Endovenous laser ablation or radiofrequency ablation for varicose veins: a review
Robin Man KARMACHARYA, MS;
Satish VAIDYA, MS;
Prasesh DHAKAL, MBBS;
Niroj BHANDARI, MBBS;
Sahil BADE, MBBS;
Sohail BADE, MBBS;
Selene POKHAREL, MBBS;
Shreeja SHIKHRAKAR, MBBS;
Prabha SHRESTHA, MSN;
Department of Surgery, Dhulikhel Hospital,
Kathmandu University Hospital, Kavre,
Nepal
Abstract
Varicose veins are a part of chronic venous insufficiency syndrome, presenting with dilated veins, skin changes, and even ulceration in the lower limbs. Untreated, it can result in many complications and has an impact upon one’s quality of life. Management depends upon the stage and etiology of varicose veins. Conventional vein stripping surgery is now being replaced by minimally invasive modalities, among which endovenous laser ablation (EVLA) and radiofrequency ablation (RFA) are the mainstays of treatment. Each procedure has its own sets of procedural technique, variants, performance, outcomes, and complications. Here, we discuss the various aspects of EVLA and RFA on varicose vein treatment.
Introduction
Varicose veins are dilated tortuous veins that have significant impact on a person’s quality of life (QOL).sup1/ For ease of communication, clinical-etiology-anatomy-pathophysiology (CEAP) classification is used to clinically classify varicose veins.2 Treatment of varicose veins ranges from conservative management, pharmacotherapy, endovenous treatments, and surgery.
The size of the affected vessels determines the treatment modality—spider telangiectasias and reticular veins are best treated with foam sclerotherapy, thermocoagulation, and cutaneous lasers, whereas larger varicosities are preferably treated with surgery and microinvasive procedures, such as endovenous laser ablation (EVLA) and radiofrequency ablation (RFA).3 Nonthermal ablation techniques include sclerotherapy, glue, mechanochemical ablation (MOCA), and steam. They provide an advantage to patients with below-the-knee disease, owing to less risk of nerve injury or skin burn. MOCA is a hybrid process of using mechanical trauma and simultaneous sclerotherapy to ablate and treat varicose veins.4 Intradermal, subcutaneous, and perforator veins can be treated by chemical ablation of a varicose vein by intravenous injection of liquid or foam sclerosant via a method known as sclerotherapy.5 Cyanoacrylate glue can be used to ablate vessels as it polymerizes on contact with blood, causing vessel inflammation and fibrosis and occlusion, whereas the steam technique works via steam applied through the catheter canal, which releases thermal energy, causing vessel ablation and sclerosis.6 These are emerging technologies that are being explored for their use in varicose veins.
Owing to complications, such as bruising, postoperative pain, anesthesia complications, hematoma, saphenous nerve injury, and wound infection, conventional surgical stripping is gradually being replaced by new minimally invasive techniques like EVLA and RFA.7 Relevant contraindications of EVLA and RFA include an incompetent superficial vein diameter of less than 2 mm, history of extensive deep venous thrombosis (DVT) in the same leg, active superficial venous thrombosis in the vein to be treated, history of a prior surgical or endovenous treatment of the same leg, pregnancy, known malignancy and systemic conditions resulting in overall poor health, frailty, immobility, and known bleeding or clotting disorders.8 Various scores are used for assessment of severity and impact of varicose veins such as the Aberdeen Varicose Vein Questionnaire (AVVQ), the Aberdeen Varicose Vein Severity Score (AVVSS), the Chronic Venous Insufficiency Questionnaire (CIVIQ-2), health-related QOL (HRQOL), the Venous Clinical Severity Score (VCSS), and the Visual Analog Scale (VAS) for pain. We have described some of the outcomes with these scores.
Although both EVLA and RFA follow the principle of thermal ablation of varicose veins, there are fundamental differences in mechanism of ablation, devices used, procedure, outcomes, and complications. Here we discuss the principles and differences between EVLA and RFA techniques for the treatment of varicose veins.
Endovenous laser ablation
EVLA is a minimal invasive procedure in which a percutaneous laser fiber is introduced within the incompetent varicose vein resulting in nonthrombotic occlusion and inflammation of the vein.7 The major mechanism of EVLA is the conversion of absorbed light energy into heat either through direct absorption of the laser power emitted from the fiber into the blood and perivenous tissues or through direct contact between the fiber tip and the vein wall.9
EVLA is indicated in an ambulatory patient with great, small, or accessory saphenous vein reflux with surface varices, and/ or symptoms or complications related to superficial venous insufficiency. It can be used in all stages of varicose veins.10 Studies have shown better resolution of venous ulcers with EVLA. So, for stage C5 and C6 varicose veins, EVLA is generally preferred over RFA.7 EVLA can also be done in tributaries of sufficient length.11
Operative procedure
Although it is a common practice to have an institutional operative protocol for EVLA and RFA, it’s mainly based on steps learned during training and on publications mentioning the procedures. The protocol is often tailored to the institution based on the experience with the procedures. Preoperative planning for these procedures along with access site determination is generally done by mapping the hemodynamic status of the veins via an ultrasound before and during the procedure.
