Duplex ultrasound as first-line imaging for morphology and hemodynamics in the upper limb venous system
Charlotte STRANDBERG,2 MD
1Vascular Department, Gentofte Hospital
and Rigshospitalet,
University of Copenhagen, Denmark;
2Department of Radiology, Gentofte and
Herlev Hospital, Copenhagen, Denmark
Abstract
This review describes venous anatomy and hemodynamic characteristics for venous return in the upper limb, including main differences in comparison with venous drainage in the lower limb. Duplex ultrasound (DUS) is the first-line imaging modality even it seems less standardized than other investigation approaches for veins in the lower limb. This article presents useful instructions to assess veins from the peripheral to the thoracic outlet via the costoscalene hiatus. Without basic understanding, it is even more difficult to diagnose acute and chronic changes, such as deep-vein thrombosis (DVT), by far the most frequent disease, considered primary idiopathic or effort-induced (Paget-Schroetter syndrome), and secondary after central venous cannulation if cancer-related. Furthermore, imaging with DUS is also indispensable for assessing the usefulness of superficial veins for arteriovenous fistula and sometimes as a conduit for arterial bypass. Computed tomography venography (CTV) and magnetic resonance venography (MRV) should be offered if DUS is inconclusive due to obesity and/or technical problems and in cases with normal DUS despite strong suspicion of disease.
Introduction
The venous system in the upper limb has not attracted the same amount of attention as the venous system in the lower limbs. The hemodynamic influence, owing to lower involvement of gravity and limb weight, is less pronounced, as are complications after acute thrombosis, which do not exhibit the same clinical impact in the long run as observed in lower limbs. Although thrombosis in the upper limbs, either superficial or deep, plays a lessor role than deep-vein thrombosis (DVT) in the lower limbs, it is important to know how the venous system is constructed and how the venous return functions under normal conditions. Furthermore, such knowledge is useful for clinicians performing procedures that require vein access such as making arteriovenous (av) fistula for dialysis or for implanting feeding catheters and other devices for cardiac use. In some cases, arm veins are useful as bypass material for chronic arterial disease and, even more seldom, are used for segmental vein transplantation in case of chronic valve incompetence in the lower limb.
Duplex ultrasound (DUS) is useful as a first-line imaging modality for all these tasks.1 In general, DUS examination in the upper limb is more difficult than in the lower limbs. It is advisable to compare findings with those from a normal site from the opposite side in case of doubt. Otherwise, another imaging modality is needed.
Anatomy
Like in the lower limbs, the venous system in the upper limbs is composed of superficial and deep veins. Perforating connections in the arm system are few and unimportant. Both systems have valves, which play a minor role owing to a less-pronounced influence of gravity than in the lower limb. Such valves are absent in the most central veins. The shoulder region is filled with various vein connections that allow development of collaterals as an important return possibility in a postthrombotic stage.2
Superficial veins
The cephalic and basilic veins arise from the dorsal venous plexus of the hand and the palmar part, respectively. The cephalic vein runs along the anterior aspect of the forearm and hereafter in a lateral direction into the deltopectoral groove ending through the clavipectoral fascia into the axillary vein. The basilic vein runs on the ulnar side of the forearm and connects with the brachial vein midway along the upper arm. The two systems are connected in the cubital region with the median cubital vein, which is inconstant in location.
Deep veins
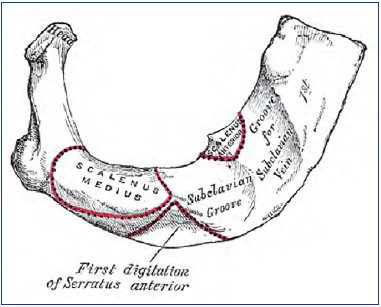
The ulnar, radial, brachial veins are often paired and run along the arteries. The axillary vein begins at the border of the teres major muscle and continues at the border of the first rib into the subclavian vein entering the thoracic aperture. Connecting to the internal jugular vein at the medial border of the scalenus anterior muscle, the vein is named the brachiocephalic vein, and hereafter receiving the vein from the opposite side to be named the superior vena cava behind the first right costal cartilage. Two ribs further distally, the cava inters the right atrium. Grooves are typically found on the upper surface of the first rib with imprint of the vein going anterior and the artery going behind the anterior scalenus muscle (Figure 1).
