Duplex ultrasonography protocol for investigation of patients presenting with recurrent varicose veins after surgery
France
SUMMARY
Duplex ultrasonography has become the investigation of reference in patients presenting with recurrent varicose veins after surgery. It consists of three methods of investigation: B-mode ultrasound, pulsed duplex ultrasound, and color duplex scanning. A complete investigation of the different venous systems is necessary:
– the deep venous network, identifying any abnormalities that may be postthrombotic or a primary cause
– the superficial venous network and the perforator veins, identifying the origin(s) of the deep vein reflux to the superficial venous network, and also performing a complete, anatomical, and hemodynamic evaluation of the varicose vein network
Duplex ultrasonography enables precise anatomical and hemodynamic diagnosis of recurrent varicose veins. A precise description of different types of varicose vein recurrence, in particular, in the former saphenofemoral and popliteal junctions, is beyond the scope of this protocol.
Duplex ultrasound scanning has become the investigation of reference in patients presenting with post-surgical recurrent varicose veins. It consists of three methods of investigation: B-mode ultrasound, pulsed duplex ultrasound, and color duplex scanning.
A complete investigation of the different venous systems is necessary.
A- Investigation of the deep venous network
The examination should investigate the totality of the deep vein network from the inferior vena cava to the calf veins in the lower one-third of the leg. Abnormalities of the deep veins can be postthrombotic6 or primary in origin.7 Postthrombotic abnormalities can be obstructive and responsible for venous reflux or combined obstruction + reflux. The examiner should first look for anatomical anomalies using B-mode ultrasound, and then hemodynamic abnormalities.
1) A normal vein is totally compressible with the ultrasound transducer. Postthrombotic abnormalities are suggested by a non-compressible or partially compressible vein, hyperechoic parietal calcifications, or endoluminal fibrous formations (Figure 1). Special attention should be paid to the femoral vein (former superficial femoral vein) in the thigh which usually has several large branches, only one of which can be affected by postthrombotic abnormalities. Investigation of the calf veins requires careful adjustment of the different ultrasound parameters.
2) Hemodynamically, the absence of venous flow or the existence of diminished flow compared with the contralateral veins indicates an obstructive effect of postthrombotic abnormalities. Deep vein reflux of duration greater than 1 second (Figure 2) is considered significant.8-11 Reflux of duration greater than 0.5 seconds is considered significant for the deep femoral vein and the calf veins, whether it involves the posterior tibial crural veins, the anterior tibial or fibular veins, the gastrocnemius calf veins (former triceps sural veins), or the soleus veins.8-11
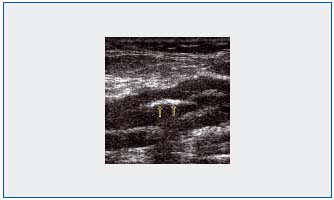
Figure 1: Visualization with B-mode ultrasonography of postthrombotic endoluminal fibrous formations.
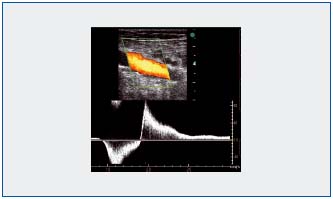
Figure 2: Identification with color duplex ultrasound and pulsed duplex ultrasound of a reflux greater than 1 second in a popliteal vein.
3) Methodology of the examination
The investigation consists of 3 phases:
1- Investigation of the inferior vena cava and the iliac veins is carried out with the patient supine. In a normal subject, gentle pressure exerted by the ultrasound transducer completely compresses the veins. In color and pulsed mode ultrasound scanning, the examiner checks the spontaneous blood flow, modulated by respiration and accelerated by manual compression of the thigh muscles. Then, with the Doppler transducer successively placed on the two common femoral veins, the examiner looks for blood flow modulated by respiration and by a Valsalva maneuver: abrupt stoppage of venous flow followed by its rapid resumption at the end of this maneuver is an important finding predictive of normal iliocaval patency.
With the patient still supine, the examiner looks for the following:
* reflux in the common femoral vein and in the deep femoral vein with a Valsalva maneuver
* postthrombotic anatomical anomalies with B-mode ultrasound in the common femoral, femoral (former superficial femoral) and deep femoral veins.
