Discovery of lymphatic filariasis during a humanitarian aid mission to Burkina Faso
André CORNU-THENARD
Jean-Luc GILLET J
Nathalie GRIMALDI
Elizabeth CORNU-THENARD
Nelly GILLET
Rue du Fbg Saint-Antoine
75012 Paris, France
SUMMARY
Lymphatic filariasis affects 120 million persons worldwide, a third of whom live in Africa. It is caused by threadlike parasitic worms transmitted to humans by the bite of mosquitoes which are vectors of the disease. One of the effects resulting from a mosquito bite affecting a lower limb is the occurrence of lymphedema. When the latter becomes massive, it is known as elephantiasis. The purpose of the December 2009 aid mission was to treat patients with this disease by using compression therapy. Also, it was planned to study, in cooperation with the local health authorities, the possible setting up of a specific care facility to train nurses in the different methods of compression therapy, which remarkably is missing from the therapeutic arsenal in Burkina Faso. These nurses would care for the many patients affected: over 150 identified in 2000 in the city of Kaya alone, without counting cases of hydrocele, and involvement of the upper limbs, genital organs, and breasts.
The aim of our humanitarian aid mission was to take care of all cases of lymphatic disease using appropriate treatments.
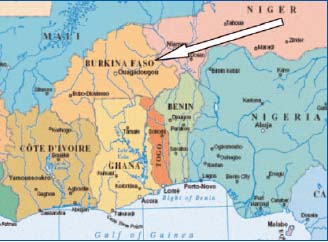
Figure 1. Location
of Burkina Faso in
West Africa
Since 1998, the not-for-profit organization Kontacts has been going to Kaya, Burkina Faso, a city located some 100 km north-east of the capital, Ouagadougou, in the framework of exchanges between young French aid workers and the Burkinabé (Figure 1). Kontacts is non-political and non- denominational, which allows us to work with partners whether Christian, Moslem, or Animist. Three avenues of exchange with the population have been initiated: education and teaching, art and culture, and hygiene and health. Achievements hitherto are detailed on the French-language Web site www.kontacts.org.
In January 2009, during another stay in Kaya, we discovered two young people with enormous lymphedema (Figure 2a, 2b and Figure 3a, 3b). Failure to recognize this vascular infectious disease led us to a surprising discovery, for which currently there are few details in our European manuals: lymphatic filariasis.

Figure 2a. Patient 1 – Bilateral elephantiasis, right panel
(January 2009).

Figure 2b. Patient 1 – Detailed view of right foot. Verrucous
swelling on the dorsal aspect of the foot overlaps anteriorly and
covers the toes.

