I. Union Internationale de Phlébologie Presidential Address, Awards, and Consensus Documents
I. Union Internationale de
Phlébologie Presidential Address,
Awards, and Consensus Documents
Presidential address
Angelo Scuderi, Brazil
The Union Internationale de Phlébologie is the largest international organization devoted to the investigation and management of venous disorders and they have contributed many consensus documents to provide guidelines for vascular specialists and others worldwide on the management of patients with various venous problems. The
In 2015, one document about venous ulcers was prepared and published in International Angiology (Mosti et al. Int Angiol. 2015;34(3):202-218). The working group produced comments and suggestions for updating the recent guidelines on the management of venous leg ulcers by the Society for Vascular Surgery and the American Venous Forum (SVS–AVF). The SVS–AVF guidelines include 75 recommendations. The Union Internationale de Phlébologie experts have changed the grade of recommendation in 6 cases, summarized 4 recommendations into 1, added 3 new recommendations, and even reversed 3 others. For example, the Union Internationale de Phlébologie working group was against routine laboratory evaluation for thrombophilia for patients with chronic recurrent venous leg ulcers, while the recommendation of American experts suggested such testing if patients had a history of recurrent venous thromboembolism. The most important conclusion from the consensus is that only 60% of the guidelines do not contain any recommendations, just suggestions that are supported by very weak evidence. Grade 1A was allocated to only 1 recommendation regarding compression over no compression when treating venous leg ulcers. This highlights existing problems when preparing modern guidelines because many aspects of venous disease are still poorly investigated or even unknown.
Other Union Internationale de Phlébologie consensus documents are now being prepared on hemodynamic concepts, pelvic varicose veins, rehabilitation, and foam sclerotherapy, which are challenging topics that have never been discussed in any guidelines.
Servier award 2013-2015
Chronic venous disease of the lower limbs in a Sub-Saharan African setting
Marcus Fokou, Cameroon
For the first time, the pattern of chronic venous disease in a Sub-Saharan African setting was investigated. Specifically, the study was designed to determine the characteristics of patients suffering from chronic venous disease, describe the extent of chronic venous disease according to the clinical, etiological, anatomical, pathophysiological (CEAP) classification, and assess both the venous clinical severity score and venous disability score.
During a 12-month period, a cross-sectional study was conducted on all patients with evidence of chronic venous disease, who were >18 years old and attending the outpatient clinic of the Yaoundé General Hospital in Cameroon. The method of examination was adapted from the method used in the San Diego population study1 and the full CEAP classification was used.2 A structured interview recorded information on demographics, relevant medical history, with a special consideration for information suggesting the etiology of the venous disease (primary, secondary, congenital), family history, symptoms potentially related to venous disease (aching, itching, heaviness, nighttime cramping, restless and tired legs), and lifestyle. A comprehensive standardized examination was conducted by one of the two vascular surgeons to determine the magnitude of visible disease according to the CEAP classification. A duplex ultrasound, performed by the radiologist following the standardized protocol, investigated the functional disease at various anatomical sites (superficial, deep, and perforator veins) and the pathophysiology (normal, reflux, and obstruction) to define the CEAP classification. The venous disability score and the revised venous clinical severity score were used to grade the severity of the chronic venous disease.
The study started in November 2013 and ended in July 2015. A total of 210 patients (238 affected legs) with chronic venous disease and 100 healthy controls were enrolled. Chronic venous disease patients were mostly men (54.3%) and the age ranged from 18 to 85 years with a mean of 44.5 years. Risk factors, such as obesity (body mass index >30), were found in 33% of patients and a family history of chronic venous disease in 18% of patients (53% from the maternal side, 42% from the paternal side, and 5% for both parents). Most of the patients (66%) had a lifestyle that required long periods of standing (>8 hours/day). Only 8% were tobacco consumers and all smokers were men. For women, 68% had not gone through menopause. Among the women, only 15% were taking birth control pills and the parity ranged from 1 to 13 with a mean of 3.7 deliveries per woman. None of the postmenopausal women were using hormone replacement therapy. Out of the 43% of the chronic venous disease patients, 34% had been previously treated with venoactive drugs, 16% with compression hosiery, 2% with surgery, and only 1 patient had been treated with sclerosants.