2- With the patient standing on a phlebology step stool, with weight-bearing on a handrail, knees slightly flexed and muscles relaxed, the examiner will look for reflux in the femoral and popliteal veins, and then in the calf veins, by exerting manual compression on the calf. Different investigation protocols have been proposed. Some teams investigate patients in the supine position, and in the Trendelenburg position.12 But a consensus has emerged for the need to look for venous reflux in standing patients.10 The use of a compression sleeve allows standardization of the method and enables a reproducible duration of reflux to be obtained.10 However, manual compression is unquestionably more suitable for everyday practice and several authors have emphasized that the sensitivity of this method is comparable to that of pneumatic compression.8,10,13
3- The patient is then examined seated on the edge of the examining table8,9 with his feet resting on a stool. By compressing the base of the calf, the examiner will look for reflux in the various deep veins of the leg.
B- Investigation of the superficial venous network and the perforator veins
Investigation of the superficial venous network in a patient presenting with a post-surgical recurrent varicose vein should be precise and thorough. The origin of deep vein reflux into the superficial venous network is identified, attentively examining the former saphenofemoral and saphenopopliteal junctions and the perforator veins, and a complete, anatomical and hemodynamic evaluation is made of the varicose vein network, using the new anatomical nomenclature to describe it.14
There is no consensus on quantification of venous reflux. We consider that a vein in the superficial venous network is varicose when its diameter, measured with B-mode ultrasound in transverse section, is greater than 3 mm, and when, after a compression test of the muscles upstream or a Valsalva maneuver, it presents reflux of duration greater than or equal to 0.5 seconds.10 Like most authors, we consider that a perforator vein is incompetent when, after manual compression of the lower one-third of the thigh or of the leg, there is reflux of duration greater than or equal to 0.5 seconds15, although a recent study has suggested that this figure can be decreased to 0.35 seconds.10 As in the case of screening to detect deep vein reflux, the patient was examined standing10 and then seated on the edge of the examining table with his feet resting on a stool, to investigate the perforator veins in the lower calf.
1- At the former saphenofemoral junction, incomplete or distant GSV stripping (crossectomy) should be differentiated from neovascularization. The description of the different types of neovascularization observed is beyond the scope of this protocol4,16-19. Duplex ultrasound investigates the collateral veins, which drain the abdominal wall and the pelvis (superficial epigastric vein, superficial external pudendal vein, deep pudendal vein, superficial iliac circumflex vein).
2- In the thigh, duplex ultrasound looks for leakage points in the perineal veins, which are often the origin of varicose vein recurrence in the medial aspect of the thigh, and the perforator veins, which can run along the entire length of the thigh, with special attention given to the perforators in the femoral canal (Figure 3). The perforator vein can be centered, but often the anatomy is more complicated.20
3- In the popliteal fossa, duplex ultrasound identifies the mechanism of the recurrence4,9,21 whose description is also beyond the scope of this protocol.
4- In the leg, the different perforator veins (Figure 4) can be the origin of recurrent varicose veins.
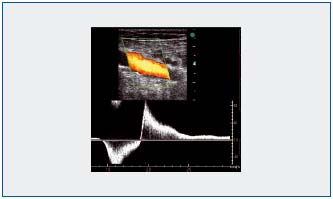
Figure 3: Identification with color duplex ultrasound of an incontinent perforator vein in the femoral canal.
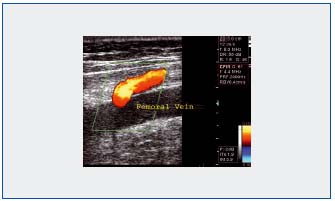
Figure 4: Identification with color duplex ultrasound of an incontinent calf perforator vein.
REFERENCES
Duplex ultrasound has become the investigation of reference in patients presenting with a recurrence of varicose veins after surgery. It should be thorough, investigate the totality of the different venous networks, and should be carried out following a strict protocol. It then allows a precise, anatomical, and hemodynamic diagnosis of post-surgical varicose vein recurrence.
REFERENCES
2. Myers KA, Zeng GH, Zliegenbein RW, Matthews PG. Duplex ultrasound scanning for chronic venous disease: recurrent varicose veins in the thigh after surgery to the long saphenous vein. Phlebology. 1996;11:125-131.