Figure 3a. Patient 2 – Elephantiasis of the left foot

Figure 3b. Patient 2 – The first bandage
LYMPHATIC FILARIASIS
Epidemiology
Lymphatic filariasis is a threat in nearly 80 countries. Of 120 million persons already affected, over 40 million are seriously disabled. A third of those afflicted live in Africa, another third in India, and the remainder in South Asia, the Pacific islands, and in South America.1 Lymphatic filariasis is the second leading cause of permanent disability worldwide,2 in particular due to the fact that generally it is acquired in early childhood (www.filariasis.org). It results not only in major physical disabilities, but also in psychological and social ones. The social life of these young people is especially disastrous. The disease is considered as a curse, those afflicted hide and so have no family life, do not attend school, and have almost no friends.
Cause
Lymphatic filariasis is caused by threadlike parasitic worms, Wuchereria bancrofti and Brugia malayi, which reside in the lymphatic system and for which humans are the only definitive host.
Transmission
The disease is spread by mosquitoes (Figure 4).1-4
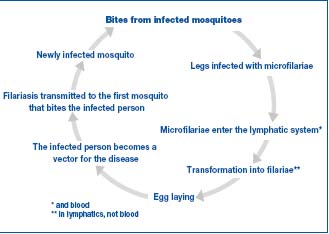
Figure 4. Transmission of the disease and the vicious circle.
Signs
The disease usually develops in adults. In its most visible forms, lymphatic filariasis causes elephantiasis of the legs or arms, the genital organs (hydrocele), the vulva, or breasts. Subclinical alterations, in particular renal, are common.
Diagnosis
Several methods of diagnosis are possible: the most conventional consists in examining a blood sample and visualizing the microfilaria. This examination must be conducted when the parasites are circulating in the bloodstream, ie, at night. A simple, sensitive, and specific test to detect the antigen, the ICT filariasis test, detects infection within a few minutes (www.filariasis.org). Ultrasonography can visualize the adult worms, which can be 10 cm long.
Treatment
A worldwide program of eradication of this disease was launched by the WHO in 2000.2 Only a short time ago, only 48 out 81 countries were applying these recommendations. The primary objective of treatment is to interrupt transmission of filariasis by administration of massive amounts of two medicinal products in a single dose. Three microfilaricides—diethylcarbamazine, ivermectin, and albendazole—can be prescribed in combination (called “DIA” treatment if all three are used). The macrofilaricide doxycycline at a dosage of 200 mg/day for 8 weeks can be used for individual treatment, but not mass eradication.5 In Burkina Faso, the WHO program is re-launched every 2 to 3 years for treatment of the younger generations. The difficulty lies in reaching populations in isolated villages.
Once the disease is established, nothing really can be done: lower limb elephantiasis, hydrocele, swelling of the genital organs, and breast hypertrophy can take on proportions that today are difficult to imagine. In the city of Kaya alone over 600 cases of hydrocele, and 150 of elephantiasis of the foot, 30 of the arms, and 20 involving the breasts were identified in 2008.
For doctors who are vascular specialists, compression therapy, combined with sessions of manual lymphatic drainage and night-time postural drainage is the basic treatment for reduction of lymphedema. Our discussions with people at the Regional Hospital Center of Kay suggested that compression therapy is unknown. Apart from elevating the affected limb, the only treatment applied in an emergency or when there are ulcer complications is amputation! This is probably also true in other countries of western Africa. The reason may lie in the fact that after the departure of the Europeans during the 1960s, compression therapy was abandoned, probably as the result of a lack of clinical supplies. Lastly, it should be noted that old case reports indicate that MPFF (micronized purified flavonoid fraction, Servier, France) seemed to be really effective on this type of lymphedema.6
HUMANITARIAN AID MISSIONS 2009-2010
January 2009: A discovery
This mission to “investigate areas of additional intervention” for Kontacts revealed no venous lymphatic disorder of the limbs. We did not imagine that such a disease could exist in a population which has produced world class athletes, but through Father Theophile, the parish priest, we discovered two young men with massive lymphedema (Figures 2a, 2b and 3a).
In the first patient the disease was extensive and in particular affected both legs, preventing him from walking unaided (Patient 1, Figure 2a). The edema of the dorsal aspect of his right foot concealed his toes (Patient 1, Figure 2b). The second (Patient 2, Figure 3a) arrived on crutches.
Compression therapy was immediately initiated in both patients. Biflex® bandages (Laboratoires Thuasne), which we had brought at the request of a nurse during a previous trip, were applied (Figure 3b).7 The improvement during the few days prior to our return to France was remarkable. Subsequently, videoconference monitoring (our thanks to the Skype Phone Service) was used to assess medical and psychological improvement in the condition of these two young patients (Figure 5).

