-677.
62. Kim J, Kim MJ, Song SY, Kim JH, Lim JS, Oh YT et al. Acute thrombosis of a portal vein aneurysm and development. Clin Radiol. 2004;59:631- 633.
63. Onbas O, Kantarci M, Alper F, Erdogmus B, Altinkaynak M. Images of interest. Hepatobiliary and pancreatic: Portal vein aneurysm. J Gastroenterol Hepatol. 2004;19:1085.
64. Heeren M, Op de Beeck B, Van den Brande P. Aneurysm of the splenic vein. Acta Chir Belg. 2004;104:322-324.
65. Wolosker N, Zerati AE, Nishinari K, de Melo Galvão Filho M, Wolosker AM.Aneurysm of superior mesenteric vein: case report with 5-year follow-up and review of the literature. J Vasc Surg. 2004;39:459-461.
66. Hechelhammer L, Crook DW, Widmer U, Wildermuth S, Pfammatter T.Thrombosis of a superior mesenteric vein aneurysm: transarterial thrombolysis and transhepatic aspiration thrombectomy. Cardiovasc Intervent Radiol. 2004;27:551-555. Epub 2004 Jul 30.
67. Ferraz-Neto BH, Sakabe D, Buttros DA, Resende MB, Afonso RC. Portal vein aneurysm as late complication of liver transplantation: a case report. Transplant Proc. 2004;36:970-971.
68. Kaido T, Taii A, Nakajima T. A huge intrahepatic portal vein aneurysm. Abdom Imaging. 2005;30:69-70.
69. Jin B, Sun Y, Li YQ, Zhao YG, Lai CS, Feng XS et al. Extrahepatic portal vein aneurysm: Two case reports of surgical intervention. World J Gastroenterol. 2005;11:2206-2209.
70. Alexopoulou A, Papanikolopoulos K, Thanos L, Dourakis SP. Aneurysmal dilatation of the portal vein: A rare cause of portal hypertension. Scand J Gastroenterol. 2005;40:233-235.
71. Hosoki Y, Saito H, Sakurai S, Suzuki Y, Inoue M, Miyoshi S, et al. Enlarging splenic vein aneurysm associated with increasing portal hypertension. J Gastroenterol. 2005;40:1078-1079.
72. Kocakoc E, Kiris A, Bozgeyik Z, Uysal H, Artas H. Splenic vein aneurysm with calcification of splenic and portal veins. J Clin Ultrasound. 2005;33:251- 253.
73. Cömert M, Erdem LO, Ozdolap S, Erdem CZ, Sarikaya S. Splenic vein aneurysm demonstrated by magnetic resonance angiography. Dig Dis Sci. 2005;50:1344-1346.
74. De Gaetano AM, Andrisani MC, Gui B, Maresca G, Ionta R, Bonomo L. Thrombosed extrahepatic portal vein aneurysm: Report of two cases and review of the literature. Abdom Imaging. 2006;31:545-548.
75. Laumonier H, Montaudon M, Corneloup O, Brunot S, Laurent F. CT angiography of intrahepatic portal aneurysm. Abdom Imaging. 2005;30:755-757.
76. Luo HF, Wang HJ, Li B, Wang ZY. Diagnosis and management of extrahepatic portal vein aneurysm: A case report. Hepatobiliary Pancreat Dis Int. 2006;5.
77. Wolff M, Schaefer N, Schmidt J, Hirner A. Thrombosis of a large portal vein aneurysm: Treatment by thrombectomy, aneurysmorrhaphy and portocaval shunt. J Gastrointest Surg. 2006;10:128-131.
78. Giavroglou C, Xinou E, Fotiadis N. Congenital extrahepatic portal vein aneurysm. Abdom Imaging. 2006;31:241-244.
79. Shah OJ, Robbani I. Splenic vein aneurysm in association with extrahepatic portal hypertension. Ann Saudi Med. 2006;26:237-238.
80. Cho SW, Marsh JW, Fontes PA, Daily MF, Nalesnik M, Tublin M, et al. Extrahepatic portal vein aneurysm— report of six patients and review of the literature. J Gastrointest Surg. 2008;12:145-152.
81. Koc Z, Oguzkurt L, Ulusan S. Portal venous system aneurysms: imaging, clinical findings, and a possible new etiologic factor. Am J Roentgenol. 2007;189:1023-1030.
82. Garg MK, Sandhu MS, Kalra N, Chawla YK. Partially thrombosed splenic vein aneurysm. J Postgrad Med. 2007;53:50-51.
83. Perret WL, de Silva A, Elzarka A, Schelleman A. Portal circulation aneurysms: two case reviews. Australas Radiol. 2007;51:87-90.
84. Ho CM, Tsai SF, Lin RK, Liang PC, Sheu TW, Hu RH et al. Computer simulation of hemodynamic changes after right lobectomy in a liver with intrahepatic portal vein aneurysm. J Formos Med Assoc. 2007;106:617-623.
85. Miyazaki K, Takatsuki M, Eguchi S, Hidaka M, Tokai H, Hamasaki K et al. Living donor liver transplantation for hepatitis C virus cirrhosis with a huge portal vein aneurysm. Liver Transpl. 2008;14:1221-1222.
86. Parpaglioni R, Metta E, Zagari A, Celleno D. Spontaneous splenic vein aneurysm rupture in the puerperium. Int J Obstet Anesth. 2009;18:48-51.
87. Weber G, Milot L, Kamaoui I, Pilleul F. Splanchnic vein aneurysms: a report of 13 cases. J Radiol. 2008;89:311-316.
88. Yoneyama T, Baba Y, Fujiyoshi F, Hokotate H, Inoue H, Nakajo M. Left renal vein aneurysm: imaging findings. Abdom Imaging. 2003;28:233-235.
89. Val-Bernal JF, Fernández N, López- Rasines G. Symptomatic solitary right renal vein aneurysm: a case report. Cardiovasc Pathol. 2000;9:29-32.
90. Khader SM, Saleeb SF, Teplick SK. General case of the day. Left renal vein aneurysm. Radiographics. 1999;19:1683-1685.
91. Kabaalio lu A, Yilmaz S, Apaydin A, Sindel T, Ozkaynak C, Lüleci E. Renal vein aneurysm: diagnosis with color Doppler sonography. Am J Roentgenol. 1997;168:645-646.
92. Krinsky G, Johnson G, Rofsky N, Shapiro R, Yang B, Weinreb J. Venous aneurysms: MR diagnosis with the “layered gadolinium” sign. J Comput Assist Tomogr. 1997;21:623-627.
93. Irace L, Gossetti B, Benedetti-Valentini F, Francalanci P, Gallo P. Aneurysm of the left renal vein: a case report. J Vasc Surg. 1994;19:943-944.
94. Doust BD, Pearce JD. Gray-scale ultrasonic properties of the normal and inflamed pancreas. Radiology. 1976;120:653-657.
95. Gallego C, Velasco M, Marcuello P, Tejedor D, DeCampo L, Friera A. Congenital and acquired anomalies of the portal venous system. RadioGraphics. 2002;22:141-159.
96. Condat B, Valla D. Nonmalignant portal vein thrombosis in adults. Nat Clin Pract Gastroenterol Hepatol. 2006;3:505-515.
97. Buschi AJ, Harrison RB, Norman A, Brenbridge AG, Williamson BR, Gentry RR et al. Distended left renal vein: CT/sonographic normal variant. Am J Roentgenol. 1980;135:339-342.
98. Beckmann CF, Abrams HL. Idiopathic renal vein varices: incidence and significance. Radiology. 1982;143:649- 652.