Azygos veins
Two veins constitute this system. The azygos vein is placed on the right side of the vertebral column, arising from the renal veins, and enters the superior vena cava from behind. The hemiazygos vein lies on the left side of the vertebral column and connects to the azygos vein at the level of the eighth thoracic vertebra. An accessory azygos vein continues on the left side and enters the left brachiocephalic vein. The azygos veins play an important role for collateral drainage in case of obstruction in the inferior vena cava, as well as in the superior vena cava, for which reason the system is mentioned here, even though not accessible for DUS.3
The thoracic outlet
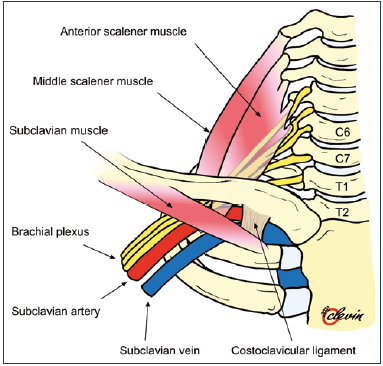
The term thoracic outlet is used to describe the passage of nerves, arteries, and veins between the thorax and the region of the shoulder. It is actually called the inlet passage, addressing the veins. The subclavian vein is surrounded by the first rib and pleura at the bottom, posteriorly by the scalenus anterior muscle, medially by the costoclavicular joint and ligament, and anteriorly by the clavicle with the subclavian muscle (Figure 2). This passage has more or less of a congenital narrowing, and in 70% of all individuals, a stenosis can be visualized by venography, especially with the arm in hyper abduction. Another cause of stenosis is related to muscular enlargement. Another term is the thoracic outlet syndrome (TOS), referring to symptoms from compression of the nerves and arteries as well as veins passing through this region.4 The Paget-Schroetter syndrome refers to vein thrombosis in the axillary and/or subclavian vein after strenuous arm exercise or repetitive effort.5
Hemodynamics
Normal veins
The venous return in a supine position is a result of a slightly higher pressure post capillary in the hand than in the right atrium. It is obvious that the importance of gravity is less pronounced in this extremity. In a standing position with the arm in a neutral hanging position, the hydrostatic pressure in the hand is about 45 mm Hg in a person of normal height, thus much lower than in the lower limb. Involuntary muscle activity and, of course, active movements act as a venous pump, as we know from the pumping principles in the lower limbs. The hydrostatic pressure facilitates flow to the atrium in an arm elevated above horizontal level. The return is also influenced by the respiratory pressure changes during inspiration and expiration with enhanced return during expiration.3 Veins in an elevated arm over the head are visualized as nearly collapsed, whereas the veins in the opposite position are more elliptical in form.6
Vein pathology
Acute thrombosis is characterized by venous stasis with decreased flow distal to the occlusion without any collaterals. In a post-thrombotic state, the veins are more or less occlusive, with caliber-varying flow channels; collateral flow is seen as another sign along with reflux, which can be demonstrated in a hanging arm by release of compression with retrograde filling distal to the compression point. The test for reflux can also be done with a powerful and firm handshake. The most important factor for pathophysiological changes in the upper limbs is the obstructive element, because valve incompetence is of less importance owing to the less-pronounced involvement of gravity than in the lower limbs.
Duplex ultrasound (DUS)
DUS is the most used imaging modality because it gives morphological and hemodynamic information at the same time. The patient is placed in a supine position with the arm relaxed and slightly abducted and rotated laterally, and the head slightly turned to the opposite side. A high frequency linear transducer, typically 7.5-14 MHz, is used, but sometimes a 5-MHz curved array transducer is used for the subclavian vein. Both color Doppler and spectral Doppler are required for optimal flow assessment. As mentioned, other modalities such as computed tomography venography (CTV) and magnetic resonance venography (MRV) are helpful if DUS is inconclusive and/or imaging to determine etiology in adjacent structures is needed.