3. De Maeseneer MG, Tielliu IF, Van Schil PE, De Hert SG, Eyskens EJ. Clinical relevance of neovascularisation on duplex ultrasound in the long term follow up after varicose vein operation. Phlebology. 1999;14:118-122.
4. Gillet JL, Perrin M. Exploration échodoppler des récidives variqueuses post-chirurgicales. Angéiologie. 2004;56:26-31.
5. Crébassa V. Apports de nouvelles technologies ultrasonographiques dans les explorations des systèmes veineux superficiels. Phlébologie. 2006;59:221- 230.
6. Perrin M, Gillet JL, Guex JJ (in French). Syndrome post-thrombotique. Encycl Méd Chir (Elsevier SAS, Paris, tous droits réservés), Angéiologie. 2003;19- 2040,12p.
7. Perrin M, Gillet JL. Insuffisance valvulaire non post-thrombotique du système veineux profond des membres inférieurs. Encycl Méd Chir, (Elsevier SAS, Paris, tous droits réservés) Angéiologie.2003;19-2020,6p.
8. Haenen JH, Janssen MCH, Van Lagen H et al. The postthrombotic syndrome in relation to venous hemodynamics, as measured by means of duplex scanning and strain-gauge plethysmography. J Vasc Surg. 1999;29:1071-1076.
9. Haenen JH, van Langen H, Janssen MCH, et al. Venous duplex scanning of the leg; range, variability and reproducibility. Clin Sci. 1999;96:271- 277.
10. Labropoulos N, Tiongson J, Tassiopoulos AK, Kang SS, Mansour MA, Baker WH. Definition of venous reflux in lower extremity veins. J Vasc Surg. 2003;38:793-798.
11. Gillet JL, Perrin M, Allaert FA. Clinical presentation and venous severity scoring of patients with extended deep axial venous reflux. J Vasc Surg. 2006;44:588-594.
12. Criqui MH, Jamosmos M, Fronek A, et al. Chronic Venous Disease in an Ethnically Diverse Population – The San Diego Population Study. Am J Epidemiol. 2003;158:448-456.
13. Sarin S, Sommerville K, Farrah J, Scurr JH, Coleridge Smith PD. Duplex ultrasonography for assessment of venous valvular function of the lower limb. Br J Surg. 1994;81:1591-1595.
14. Caggiati A, Bergan JJ, Gloviczki P, Jantet G, Wendell-Smith CP, Partsch H. Nomenclature of the veins of the lower limbs; An international interdisciplinary consensus statement. J Vasc Surg. 2002;36:416-422.
15. Sarin S, Scurr J.H., Coleridge-Smith P.D. Medial calf perforators in venous disease: the significance of outward flow. J Vasc Surg. 1992;16:40-46.
16. Van Rij AM, Jones GT, Hill GB, Jiang P. Neovascularization and recurrent varicose veins: more histologic and ultrasound evidence. J Vasc Surg. 2004;40:296-302.
17. Stucker M, Netz K, Breuckmann F, Altmeyer P, Mumme A. Histomorphologic classification of recurrent saphenofemoral reflux. J Vasc Surg. 2004;39:816-821.
18. Fischer R., Linde N., Duff C., Jeanneret C., Chandler JG., Seeber P. Late recurrent saphenofemoral junction reflux after ligation stripping of the greater saphenous vein. J Vasc Surg. 2001;34:236-240.
19. Perrin M, Gillet JL. Récidive de varices à l’aine et à la fosse poplitée après traitement chirurgical. J Mal Vasc. 2006;31:236-246.
20. Rettori R, Franco G. Récidives variqueuses au niveau du canal fémoral après chirurgie de la veine saphène interne. J Mal Vasc. 1998;23:61-66.
21. Creton D. 125 réinterventions pour récidives variqueuses poplitées après exérèse de la petite saphène. Hypothèses anatomiques et physiologiques du mécanisme de la récidive. J Mal Vasc. 1999;24:30-36.
22. Perrin M, Gillet JL. Management of recurrent varices at the popliteal fossa after surgical treatment. Phlebology. 2008;23:64-68.