EVLA is routinely performed using dilute local anesthesia, with or without supplemental oral anxiolytics, in an office setting. Buffered local tumescent anesthesia, especially cold tumescence, along with general anesthesia (GA) has shown improved immediate postoperative pain in EVLA compared with GA only.12-14 Bupivacaine used in tumescent solution had a better outcome than the use of lidocaine and prilocaine.15
Generally taking 30-60 minutes to perform, procedure times are dependent on the length of segment treated, experience of the operator, and whether ancillary procedures, such as ambulatory phlebectomy, are done.10 For better results, it is necessary to empty the veins by external compression and Trendelenburg positioning.16,17 After positioning, the great saphenous vein (GSV) is cannulated by EVLA laser fiber. A study mentioning protocol on EVLA mentions 100 J/cm delivered empirically to the first 3 cm distal to the saphenofemoral junction (SFJ) and 40 J/cm in remaining segments.18 Regardless of how underlying saphenous incompetence is treated, ancillary treatments, such as sclerotherapy and phlebectomy, along with compression, are typically needed to treat residual varices.10
The use of elastic compression stockings after EVLA has shown reduced severity of pain and edema postoperatively.19,20 Use of compression stockings for longer than 2 days and eccentric compression applied by a new crossed-tape technique is suggested after the procedure.21,22
Endovenous laser ablation variants
Commonly used laser ablator devices are the Biolitec laser machine (Biolitec), VenaCure EVLT System (Angiodynamics), Diomed D15plus (Diomed, Inc., Andover, MA), etc.7 A popular dedicated laser fiber for EVLA has a wavelength of 1470 nm, 980 nm, 940 nm, or 840 nm in power settings of 3-12watts. Pullback speed is adjusted to 1-4 mm/s. Thus, the combination of higher power and lower pullback velocity leads to maximum burn of the veins. Maximum temperature ranges from 91 °C to 97 °C. EVLA using a shorter wavelength (usually 980 nm) has a higher temperature by about 10 °C.9
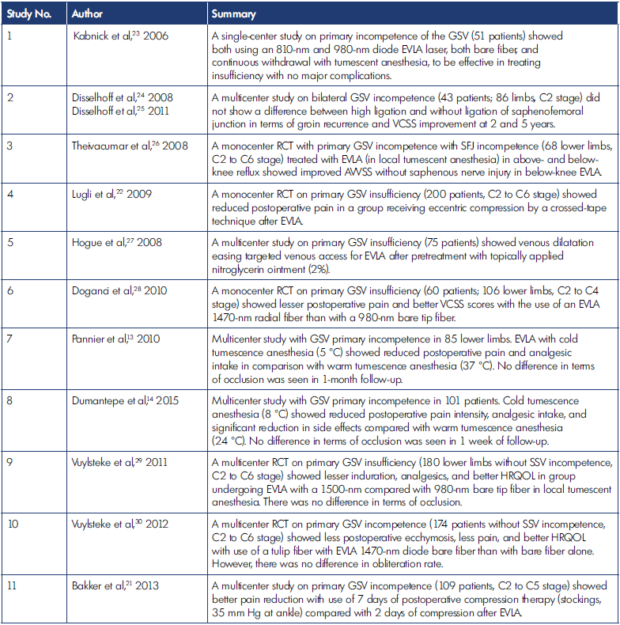
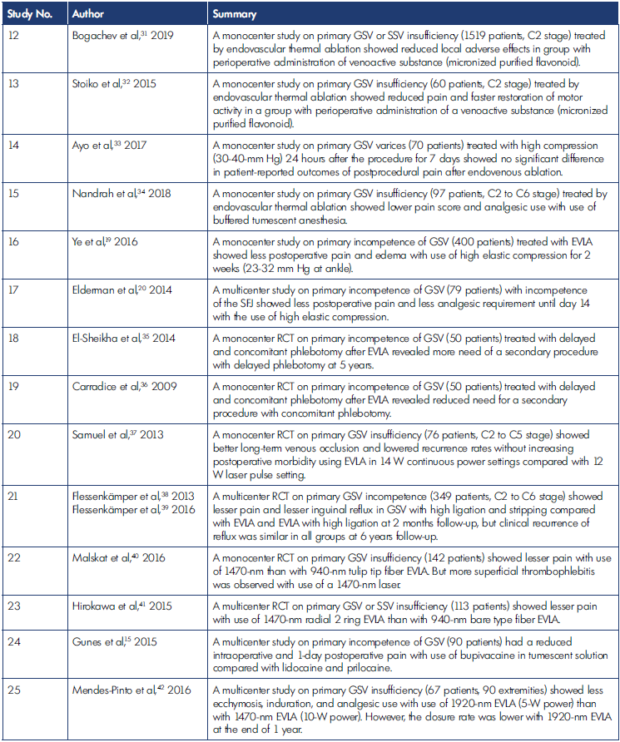
Table I. Endovenous laser ablation (EVLA) outcomes.
AVVSS, Aberdeen Varicose Vein Severity Score; EVLA, endovenous laser ablation; GSV, great saphenous vein; HRQOL, healthrelated quality of life; RCT, randomized controlled trial; SFJ, saphenofemoral junction; SSV, short saphenous vein; VCSS, Venous Clinical Severity Score.
Different variants of treatment with EVLA have been explored through various randomized controlled trials (RCTs) and other studies (Table I).13-15,19-42 When contrasting different methods of EVLA, in relation to the fibers, lesser induration and lesser postoperative pain along with better VCSS score was seen with higher wavelength of EVLA than with lower wavelength EVLA.28,29,41 However, a higher chance of superficial thrombophlebitis was seen more with EVLA 1470 nm than EVLA 940 nm.40 Reduced chance of postoperative ecchymosis and pain was seen with the EVLA tulip fiber.30 In a study of EVLA wavelengths, at 4 weeks, both laser wavelengths were successful in curing GSV insufficiency (810 nm and 980 nm), and 1 study also showed that below-knee EVLA was not associated with saphenous nerve injury.23,43 Also, EVLA done with nitroglycerin produced a statistically significant venous dilatation, easing targeted venous access.27
The limitation of EVLA is the need for uniform pullback or adjustable pullback for segments with perforators in varicose veins, which is difficult to standardize. This can result in incomplete burning or excessive burning.9
Radiofrequency ablation
RFA involves insertion of the RFA catheter inside the varicose vein that causes spasm of the vessel, ablation of endothelium of the vessel, and complete closure of the defective vein.44 Radiofrequency waves are electromagnetic energy within a frequency range of 300 kHz to 1 MHz. The wave causes vibration and friction of atoms, resulting in thermal energy. The procedure was introduced in 1999; since then, the procedure has been gaining widespread acceptance and availability.11
RFA can be used in all stages of varicose veins; but in stage C5 and C6, RFA is found to be slightly inferior to EVLA.7 Also, RFA can be combined with concomitant phlebectomy of tributaries.45 Major advantages of this technology are cosmetically better procedures, less pain, early return to work, less scar, and less chance of infection.46
Operative procedure