DUS of normal veins, morphology
A routine investigation of vein morphology begins at the level of the cubital region, whereas the veins in the forearm only are of importance for creating an av fistula at that level. The cephalic, basilic, and cubital veins are examined in a transverse scan plane, whereas the brachial and axillary veins are examined in the longitudinal and transverse scan plane. Normal veins are elliptical and easy to compress. The lateral part of the subclavian vein is investigated via an infraclavicular approach and the medial part via a supraclavicular view. It is not usually possible to compress this vein. The internal jugular vein is easy to identify and followed in the transverse plane to the junction with the subclavian vein. The brachiocephalic vein can be evaluated via a suprasternal approach with a minor high-frequency curved-array probe, which can also be used for larger individuals. It is not always easy to visualize the superior vena cava (Figures 3-5).
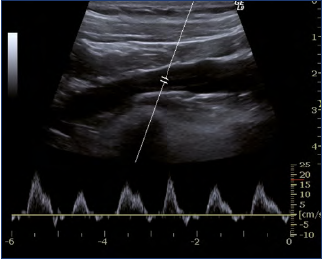
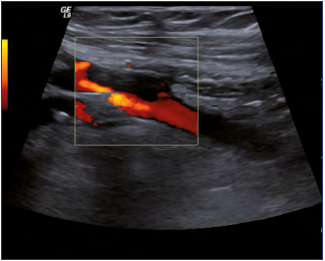
DUS of normal veins, waveform
The spectral Doppler waveform is characterized by a pulsatile configuration in the central veins (Figure 6). The action of the right atrium is reflected back and is manifested as a biphasic flow pattern with a flow peak forward in mid diastole, whereas the flow slows or reverses as the tricuspid heart valve closes. The respiratory phasicity is also reflected into the waveform, increased during inspiration and decreased during expiration (Figure 7). The influence of the heart and the respiration is less pronounced the more peripherally the examination is performed.
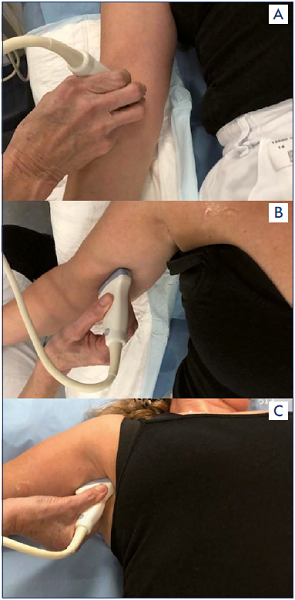
Figure 3A-3C. A linear transducer typically 7.5-14 MHz searching for the median cubital, brachial and axillary vein.
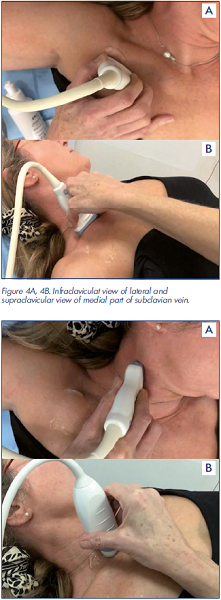
Figure 4A, 4B. Infraclaviculat view of lateral and supraclavicular view of medial part of subclavian vein.
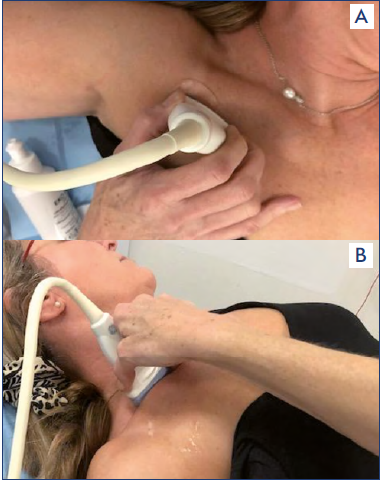
Figure 4A, 4B. Infraclaviculat view of lateral and supraclavicular view of medial part of subclavian vein.