Figure 5. Same patient (Patient 1) as in fig 2a and 2b, 6 months
later (photo sent by video transmission)
December 2009: A revolution
The aim of this trip was threefold: To see these two patients again, to treat other patients and, in particular, in cooperation with the local health authorities, to study the feasibility of creating a specific health care unit for treatment of elephantiasis. The group comprised 3 vascular specialists, 2 nurses, and 2 young men about 25 years old. Onsite expenses were paid for by a donation, but each person paid for his own airline ticket, in accordance with the principles of Kontacts. In terms of preventive measures, each of us brought about fifteen kilos of bandages and elastic stockings, since it is not possible to find these items locally.
On our arrival, we were able to observe that the progress made by our two patients, followed up over the Internet, was in fact real.8 They had resumed almost normal activity and self-sufficiency enabling them to walk easily (Figure 6). Much to the surprise of those who had not yet seen them, these 2 young men were taking care of themselves, performing careful hygienic care, and massages similar to those of lymphatic drainage, with karité (shea) butter (Figures 7, 8, 9), and in particular application of 3, 4, or 5 Cotton Short Stretch, Biflex 17, Urgoband, Medica 315 or Somos bandages (provided by the manufacturers prior to our departure). Very often, this bandage was covered with a medical compression stocking for purely cosmetic purposes. In these cases, an extensor often helped in placing the stocking over the bandage (Figure 10).9
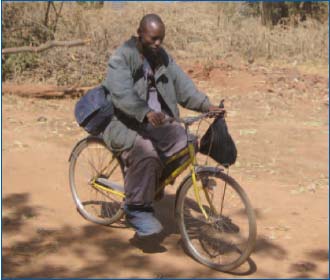
Figure 6. Our two young patients were self-sufficient starting in
August after 8-month treatment (photo of December 2009)

Figure 7. Same patient (Patient 1) performing massage similar to
lymphatic drainage. Note the large decrease in size of the
papilloma on the ankle joint.

Figure 8. Massaging with shea butter on left foot and leg: Note
the position of both hands (Patient 1).

Figure 9. Detailed view of papillomatosis of left foot (December
2009).

Figure 10. Use of an extensor for placement of an elastic stocking
over 2 bandages.
These two patients, who became “super nurses”, truly surprised us because, apart from a succinct demonstration that we gave them a year previously, they had not received any formal training. Everyone was also amazed by the excellent acceptance of such a bandage, so inelastic10,11 and thick, in a country with high temperatures. During this stay, many other patients were examined, including a thirty-year-old male who presented with massive elephantiasis manifest as overlapping redundant skin folds, associated with a wound about 40 cm² in size (Patient 3, Figure 11).

Figure 11. Patient 3 – Elephantiasis with redundant skin folds,
associated with a wound of about 40 cm² (December 2009). Patient
was scheduled for amputation.
For the onsite medical staff, in particular Dr Mohamed Sidi, Deputy Medical Director of the District Hospital of Kaya, this compression therapy was an absolute novelty He qualified it as “revolutionary”. Enthusiastic, he encouraged us to continue the idea of creating a dispensary reserved for elephantiasis. The hospital might be able to make available to us a small building, the old maternity clinic unused for 5 years, which would have to be renovated (Figures 12, 13). It might also assign us a nurse whom we would train, and who, in our absence, would be in charge of maintaining continuity of care.
Upon our return, we received the following estimates: 8000€ for renovation of the building, 6000€ for installation costs, probably 4000€ for computer equipment, and 2000€ for annual operating costs. At the same time, we learned that we had received a 2500€ grant from the Ministry of Cooperation and French Culture (see www.kontacts.fr).

Figure 12. Old hospital maternity ward, unused, to be renovated.