Preoperative mapping is done as for EVLA, and access site is determined. RFA too can be done under general, regional, or tumescent local anesthesia (under ultrasound guidance), and the Trendelenburg position can be used to achieve maximum vein collapse. The distance between the RFA catheter tip and SFJ should be at least 2 cm, and tumescent anesthesia is injected between GSV and skin with ultrasound guidance. There is a “standard technique,” where heating treatment is done at 85 C, in which the first 5.0 cm of saphenous vein is ablated at 1.0 cm per minute followed by the remainder of the GSV being ablated at 1 cm per 30 seconds, or “modified technique,” in which the first 5.0 cm of saphenous vein is heated and ablated at 1.0 cm per minute with the generator set at 90 °C after which the catheter is slowly and continuously pulled back at a rate of 1 cm per 20 seconds, which maintains a vein wall temperature of 90 °C. In both techniques, there is 0.5-cm overlap of each pair of segments, and the pullback is continuous until the desired vessel length is treated. When the final segment is treated, pulling off the heating element of the catheter into the sheath is avoided because it might melt the sheath. Usually, double ablation is done in the segment 2 cm distal to the SFJ, and adjunct sclerotherapy is done for residual veins.47
There have also been studies on the use of venoactive drugs during the perioperative period to reduce pain and enhance recovery.32 Use of micronized purified flavonoid fraction (MPFF)—a venoactive drug—in the perioperative period showed reduction in pain, ecchymosis, paresthesia, pigmentation and heat-induced thrombosis, and enhanced recovery after endovenous ablation.31,32
In recent trials, postoperative compression by superposition of stocking class I and class II after RFA under local tumescent anesthesia when done for 4 hours had lesser complications and greater reduction in leg volume then compression for 72 hours; there was no difference in venous occlusion, postoperative pain, and time to full recovery with and without postoperative compression in RFA.33,48-50
Radiofrequency ablation variants
Popular RFA generator devices are the ClosureFast RFA system (Medtronic) preceded by the ClosurePlus catheter, Olympus Celon RFITT (Olympus Medical Systems, Hamburg, Germany), and CelonLab POWER radiofrequency generator (Celon AG Medical Instruments, Teltow, Germany); 7,11,51 One popular RFA device is the VNUS ClosureFast device that uses RFA catheters of 60- and 100-cm lengths and which has a heating segment of 7 cm. The temperature attained during RFA is 120 °C with a duration of 20 seconds. Usual watt requirement is 10 to 20 watts. The second generation of RFA catheters, the ClosureFast was designed to improve on procedural deficiencies such as length of time and ease of the procedure. They use a segmental approach to ablation and involve activating the heating element for 20-second cycles. The heat is then automatically shut off, and the catheter is repositioned to the next treatment zone indicated by shaft markers on the catheter. The new catheter also no longer needs the saline drip and eliminates the high impedance issues caused by coagulum build up with the previous catheter. The segmental approach, sometimes referred to as segmental RFA ablation also speeds up the procedure and decreases the variability in dose delivered to the tissue. The new design also involved changes in the method of energy delivery in that the energy field was now shielded and an electrical field is not produced in the tissue, thereby reducing the potential concerns for interference with other indwelling devices, such as pacemakers, etc.52 They are very accurate to attain 120 °C within 3 seconds by varying wattage from 15 to 40 watts. Any deviation from this watt range and temperature will stop the radiofrequency cycle and will prompt a warning. This allows RFA to be more uniform and safer during the procedure.11
Various studies have compared different RFA devices and their outcomes (Table II).45,48-50,53-55 When different RFA technologies—VeneFit, radiofrequency induced thermal therapy (RFITT), and endovenous radiofrequency (EVRF)— were compared, mean treatment time was faster in RFITT; pain score/discomfort at 2 weeks differed in that fewer in the EVRF group reported no problems. However, there was no difference in clinical outcome when compared at 6 and 12 months. Truncal ablation failure at 12 months was lesser with VeneFit.55 Comparisons have also been made between direct RFA (dRFA; radiofrequency-induced thermotherapy) and indirect RFA (iRFA; VNUS ClosureFast) in which primary GSV occlusion rates were better after iRFA and EVLA than with dRFA.53 In another study, the F-care (EVRF, F Care Systems, Antwerp, Belgium) method was safe and fast, but the 1-year closure rate was significantly lower than with the conventional endovenous RFA ClosureFast method.54
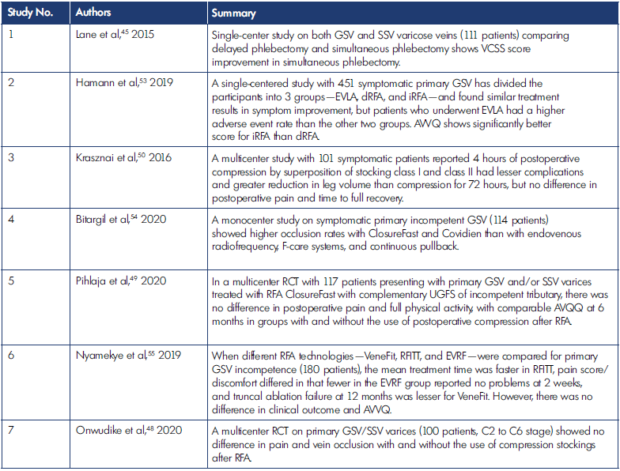
Table II. Radiofrequency (RFA) outcomes.
AVVQ, Aberdeen Varicose Vein Questionnaire; dRFA, direct radiofrequency ablation; EVLA, endovenous laser ablation; EVRF, endovenous radiofrequency; GSV, great saphenous vein; iRFA, indirect radiofrequency ablation; RCT, randomized controlled trial; RFA, radiofrequency ablation; RFITT, radiofrequency induced thermal therapy; SSV, short saphenous vein; UGFS, ultrasound-guided foam sclerotherapy; VCSS, Venous Clinical Severity Score.