Affected legs with chronic venous disease were symptomatic in 73% of the cases and had the following symptoms: leg heaviness (47%), sensation of swelling (47%), leg pain (39%), sensation of “pins and needles” in the legs (22%), nighttime cramps (18%), and itching (13%). The severity of the disease using the revised venous clinical severity score3 ranged from 1 to 21 with a mean of 4.62. Regarding the CEAP classification, chronic venous disease patients were assigned in the following classes:
•C: Clinical presentation: C0s (6.1%), C1 (345.4%), C2 (39.6%), C3 (42.7%), C4a (11.9%), C4b (4.9%), C5 (1.5%), C6 (10.1%).
•E: Etiology: primary (88.7%), secondary (9.8%), congenital (1.5%; 3 cases had Klippel-Trenaunay syndrome).
•A: Anatomical location: superficial (71%), deep (43.3%), perforators (4.3%), no location identified (6.1%).
•P: Physiopathology: reflux (62%), obstruction (9.2%), both (4.6%), none (24.3%).
Quality of life was assessed in the majority of patients. Cross results and comparisons of all variables between chronic venous disease and healthy patients will bring new views on the epidemiology of chronic venous disease, in general, and of an African presentation, in particular. This is the first time that such a survey was performed in Africa. The comparison between the results found in the present survey with those of the main population-based surveys performed in the Western World remains to be done and should bring additional information.
References
1. Criqui MH, Jamosmos M, Fronek A, et al. Chronic venous disease in an ethnically diverse population: the San Diego population study. Am J Epidemiol. 2003;158:448-456.
2. Eklöf B, Rutherford RB, Bergan JJ, et al; American Venous Forum International Ad Hoc Committee for Revision of the CEAP Classification. Revision of the CEAP classification for chronic venous disorders: consensus statement. J Vasc Surg. 2004;40:1248-1252.
3. Vasquez MA, Rabe E, McLafferty RB, et al; American Venous Forum Ad Hoc Outcomes Working Group. Revision of the venous clinical severity score: venous outcomes consensus statement. J Vasc Surg. 2010;52(5):1387-1396.
Metabonomic profiling for the identification of novel biomarkers in deep vein thrombosis
Joseph Shaloub, UK
The purpose of the study is to verify the hypothesis that biofluid (blood and urine) metabolite profiles of patients with deep vein thrombosis are significantly different from both the biofluid metabolite profiles of patients with similar symptoms, but no deep vein thrombosis, and the metabolite profiles of healthy volunteers. The methodology consists of identifying new biological biomarkers of deep vein thrombosis using a nontargeted metabonomic analysis. The identification of a new diagnostic biomarker or biomarker signature that can be measured easily in biofluids, with a relatively low cost and a high sensitivity and specificity for deep vein thrombosis would contribute to the improved management of patients with deep vein thrombosis.
The study is an observational case-control study, including 200 patients and 40 healthy subjects. A total of 200 patients presenting with a suspicion of deep vein thrombosis will be recruited. These patients will be divided into three groups: (i) patients with deep vein thrombosis confirmed by duplex ultrasound; (ii) patients with similar symptoms, but where deep vein thrombosis has been excluded by duplex ultrasound; and (iii) 40 healthy volunteers. According to the recommendations of the National Institute for Health and Care Excellence, patients presenting to the emergency department or ambulatory care units with a high suspicion of deep vein thrombosis should undergo venous duplex imaging to confirm the diagnosis. If the duplex scan cannot be carried out within 4 hours, an interim 24-hour dose of a parenteral anticoagulant will be given and the duplex scan will be performed within 24 hours.
Metabolic profiling is sensitive to environmental and external factors; therefore, blood and urine sampling will be repeated before and after parenteral anticoagulation is administered. The subjects enrolled in the study will have their full medical history recorded, including medication details, examination of the lower limbs, and blood and urine sampling data. An additional blood sample will be stored for future DNA analysis to compare with the findings of the metabolite profile. The patients in group 1 will repeat the duplex ultrasound 3 weeks after the end of their treatment (treatment usually lasting 3 to 6 months) and a further blood and urine sample will be collected for metabonomic analysis.