Figure 5A, 5B. The Jugular vein. The brachiocephalic vein and cava visualized with 5 MHz curved array transducer.
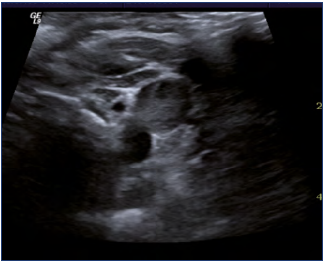
DUS of thrombosis
Thrombosis in the upper limb counts for about 5% of total DVT incidence, secondary being most frequent.7 The examination for thrombosis concerns location, extension, compressibility, and flow. The B-mode modification can demonstrate the appearance of a hypo- or hyper-echogenic thrombus (depending on thrombus age) combined with noncompressible, except in very small nonocclusive thrombus and dilated vein structures (Figures 8, 9). The central veins such as the subclavian and brachiocephalic veins are also almost impossible to compress. Therefore, color flow imaging or spectral analysis is essential for diagnosis.
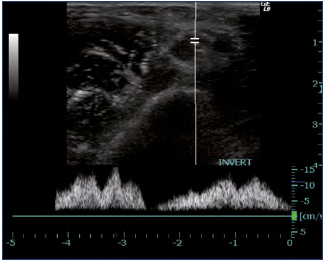
The absence of a Doppler signal means there is a thrombus. Hampered cardiac or respiratory fluctuations as well as lack of flow augmentation after distal compression raises suspicion of a central blockage (Figure 10).8 In general, the sensitivity and specificity for detection of DVT with DUS was concluded on the basis of 11 studies in comparison with venography as reference, to be greater than 90%.9 In a postthrombotic stage, color Doppler makes possible the visualization of the recanalized veins with internal channels in addition to small-caliber veins with noncompressible, thickened walls, and foci of echogenic thrombi may be seen. The spectral appearance in a stenosis typically shows accentuated turbulent and pulsatile flow. Multiple visible collateral veins point out chronic obstruction in the central veins.
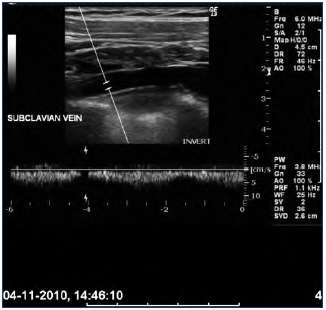
Figure 10. Doppler curve with lack of pulsatile flow in the
subclavian vein indicating a more central obstruction.
Limitations with
DUS Duplicated veins, hypovolemia, obesity, and edema may limit the quality of the examination. The fact that the hemodynamics do change with different arm positions can make the interpretation difficult. A recent publication has demonstrated false negative findings with DUS in 21% of patients with suspected thrombosis. The group of patients in this investigation had primary DVT episodes with subclavian vein thrombosis due to TOS as a more difficult diagnosis. The interpretation means use of CTV/ MRV should be encouraged in case of negative results in patients having idiopathic/primary arm thrombosis.10
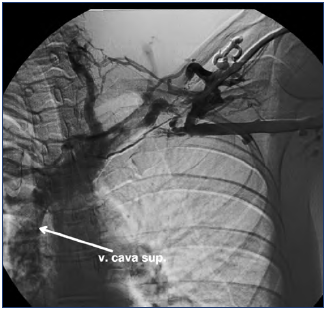
Other modalities
Phlebography
This imaging modality was considered the “gold standard” for diagnosing acute thrombosis 15-20 years ago (Figure 11). It is preferable to administer the contrast medium in the deep veins, which can be difficult. The axillary vein can be overlooked if the contrast medium is injected in the cephalic vein. The procedure is usually painful as well. DUS has overcome all these disadvantages.
Chest radiography
Chest radiography can be useful when suspicion of underlying disease arises; eg, cervical rib, extreme callus after fracture of the clavicula, and seldomly, some osteal malformations all causing secondary thrombosis.