The limiting factor for RFA is the need for a special setup including RFA generator and RFA catheter, which is costly relative to conventional open surgery. Also, it takes special training and familiarization with the setup and technique to properly perform surgery. There is a learning curve, with possibility of minor to major complications.46 RFA can only be done in the main saphenous system, such as GSV and short saphenous vein, and not in the tributaries.11 Veins that are too small or tortuous for catheter access or too large to successfully ablate would not be appropriate for treatment via RFA.52
Discussion
Both EVLA and RFA are shown to be comparable to conventional vein stripping surgery and are advantageous in terms of being minimally invasive, with lesser postoperative complications. Many studies have been done comparing various aspects of EVLA and RFA, addressing pros and cons of both (Table III).53,56-63 Although there were no sharp demarcations regarding use of EVLA and RFA preferencing one over the other, we have tried to explore their differences and variations in use (Table IV).7,9,11,16,17,56,64
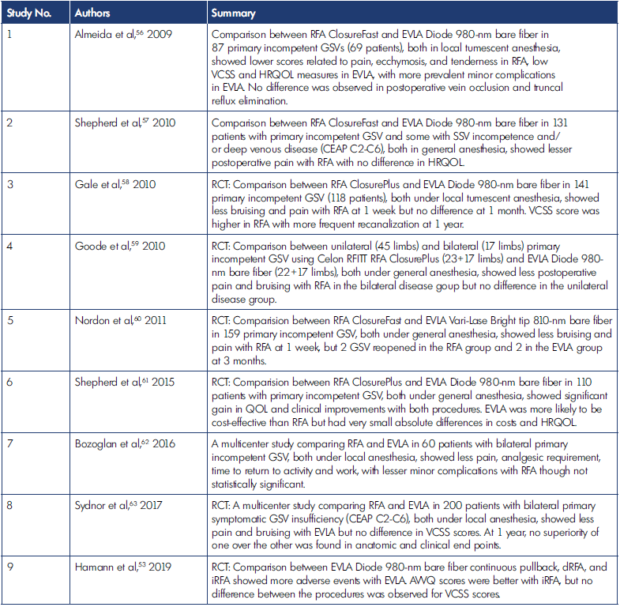
Table III. Comparison between endovenous laser ablation (EVLA) and radiofrequency (RFA) for varicose veins.
AVVQ, Aberdeen Varicose Vein Questionnaire; dRFA, direct radiofrequency ablation; EVLA, endovenous laser ablation; EVRF, endovenous radiofrequency; GSV, great saphenous vein; HRQOL, health-related quality of life; iRFA, indirect radiofrequency ablation; QOL, quality of life; RCT, randomized controlled trial; RFA, radiofrequency ablation; RFITT, radiofrequency induced thermal therapy; SSV, short saphenous vein; VCSS, Venous Clinical Severity Score.
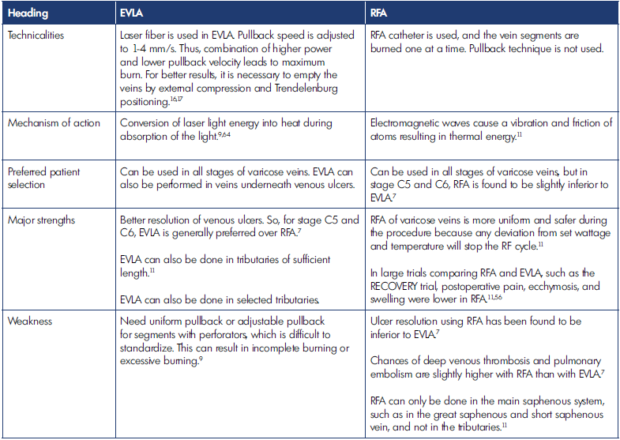
Table IV. Major details on endovenous laser ablation (EVLA) and radiofrequency (RFA).
EVLA, endovenous laser ablation; RECOVERY, Radiofrequency Endovenous ClosureFAST versus Laser Ablation for the Treatment of Great Saphenous Reflux trial; RF, radiofrequency; RFA, radiofrequency ablation.
Cost
RFA and EVLA have the extra upfront cost of the generator and cost per case for disposables. In some cases, these can be done outside the operation theater without anesthetist or surgical assistant fees.52 RFA performed in the operating room was associated with net loss per case vs office-based interventions.65 However, even though the initial setup cost was high, a cost analysis from hospitals in Michigan show that in the long run, treatment with vein stripping was associated with higher costs than RFA and EVLA. Another cost-effective analysis from the United Kingdom also showed that RFA had the highest median rank for net benefit, with MOCA second and EVLA third among varicose vein treatment options.66 In low-resource settings, reusing the RFA catheter can also be one means for cost cutting. A study from India has shown promising results in terms of vein occlusion rates and cost cutting when the RFA catheter was reused.67 Further studies on catheter-based interventions in an office setting and on reuse of catheters can significantly reduce the cost for treatment.
Technicalities
Although RFA and EVLA both cause thermal ablation, the mechanism of action and resulting technicality of thermal ablation is different between these 2 techniques. RFA causes a circular, homogeneous lesion, and there is no perforation of the venous wall. Whereas in laser ablation, the light energy is transmitted into heat energy, causing vascular wall disruption and venous wall perforation. The difference was studied in multiple experimental studies.68,69 These could be the reasons for lesser postoperative pain in RFA patients. Also, RFA seems to be more dependent on adequate vein emptying, use of tumescent anesthesia, and compression techniques than EVLA techniques, which do not depend on vein wall contact.52 But for even better results after EVLA, it was necessary to empty the veins by external compression and Trendelenburg positioning in EVLA too.16,17 Use of buffered tumescent anesthesia (to physiologic pH) has shown lower pain scores and analgesic use after endovascular procedures.34
In relation to ease of procedure and uniformity of the ablation, RFA is much more comfortable than EVLA as there is a segmental approach of ablation and the energy automatically stops after the standard duration in desired temperature.52 This has made learning hands-on skills to do RFA and following the standard operating protocol much easier. In addition, the RFA catheter is much sturdier than the EVLA catheter, and there are lesser chances of physical damage to the RFA catheter during the procedure. Although not recommended, there is more possibility of reusing the RFA catheter than the EVLA catheter.67
Technical success and redo rates
A study compared EVLA and RFA in patients with bilateral varicose veins where one limb received RFA as treatment and another limb received EVLA. Here, rate of recanalization was 6.8% in the RFA group, whereas that was not present in the EVLA group. Time to return to normal activity was 0.9 days in the EVLA group and 1.3 days in the RFA group.70 Similarly, higher technical success and low redo rates are found with use of EVLA as compared with RFA in a study from India.7 When first-generation RFA catheters were used, studies showed lower technical success and higher redo rates.71 Second-generation catheters using a segmental approach to ablation have improved technical ease, speed, and effectiveness of the RFA devices.