Figure 13. Need for renovation is obvious.
April 2010: Disappointment followed by joy
Our trip was planned to discuss these estimates for the renovation, while agreeing that some work could be postponed. Dr Sidi, still enthusiastic since he was participating in the setting up of the first center for elephantiasis in Burkina Faso, again welcomed us, but with less eagerness: A note from the Ministry of Health dated 7 April 2010, “prohibited all foreign doctors from performing medical consultations without authorization signed by the Minister himself.” Our enthusiasm collapsed, but just for a moment. As in December, we could perform consultations in a building made available to us by the church, and to speed up the implementation of the project we decided with Dr Sidi to create a Burkinabé Kontacts not-for-profit organization, which will make it possible for us to work in the hospital as soon as it is officially recognized.
This somewhat puzzling situation did not allow us to plan renovation of the building before the summer of 2010. Nevertheless, the planned operations were discussed:
• The dispensary would be the site from which an allterrain vehicle would be dispatched to bring to the clinic patients with elephantiasis, identified by nurses in the corresponding villages. This vehicle could also be used by a specialist nurse to visit the bedside of patients unable to travel (so purchase of a vehicle and two motorcycles had to be added to the planned budget, ie, 4200€).
• On arrival, a team of nurses and doctors would examine the patients, explain the disease, check that they had in fact taken the treatment for the parasitic disease, start treatment of lymphedema, and explain how to use the bandages in the following weeks. The patients would then be driven back to their village.
• Villages would be visited in rotation, according to the instructions of the nurses working there (identification of the different disorders was performed regularly).
Medically, there were three undeniable reasons for satisfaction:
The previous two patients (1 and 2) are improving, we their own care themselves (Figure 14). They made an extensor to make it easier to put on the medical compression stockings. We will show them how to put on several bandages, one over the other, to obtain stronger and more inelastic compression, and so more effective reduction of lymphedema (Figure 15).12
In the thirty-year-old patient (Patient 3, Figure 11), the ulcer healed but lymphedema of the foot worsened (Figure 16). The reason seemed obvious to us: the bandage had covered the ulcer zone but not the foot. This patient was to return to the consultation every day during our stay, but we never saw him again.

Figure 14. April 2010, the same patient’s legs, (Patient 1) ie,
after a year and half of self-care.

Figure 15. Wrapping of three 20 mm Hg elastic stockings, ie
about 60 mm Hg.