Detection and quantification of metabolites in human blood serum and urine will be completed using state of the art untargeted mass spectrometry and nuclear magnetic resonance metabolic profiling approaches. The mass spectrometry and nuclear magnetic resonance spectra from the samples will be analyzed in order to identify metabolite features whose quantities are significantly different between the three groups. These metabolites will be classified and identified. Metabolite identification will be performed by consulting with in-house and online metabolite databases. The primary outcome is to identify metabolites that are sensitive and specific for deep vein thrombosis. Secondary outcomes will include: (i) correlating the results with the extension and chronicity of the thrombus; and (ii) investigating the effect of parenteral anticoagulation on the metabonomic profile.
Detergent sclerosants activate endothelial cells at low concentration in vitro
David Connor, Australia
Sodium tetradecyl sulphate and polidocanol are two detergent sclerosants that are routinely injected during sclerotherapy for the treatment of varicose veins and venous malformations. The ultimate aim of such injections is to induce endothelial cell lysis and eventual closure of the vessel. It is acknowledged that detergent sclerosants induce endothelial cell lysis at high concentrations (>0.3%), but the effect of sublytic concentrations is unknown. The current project is testing the hypothesis that in vitro incubation of endothelial cells with low concentrations of detergent sclerosants will result in cellular activation and an increase in both the surface expression of activation markers and release of endothelial microparticles.
Cultures of human umbilical vein endothelial cells were incubated with sodium tetradecyl sulphate and polidocanol at different concentrations for 15 minutes. Detergent sclerosants release endothelial CD31+/Lactadherin+ microparticles and proinflammatory cytokines, such as activation markers (ICAM-1 and E-Selectin) and constitutive markers (PECAM-1, endoglin, VE-Cadherin, MCAM-1).
Previous work has shown that in vitro incubation of cultured endothelial cells with low concentrations of detergent sclerosants stimulates the activation of platelets and the release of procoagulant platelet-derived microparticles (Figure 1).1,2 When low concentrations of detergent sclerosants (0.075% sodium tetradecyl sulphate and polidocanol) were incubated with endothelial cells, microparticle release increased, but then started to gradually decrease as the sclerosant concentrations increased. The next stage will be to test for platelet activation, leukocyte adhesion, and endothelial cytokine release with low concentrations of sodium tetradecyl sulphate and polidocanol.

Figure 1. Flow cytometric analysis of platelet activation and release of procoagulant platelet-derived microparticles from cultured
endothelial cells incubated with various concentrations of detergent sclerosants (sodium tetradecyl sulphate and polidocanol).
References
1. Parsi K, Exner T, Connor DE, Ma DD, Joseph JE. In vitro effects of detergent sclerosants on coagulation, platelets and microparticles. Eur J Vasc Endovasc Surg. 2007;34:731-740.
2. Parsi K, Exner T, Connor DE, Herbert A, Ma DD, Joseph JE. The lytic effects of detergent sclerosants on erythrocytes, platelets, endothelial cells and microparticles are attenuated by albumin and other plasma components in vitro. Eur J Vasc Endovasc Surg. 2008;36:216-223.
Effect of compression therapy in patients receiving endovenous treatment for varicose veins using foam
sclerotherapy
Roshan Bootun, UK
The 2015 winning project will look at the effect of compression therapy in patients receiving endovenous treatment for varicose veins using ultrasound-guided foam sclerotherapy. As uncertainty remains about the use of compression stockings following treatment of varicose veins, the 2013 National Institute for Health and Care Excellence guidelines on varicose veins recommends further research to evaluate both the clinical effectiveness and cost-effectiveness of this postprocedural intervention.1 At the same time, the Union Internationale de Phlébologie recommended using compression for certain indications, including postoperative treatment of varicose veins.2
Hamel-Desnos et al previously conducted a randomized controlled trial studying the effect of compression in patients undergoing ultrasound-guided foam sclerotherapy of the saphenous veins.3 They reported that patients with compression had similar pain and quality of life scores than patients without compression; however, only 60 patients were recruited in the trial; therefore, it could be hypothesized that the population was not large enough to demonstrate a difference.
Based on power calculations, the sample size has been estimated at 350 patients. The project will examine the effect of compression therapy after ultrasound-guided foam sclerotherapy. In this trial, patients will be randomized to either group with compression (group A) or a group without compression (group B). Adults with varicose veins suitable for ultrasound-guided foam sclerotherapy will be included in the study. Patients will be excluded from the trial if they present with current deep vein thrombosis or peripheral arterial disease.