Outcomes and complications
Many comparative studies have shown similar outcomes between EVLA and RFA in terms of safety and efficacy, including vein ablated length, GSV occlusion, pain scores, QOL, and complications after the procedures—thrombophlebitis, hematoma, edema, ecchymosis, paresthesia, and recanalization.72-74
There are trials and studies that find EVLA superior in terms of ulcer resolution, lesser skin complications, faster return to work, patient satisfaction, and less recanalization.7,74 EVLA has shorter procedure times and lower per treatment cost. Reported occlusion rates of EVLA generally are slightly higher than those obtained with RFA.10 However, return to work has also been found to be significantly sooner with RFA than with surgery, but not for EVLA, in a meta-analysis.75 This might result from different ablative mechanisms that can cause vein wall perforation with EVLA (810 and 980 nm with bare tip) but not RFA. This has led to evolution of a new 1470-nm EVLA procedure with a radial fiber that is claimed to cause less pain with similar short-term efficacy.28
A study has shown that chances of DVT and pulmonary embolism are slightly higher for RFA than EVLA.7 Large trials comparing RFA and EVLA, such as the RECOVERY trial (Radiofrequency Endovenous ClosureFAST versus Laser Ablation for the Treatment of Great Saphenous Reflux), also show that postoperative pain, ecchymosis, and swelling was lower in RFA.11,56 EVLA may include more bruising and discomfort in the early postoperative period, although this may be technique dependent.10 RFA has less periprocedural pain, analgesic requirement, and bruising. RFA has also been shown to have less technical failure and early recovery with less postoperative pain.59,76,77
Several meta-analyses have been done over time evaluating EVLA and RFA, but sufficient trials have not been done to give a more robust and significant answer for choosing between EVLA and RFA for varicose veins. Earlier analysis had shown both EVLA and RFA to be safe and comparable to surgical stripping with lesser procedural pain.72,78,79 EVLA had better short-term outcomes with more occlusion and less recanalizations.80 However, analysis of long-term follow-up of 5 years did not show a difference in outcomes between conventional surgery, EVLA, and RFA.81 A Cochrane review was done focusing on the methods of treatment of short saphenous veins only, which showed that EVLA had lower recanalization and recurrence of reflux than conventional surgery.82
Guidelines provided by various societies and forums are not very specific in their recommendations. The Society for Vascular Surgery and the American Venous Forum, in a guideline issued in 2011, mentioned the role of endovenous thermal ablation for treatment of incompetent saphenous vein, but a separate recommendation for EVLA or RFA was not mentioned.83 A recent guideline by the American Venous Forum in 2020 mentions the appropriateness of endovenous thermal ablation for stage C2 to C6 and does not recommended it for an earlier stage.36 It is considered appropriate is for GSV, SSV, and accessory veins. The recent report also does not separate recommendation for EVLA and RFA.
Conclusion
Although both RFA and EVLA are near equally good in a large proportion of varicose vein cases, there are some instances where one method is better than the other. The RFA device has a more robust mechanism for safety, making it easier for hands-on learning experience. EVLA has been used for all stages of varicose veins, including ulcers. Technical success and outcomes are similar for both the procedures, with lesser skin complications with RFA use. Larger clinical trials and more robust guidelines are required for all aspects of EVLA and RFA use.
REFERENCES
1. Branisteanu D-E, Feodor T, Baila S, Mitea I-A, Vittos O. Impact of chronic venous disease on quality of life: results of vein alarm study. Exp Ther Med. 2019;17(2):1091-1096.
2. Eklof B, Rutherford RB, Bergan JJ, et al. Revision of the CEAP classification for chronic venous disorders: consensus statement. J Vasc Surg. 2004;40(6):1248- 1252.
3. Kremastiotis J, Jfri A, Litvinov IV, Barolet D, Netchiporouk E. Treatment modalities for varicose veins of lower extremities. J Cutan Med Surg. 2020;24(2):203-204.
4. Vos CG, Unlu C, Bosma J, van Vlijmen CJ, de Nie AJ, Schreve MA. A systematic review and meta-analysis of two novel techniques of nonthermal endovenous ablation of the great saphenous vein. J Vasc Surg Venous Lymphat Disord. 2017;5(6):880-896.
5. Rabe E, Breu FX, Flessenkamper I, et al. Sclerotherapy in the treatment of varicose veins: S2k guideline of the Deutsche Gesellschaft fur Phlebologie (DGP) in cooperation with the following societies: DDG, DGA, DGG, BVP. Hautarzt. 2021;2(suppl 2):23-36. http://dx.doi. org/10.1007/s00105-020-04705-0
6. Woźniak W, Mlosek RK, Ciostek P. Assessment of the efficacy and safety of steam vein sclerosis as compared to classic surgery in lower extremity varicose vein management. Wideochir Inne Tech Maloinwazyjne. 2015;10(1):15-24.
7. Swenil S, Rahul J, Jawahar R, Uday P. RFA vs EVLT: a comparison of treatment options for varicose veins [Internet]. J Med Sci Clin Res. 2017;5:28952-28960. http://dx.doi. org/10.18535/jmscr/v5i10.81
8. Mani BC, Delgado GA. Varicose veins radiofrequency ablation therapy. In: StatPearls [Internet]. StatPearls Publishing; 2020.
9. Malskat WSJ, Poluektova AA, van der Geld CWM, et al. Endovenous laser ablation (EVLA): a review of mechanisms, modeling outcomes, and issues for debate. Lasers Med Sci. 2014;29(2):393-403.
10. Uhl JF, Zimmet SE. Endovenous laser ablation. Phlebolymphology. 2009. Accessed May 9, 2021. https://www. www.phlebolymphology.org/endovenous-laserablation/
11. Garcia-Madrid C, Pastor Manrique JO, Gomez-Blasco F, Sala Planell E. Update on endovenous radio-frequency closure ablation of varicose veins. Ann Vasc Surg. 2012;26(2):281-291.