Computed tomography venography (CTV)
Multiple spiral CTV with 3D reconstructions is an ideal minimal invasive technique for rapid venous assessment. Bilateral arm injection is optimal for visualizing the central veins, including superior vena cava. However, this tool has limitations such as requirement for radiation and the possible occurrence of allergic reactions to the iodinated contrast medium.11
Magnetic resonance venography (MRV)
This modality with and without contrast medium is an alternative method if DUS is inconclusive; it is used for central veins.12 Limitations involve claustrophobia (which may be triggered in some patients) and those involving the presence of metallic devices.12,13
Conclusion
DUS is a rapid and repeatable method for examination of the veins in the upper limbs. It is a first-line imaging method for diagnosing DVT, either primary or secondary, as well as postthrombotic changes. CTV and MRV are mandatory alternatives if DUS is technically insufficient and if DUS results are normal despite strong suspicion of disease. Knowledge of the normal anatomy is also useful for deciding if the veins can be used for different access strategies and av fistula. There is notable absence of a consensus document for DUS in the upper limbs such as we have for this imaging modality in the lower limbs.14
REFERENCES
1. Chin EE, Zimmerman PT, Grant EG. Sonographic evaluation of upper extremity deep venous thrombosis. J Ultrasound Med. 2005;24:829-838.
2. Gloviczki P, Mózes G. Development and anatomy of the venous system. In: Gloviczki P, ed. Handbook of Venous Disorders. London, UK: Arnold; 2009:12- 24.
3. Bækgaard N, Broholm R, Strandberg C. Anatomy, hemodaynamics and imaging of the upper extremity venous system. In: Wittens C, ed. Advances in Venous Therapy. Turin, Italy: Edizoni Minerva Medica; 2011:111-118.
4. Illig KA, Donahue D, Duncan A, et al. Reporting standards of the Society for Vascular Surgery for thoracic outlet syndrome. J Vasc Surg. 2016;64:23-35.
5. Illig KA, Doyle AJ. A comprehensive review of Paget-Schoetter syndrome. J Vasc Surg. 2010;51:1538-1547.
6. Meissner MH, Moneta G, Burnand K, et al. The hemodynamics and diagnosis of venous disease. J Vasc Surg. 2007;46:4S-24S.
7. Isma N, Svensson PJ, Gottsäter A, et al. Upper extremity deep venous thrombosis in the population-based Malmö thrombophilia study (MATS). Epidemiology, risk factors, recurrence risk, and mortality. Thromb Res. 2010;125:335-338.
8. Patel MC, Berman LH, Moss HA, et al. Subclavian and internal jugular veins at Doppler US: abnormal cardiac pulsatility and respiratory phasicity as a predictor of complete central occlusion. Radiology. 1999;211:579-583.
9. Kraaijpoel N, van Es N, Porreca E, et al. The diagnostic management of upper extremity deep vein thrombosis: a review of the literature. Thrombosis Res. 2017;156:54-59.
10. Brownie ER, Abuirqeba AA, Ohman JW, et al. False-negative upper extremity ultrasound in the initial evaluation of patients with suspected subclavian vein thrombosis due to thoracic outlet syndrome (Paget- Schroetter syndrome). J Vasc Surg: Venous and Lym Dis. 2020;8:118-126.
11. Sabharwal R, Boshell D, Vladuca P. Multi detector spiral CT venography in the diagnosis of upper extremity venous thrombosis. Australas Radiol. 2007;51: 3253-3256.
12. Lim RP, Hornsey E, Ranatunga D, et al. Upper extremity non-contrast magnetic resonance venography (MRV) compared to contrast enhanced MRV and ultrasound. Clin Imaging. 2017;45:51-57.
13. Baarslag HJ, van Beek EJR, Reekers JA. Magnetic resonance venography in consecutive patients with suspected thrombosis of the upper extremity: initial experience. Acta Radiol. 2004;45:38-43.
14. De Maeseneer M, Pichot O, Cavezzi A, et al. Duplex ultrasound investigation of the veins of the lower limbs after treatment for varicose veins – UIP consensus document. Union Internationale de Phlebologie. Eur J Vasc Endovasc Surg. 2011;42(1):89-102.