Figure 16. Patient 3 – April 2010: The 40 cm² wound has
healed, but lymphedema has markedly progressed.
The first two patients took it upon themselves to explain to other patients how important it is to comply with treatment. In our absence they took care of other young patients who had the same problem: oral explanations, care, bandages, and distribution of a document they themselves had written. In no time at all, they became specialists in reduction of elephantiasis, an unforeseen and major event. Consequently, Dr Sidi suggested the principle of making them head the dispensary. In the midst of our medical and political concerns, and in temperatures of 40°C in the shade, we were nevertheless able to attend to other areas of interest to Kontacts: contacts with schools (Figure 17), contests to collect plastic bags strewn in large numbers in streets, fields, and even in the schools (Figure 18), help teaching reading and writing in the evening for the youngest children.
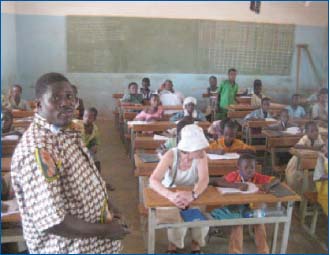
Figure 17. Contact with teachers to give them school supplies and
to ask what they need.
Figure 18. Collection of plastic bags by school children.
Videoconference monitoring: The unimaginable happens
As before, videoconferencing was used every Wednesday. In May, the use of a 3G key improved image and sound quality. We understood that the actions of our youthful assistants continued to increase. By going through the city, other young people with the disease were discovered. They made every effort to convince them of the need to be treated by wrapping using several bandages and stockings. We receive photos of these new patients regularly. What a success! Without asking for anything, they are doing remarkable work.
As soon as the building has been renovated, we will make certain they are recruited, with a salary reserved for the best nurses. This rehabilitation project seems imminent, because as of the end of July, the Burkinabé Kontacts was officially recognized . Authorization from the Burkina Faso Ministry of Health to practice medicine has yet to be obtained, as has an official document allocating to us this old maternity building.
Future missions
September 2010: Launch of building renovation. The Skype phone system may be adequate, but closer supervision seems preferable.
November 2010: Departure of a group of vascular specialist doctors and surgeons to continue our initiatives (the number is not limited; for information see www.kontacts.org).
September 2011: Planned departure just after the UIP Congress in Prague.
Other trips are planned but will depend on budgets and donations received (pharmaceutical firms, private persons or sponsors). Donations are not used to pay for airline tickets but to pay for our actions in the field. No money is given. Each paid action is detailed in an invoice: the entire accounting system is transparent (see Web site for additional information).
To finish this section and to catch a glimpse of the future, according to what was said by the Ambassador of Burkina Faso in France, his Excellency Luc Tiao, if completion of this first dispensary is a success, many other centers could be built in Burkina Faso. We will make use of what has been done in India to fight this scourge (www.filariajournal.com) and information given by the Global Alliance to Eliminate Lymphatic Filariasis which indicates that Burkina Faso is one of the countries of Africa which best fights for eradication of lymphatic filariasis.13,14 The mission of these healthcare centers will be identical: To restore hope to abandoned young people and to rehabilitate them socially, educationally, and occupationally. In a word to restore their freedom. We have much work to do.
IN CONCLUSION
Lymphatic filariasis continues to affect millions of people worldwide. One of its results is the occurrence of lower limb lymphedema which can assume massive proportions, whence the term elephantiasis. Our humanitarian aid missions have enabled us to discover this terrible disease, and to make every effort to treat it so as to prevent the worst possible treatment, amputation. The basic treatment for reduction of elephantiasis is compression therapy, which we have used to good effect several times. The most unbelievable event in this medical adventure was that some patients spontaneously managed fellow sufferers. What satisfaction!
REFERENCES
1. Carme B. Filariose. Revue du Praticien. 2007;57:157-164.
2. OMS. Filariose lymphatique. R.E.H. 2003;78:171-179.
3. OMS. Programme mondial pour l’élimination de la filariose lymphatique. R.E.H. 2008;83:333-341.
4. Vaqas B, Ryan TJ. Lymphoedema: Pathophysiology and management in resource-poor settings- relevance for lymphatic filariasis control programmes. Filaria Journal. 2003,2:1-10.
5. Taylor MJ, Makunde WH, McGarry HF, et al. Macrofilaricidal activity after doxycycline treatment of Wuchereria bancrofti: A double-blind randomised placebo-controlled trial. Lancet. 2005;365:2116-121.
6. Das LK, Subramanyam Reddy G, Pani SP. Some observations on the effect of Daflon (micronized purified flavonoid fraction of Rutaceae aurantiae) in bancroftian filarial lymphoedema. Filaria Journal. 2003,2:5.
7. Cornu-Thenard A, Cornu-Thenard E. Un séjour humanitaire au Burkina- Faso. Une aide de la télémédecine pour la phlébologie. Phlébologie. 2009, 62,4:87-89 (Abstract in English).
8. Gillet JL, Cornu-Thenard A, Grimaldi N, et al. Prise en charge des éléphantiasis et projet de création d’une unité de soins spécifique. Phlébologie. 2010,63,1:81-87 (Abstract in English).
9. Cornu-Thenard A. Un extenseur au service de la compression. JMV. 1980,5:73-74
10. Partsch H, Rabe E, Stemmer R. The Compressive Treatment of Members. Editions EPF. 2000.
11. Partsch H, Damstra RJ, Tazelaar DJ, et al. Multicentre randomised controlled trial of four-layer bandaging versus short-stretch bandaging in the treatment of venous leg ulcers? VASA. 2001;30:108-113.
12. Cornu-Thenard A, Boivin P. A new technique for reduction of lower limbs edema: Elastic stockings. NASP Intensive Course in Phlebology. 1991 Houston. Ed PRM. Dallas, Texas, 339- 345.
13. Moffat CJ. International development of the Lymphoedema Framework. Journal of Lymphoedema. 2008,3,2,37- 38
14. Jacobson J. GAELF. The Gates Foundation Perspective, Report April 2008,13-16.