12. Nandhra S, Wallace T, El-Sheikha J, Carradice D, Chetter I. A randomised controlled trial of perivenous tumescent anaesthesia in addition to general anaesthesia for surgical ligation and stripping of the great saphenous vein. Phlebology. 2020;35(5):305-315.
13. Pannier F, Rabe E, Maurins U. 1470 nm diode laser for endovenous ablation (EVLA) of incompetent saphenous veins – a prospective randomized pilot study comparing warm and cold tumescence anaesthesia. Vasa. 2010;39(3):249-255.
14. Dumantepe M, Uyar I. Comparing cold and warm tumescent anesthesia for pain perception during and after the endovenous laser ablation procedure with 1470 nm diode laser. Phlebology. 2015;30(1):45-51.
15. Gunes T, Altin F, Kutas B, et al. Less painful tumescent solution for patients undergoing endovenous laser ablation of the saphenous vein. Ann Vasc Surg. 2015;29(6):1123-1127.
16. Desmyttere J, Grard C, Mordon S. A 2 years follow-up study of endovenous 980nm laser treatment of the great saphenous vein: role of the blood content in the GSV [Internet]. Med Laser Application. 2005;20:283-289. http:// dx.doi.org/10.1016/j.mla.2005.08.003
17. Vuylsteke ME, Martinelli T, Van Dorpe J, Roelens J, Mordon S, Fourneau I. Endovenous laser ablation: the role of intraluminal blood. Eur J Vasc Endovasc Surg. 2011;42(1):120-126.
18. Varetto G, Guiot C, Destro M, et al. Endovenous laser ablation for varicose veins: towards a personalized energy dose. J Vasc Diagnostic. 2014;2:85-90.
19. Ye K, Wang R, Qin J, et al. Postoperative benefit of compression therapy after endovenous laser ablation for uncomplicated varicose veins: a randomised clinical trial. Eur J Vasc Endovasc Surg. 2016;52(6):847-853.
20. Elderman JH, Krasznai AG, Voogd AC, Hulsewe KWE, Sikkink CJJM. Role of compression stockings after endovenous laser therapy for primary varicosis. J Vasc Surg Venous Lymphat Disord. 2014;2(3):289-296.
21. Bakker NA, Schieven LW, Bruins RMG, van den Berg M, Hissink RJ. Compression stockings after endovenous laser ablation of the great saphenous vein: a prospective randomized controlled trial. Eur J Vasc Endovasc Surg. 2013;46(5):588-592.
22. Lugli M, Cogo A, Guerzoni S, Petti A, Maleti O. Effects of eccentric compression by a crossed-tape technique after endovenous laser ablation of the great saphenous vein: a randomized study. Phlebology. 2009;24(4):151-156.
23. Kabnick LS. Outcome of different endovenous laser wavelengths for great saphenous vein ablation. J Vasc Surg. 2006;43(1):88-93.
24. Disselhoff BCVM, der Kinderen DJ, Kelder JC, Moll FL. Randomized clinical trial comparing endovenous laser with cryostripping for great saphenous varicose veins. Br J Surg. 2008;95(10):1232-1238.
25. Disselhoff BCVM, der Kinderen DJ, Kelder JC, Moll FL. Five-year results of a randomised clinical trial of endovenous laser ablation of the great saphenous vein with and without ligation of the saphenofemoral junction. Eur J Vasc Endovasc Surg. 2011;41(5):685-690.
26. Theivacumar NS, Dellagrammaticas D, Mavor AID, Gough MJ. Endovenous laser ablation: does standard aboveknee great saphenous vein ablation provide optimum results in patients with both above- and below-knee reflux? A randomized controlled trial. J Vasc Surg. 2008;48(1):173-178.
27. Hogue RS, Schul MW, Dando CF, Erdman BE. The effect of nitroglycerin ointment on great saphenous vein targeted venous access site diameter with endovenous laser treatment. Phlebology. 2008;23(5):222- 226.
28. Doganci S, Demirkilic U. Comparison of 980 nm laser and bare-tip fibre with 1470 nm laser and radial fibre in the treatment of great saphenous vein varicosities: a prospective randomised clinical trial [Internet]. Eur J Vasc Endovasc Surg. 2010;40:254-259. http://dx.doi. org/10.1016/j.ejvs.2010.04.006
29. Vuylsteke M, De Bo TH, Dompe G, Di Crisci D, Abbad C, Mordon S. Endovenous laser treatment: is there a clinical difference between using a 1500 nm and a 980 nm diode laser? A multicenter randomised clinical trial. Int Angiol. 2011;30(4):327- 334.
30. Vuylsteke ME, Thomis S, Mahieu P, Mordon S, Fourneau I. Endovenous laser ablation of the great saphenous vein using a bare fibre versus a tulip fibre: a randomised clinical trial. Eur J Vasc Endovasc Surg. 2012;44(6):587-592.
31. Bogachev VI, Boldin BV, Turkin PI. Perioperative administration of micronized purified flavonoid fraction in endovascular treatment of varicose disease. Article in Russian. Angiol Sosud Khir. 2019;25(2):88- 95.
32. Stoiko YM, Mazaishvili KV, Khlevtova TV, Tsyplyashchuk AV, Kharitonova SE, Akimov SS. Effect of pharmacotherapy on course of postoperative period after endovenous thermal ablation. Article in Russian. Angiol Sosud Khir. 2015;21(3):77-81.
33. Ayo D, Blumberg SN, Rockman CR, et al. Compression versus no compression after endovenous ablation of the great saphenous vein: a randomized controlled trial. Ann Vasc Surg. 2017;38:72-77.
34. Nandhra S, Wallace T, El-Sheikha J, Leung C, Carradice D, Chetter I. A randomised clinical trial of buffered tumescent local anaesthesia during endothermal ablation for superficial venous incompetence. Eur J Vasc Endovasc Surg. 2018;56(5):699-708.
35. El-Sheikha J, Nandhra S, Carradice D, et al. Clinical outcomes and quality of life 5 years after a randomized trial of concomitant or sequential phlebectomy following endovenous laser ablation for varicose veins. Br J Surg. 2014;101(9):1093-1097.
36. Carradice D, Mekako AI, Hatfield J, Chetter IC. Randomized clinical trial of concomitant or sequential phlebectomy after endovenous laser therapy for varicose veins. Br J Surg. 2009;96(4):369-375.
37. Samuel N, Wallace T, Carradice D, Mazari FAK, Chetter IC. Comparison of 12-w versus 14-w endovenous laser ablation in the treatment of great saphenous varicose veins: 5-year outcomes from a randomized controlled trial. Vasc Endovascular Surg. 2013;47(5):346-352.
38. Flessenkamper I, Hartmann M, Stenger D, Roll S. Endovenous laser ablation with and without high ligation compared with high ligation and stripping in the treatment of great saphenous varicose veins: initial results of a multicentre randomized controlled trial. Phlebology. 2013;28(1):16- 23.
39. Flessenkamper I, Hartmann M, Hartmann K, Stenger D, Roll S. Endovenous laser ablation with and without high ligation compared to high ligation and stripping for treatment of great saphenous varicose veins: results of a multicentre randomised controlled trial with up to 6 years follow-up. Phlebology. 2016;31(1):23-33.
40. Malskat WSJ, Giang J, De Maeseneer MGR, Nijsten TEC, van den Bos RR. Randomized clinical trial of 940- versus 1470-nm endovenous laser ablation for great saphenous vein incompetence. Br J Surg. 2016;103(3):192-198.
41. Hirokawa M, Ogawa T, Sugawara H, Shokoku S, Sato S. Comparison of 1470 nm laser and radial 2 ring fiber with 980 nm laser and bare-tip fiber in endovenous laser ablation of saphenous varicose veins: a multicenter, prospective, randomized, non-blind study. Ann Vasc Dis. 2015;8(4):282-289.
42. Mendes-Pinto D, Bastianetto P, Cavalcanti Braga Lyra L, Kikuchi R, Kabnick L. Endovenous laser ablation of the great saphenous vein comparing 1920-nm and 1470-nm diode laser. Int Angiol. 2016;35(6):599-604.
43. Theivacumar NS, Dellagrammaticas D, Darwood RJ, Mavor AID, Gough MJ. Fate of the great saphenous vein following endovenous laser ablation: does recanalisation mean recurrence? Eur J Vasc Endovasc Surg. 2008;36(2):211-215.
44. Bergan JJ, Kumins NH, Owens EL, Sparks SR. Surgical and endovascular treatment of lower extremity venous insufficiency. J Vasc Interv Radiol. 2002;13(6):563-568.
45. Lane TRA, Kelleher D, Shepherd AC, Franklin IJ, Davies AH. Ambulatory varicosity avulsion later or synchronized (AVULS): a randomized clinical trial. Ann Surg. 2015;261(4):654-661.
46. Karmacharya RM, Shrestha BK, Shrestha B, et al. Varicose vein invasive intervention at university hospital of Nepal, our experience in the last six years [Internet]. Open Access Surg. 2019;12:21-25. http:// dx.doi.org/10.2147/oas.s214962
47. Abd El-Mabood E-S, El-Gohary H, Salem A. Radiofrequency ablation (RFA) for primary varicose veins: a feasible day-case procedure with good surgical and functional outcomes. Egypt J Surg. 2017;36(4):407.
48. Onwudike M, Abbas K, Thompson P, McElvenny DM. Editor’s Choice – Role of compression after radiofrequency ablation of varicose veins: a randomised controlled trial. Eur J Vasc Endovasc Surg. 2020;60(1):108-117.
49. Pihlaja T, Romsi P, Ohtonen P, Jounila J, Pokela M. Post-procedural compression vs. no compression after radiofrequency ablation and concomitant foam sclerotherapy of varicose veins: a randomised controlled non-inferiority trial. Eur J Vasc Endovasc Surg. 2020;59(1):73- 80.
50. Krasznai AG, Sigterman TA, Troquay S, et al. A randomised controlled trial comparing compression therapy after radiofrequency ablation for primary great saphenous vein incompetence. Phlebology. 2016;31(2):118-124.
51. Gohel MS, Davies AH. Radiofrequency ablation for uncomplicated varicose veins [Internet]. Phlebology 2009;24:42- 49. http://dx.doi.org/10.1258/ phleb.2009.09s005
52. Medical Advisory Secretariat. Endovascular radiofrequency ablation for varicose veins: an evidence-based analysis. Ont Health Technol Assess Ser. 2011;11(1):1-93.
53. Hamann SAS, Timmer-de Mik L, Fritschy WM, Kuiters GRR, Nijsten TEC, van den Bos RR. Randomized clinical trial of endovenous laser ablation versus direct and indirect radiofrequency ablation for the treatment of great saphenous varicose veins. Br J Surg. 2019;106(8):998-1004.
54. Bitargil M, Kılıc HE. Ablation of the great saphenous vein with F-care versus Closurefast endovenous radiofrequency therapy: double-blinded prospective study. Phlebology. 2020;35(8):561-565.
55. Nyamekye IK, Dattani N, Hayes W, Harding D, Holloway S, Newman J. A randomised controlled trial comparing three different radiofrequency technologies: short-term results of the 3-RF trial. Eur J Vasc Endovasc Surg. 2019;58(3):401-408.
56. Almeida JI, Kaufman J, Gockeritz O, et al. Radiofrequency Endovenous ClosureFAST versus Laser Ablation for the Treatment of Great Saphenous Reflux: a multicenter, single-blinded, randomized study (RECOVERY Study) [Internet]. J Vasc Interv Radiol. 2009;20:752-759. http://dx.doi. org/10.1016/j.jvir.2009.03.008
57. Shepherd AC, Gohel MS, Brown LC, Metcalfe MJ, Hamish M, Davies AH. Randomized clinical trial of VNUS ClosureFAST radiofrequency ablation versus laser for varicose veins. Br J Surg. 2010;97(6):810-818.
58. Gale SS, Lee JN, Walsh ME, Wojnarowski DL, Comerota AJ. A randomized, controlled trial of endovenous thermal ablation using the 810-nm wavelength laser and the ClosurePLUS radiofrequency ablation methods for superficial venous insufficiency of the great saphenous vein. J Vasc Surg. 2010;52(3):645-650.
59. Goode SD, Chowdhury A, Crockett M, et al. Laser and radiofrequency ablation study (LARA study): a randomised study comparing radiofrequency ablation and endovenous laser ablation (810 nm). Eur J Vasc Endovasc Surg. 2010;40(2):246-253.
60. Nordon IM, Hinchliffe RJ, Brar R, et al. A prospective double-blind randomized controlled trial of radiofrequency versus laser treatment of the great saphenous vein in patients with varicose veins. Ann Surg. 2011;254(6):876-881.
61. Shepherd AC, Ortega-Ortega M, Gohel MS, Epstein D, Brown LC, Davies AH. Costeffectiveness of radiofrequency ablation versus laser for varicose veins. Int J Technol Assess Health Care. 2015;31(5):289-296.
62. Bozoglan O, Mese B, Eroglu E, et al. Comparison of endovenous laser and radiofrequency ablation in treating varicose veins in the same patient. Vasc Endovascular Surg. 2016;50(1):47-51.
63. Sydnor M, Mavropoulos J, Slobodnik N, Wolfe L, Strife B, Komorowski D. A randomized prospective long-term (>1 year) clinical trial comparing the efficacy and safety of radiofrequency ablation to 980 nm laser ablation of the great saphenous vein. Phlebology. 2017;32(6):415-424.
64. Vuylsteke ME, Mordon SR. Endovenous laser ablation: a review of mechanisms of action. Ann Vasc Surg. 2012;26(3):424- 433.
65. Lin JC, Nerenz DR, Migliore P, Young R, Shepard AD, Weaver WD. Cost analysis of endovenous catheter ablation versus surgical stripping for treatment of superficial venous insufficiency and varicose vein disease. J Vasc Surg Venous Lymphat Disord. 2014;2(1):98-103.
66. Epstein D, Onida S, Bootun R, Ortega- Ortega M, Davies AH. Cost-effectiveness of current and emerging treatments of varicose veins. Value Health. 2018;21(8):911-920.
67. Selvaraj A, Stephen E, Kota A, et al. Outcome of re-using radiofrequency ablation catheter for varicose veins treatment. Indian J Vasc Endovasc Surg. 2020;7(2):154.
68. Schmedt CG, Sroka R, Steckmeier S, et al. Investigation on radiofrequency and laser (980 nm) effects after endoluminal treatment of saphenous vein insufficiency in an ex-vivo model. Eur J Vasc Endovasc Surg. 2006;32(3):318-325.
69. Weiss RA. Comparison of endovenous radiofrequency versus 810 nm diode laser occlusion of large veins in an animal model. Dermatol Surg. 2002;28(1):56-61.
70. Bozoglan O, Mese B, Eroglu E, Ekerbicer HC, Yasim A. Comparison of endovenous laser and radiofrequency ablation in treating varices in the same patient. J Lasers Med Sci. 2017;8(1):13-16.
71. Puggioni A, Kalra M, Carmo M, Mozes G, Gloviczki P. Endovenous laser therapy and radiofrequency ablation of the great saphenous vein: analysis of early efficacy and complications. J Vasc Surg. 2005;42(3):488-493.
72. He G, Zheng C, Yu MA, Zhang H. Comparison of ultrasound-guided endovenous laser ablation and radiofrequency for the varicose veins treatment: an updated meta-analysis. Int J Surg. 2017;39:267-275.
73. Yumun HNA, Gur O, Gurkan S. Comparison of 1470 nm radial fiber laser ablation and radiofrequency ablation in endovascular treatment of venous insufficiency [Internet]. World J Cardiovasc Surg. 2016;06:117-124. http://dx.doi. org/10.4236/wjcs.2016.69019
74. Park I, Park SC. Comparison of short-term outcomes between endovenous 1,940-nm laser ablation and radiofrequency ablation for incompetent saphenous veins. Front Surg. 2020;7:620034.
75. Siribumrungwong B, Noorit P, Wilasrusmee C, Attia J, Thakkinstian A. A systematic review and meta-analysis of randomised controlled trials comparing endovenous ablation and surgical intervention in patients with varicose vein. Eur J Vasc Endovasc Surg. 2012;44(2):214-223.
76. Goode SD, Chowdhury A, Crockett M, et al. Laser and Radiofrequency Ablation Study (LARA study): a randomised study comparing radiofrequency ablation and endovenous laser ablation (810nm) [Internet]. J Vasc Surg. 2010;52:522. http:// dx.doi.org/10.1016/j.jvs.2010.06.097
77. Shepherd AC, Gohel MS, Lim CS, Hamish M, Davies AH. Pain following 980-nm endovenous laser ablation and segmental radiofrequency ablation for varicose veins: a prospective observational study. Vasc Endovascular Surg. 2010;44(3):212-216.
78. Luebke T, Brunkwall J. Systematic review and meta-analysis of endovenous radiofrequency obliteration, endovenous laser therapy, and foam sclerotherapy for primary varicosis. J Cardiovasc Surg. 2008;49(2):213-233.
79. Murad MH, Coto-Yglesias F, Zumaeta- Garcia M, et al. A systematic review and meta-analysis of the treatments of varicose veins. J Vasc Surg. 2011;53(5 Suppl):49S- 65S.
80. van den Bos R, Arends L, Kockaert M, Neumann M, Nijsten T. Endovenous therapies of lower extremity varicosities: a meta-analysis. J Vasc Surg. 2009;49(1):230-239.
81. Kheirelseid EAH, Crowe G, Sehgal R, et al. Systematic review and meta-analysis of randomized controlled trials evaluating longterm outcomes of endovenous management of lower extremity varicose veins. J Vasc Surg Venous Lymphat Disord. 2018;6(2):256-270.
82. Paravastu SCV, Dodd PDF. Endovenous ablation therapy (LASER or radiofrequency) or foam sclerotherapy versus conventional surgical repair for short saphenous varicose veins [Internet]. Cochrane Database Syst Rev. 2013. http://dx.doi. org/10.1002/14651858.cd010878
83. Gloviczki P, Comerota AJ, Dalsing MC, et al. The care of patients with varicose veins and associated chronic venous diseases: clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum [Internet]. J Vasc Surg. 2022;53:2S-48S. http://dx.doi. org/10.1016/j.jvs.2011.01.079