The primary objective of the study will be patient’s pain score for the first 10 days postprocedure, which will be determined using a validated visual analogue scale. Secondary objectives will be to compare the two treatment groups with respect to quality of life scores, clinical scores, degree of phlebitis, time to return to normal activities, and occlusion rate at 6 months. Recruitment will require 12 months and the follow-up will last 6 months.
The results will be presented at the 2017 Union Internationale de Phlébologie meeting in Melbourne, Australia
References
1. National Institute for Health and Care Excellence (NICE) guidelines [CG168]. Varicose veins in the legs: the diagnosis and management of varicose veins. https://www.nice.org.uk/guidance/cg168. Published July 2013. Accessed September 9, 2015.
2. Partsch H, Flour M, Smith PC; International Compression Club. Indications for compression therapy in venous and lymphatic diseases: consensus based on experimental data and scientific evidence. Under the auspices of the IUP. Int Angiol. 2008;27(3):193-219.
3. Hamel-Desnos CM, Guias BJ, Desnos PR, Mesgard A. Foam sclerotherapy of the saphenous veins: randomised controlled trial with or without compression. Eur J Vasc Endovasc Surg. 2010;39(4):500-507
Outflow performance of different stockings in the treatment of lymphedema and postthrombotic syndrome using air plethysmography
Christopher Lattimer, UK
Manufacturers extensively test compression stockings to quantify compression strength, pressure graduation, surface contour, and knit. Despite this testing, compression stockings are not tolerated by some people and they could even cause harm. Furthermore, compliance is a major issue. These factors may be related to how stockings augment the venous return. This study compared the in vivo performance of elastic compression stockings in healthy controls with patients with varicose veins, postthrombotic syndrome, and lymphedema.
Stocking ejection force was tested by measuring the reduction in calf volume of a congested calf after sudden deflation of a thigh-cuff (outflow fraction). The ability of a stocking to resist increases in calf volume after incremental thigh-cuff inflations was tested by measuring the incremental thigh-cuff pressure causing the maximal increase in calf volume (IPMIV). Venous filling index was assessed when the patients stood up in order to verify the presence of reflux (high venous filling index, >2.5 mL/s). Venous drainage index was measured after leg elevation (low venous drainage index, <10 mL/s). A slow decrease in calf volume after elevation implies venous obstruction.
A total of 12 legs were tested in each group using no compression, knee-length class 1 (18 to 21 mm Hg) compression, and then class 2 (23 to 32 mm Hg) compression.
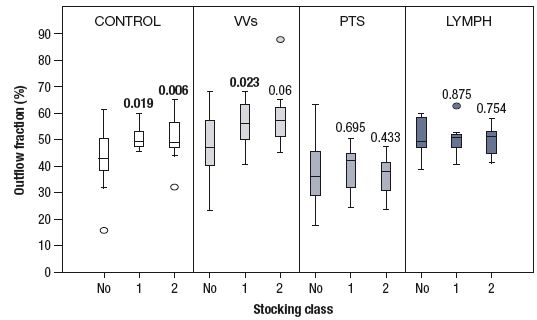
Figure 1. Stocking ejection force is tested by measuring the reduction in calf volume of a
congested calf after sudden deflation of a thigh cuff (outflow fraction).

Figure 2. The performance of a stocking to resist increases in calf volume after incremental
thigh-cuff inflations was assessed using the incremental thigh cuff pressure causing the maximal
increase in calf volume (IPMIV).
Stocking interface pressures (mm Hg) were measured in the supine position at 2 points using the PicoPress_. The values of the outflow fraction, IPMIV, venous filling index, and venous drainage index were quantified in each of the four groups. In particular, stockings significantly improved the outflow fraction and IPMIV both in controls and patients with varicose veins (Figures 1 and 2). The venous filling index improved significantly in patients with varicose veins. There was a 6-fold improvement in the venous drainage index in the only postthrombotic syndrome patient with an iliac occlusion from 2.3 (none) to 14.3 and 13.3 with class 1 and 2 stockings, respectively.
In conclusion, stocking performance tests measuring acute volume changes in vivo in response to provocation maneuvers may explain why the legs of some patients improve with stockings and why other legs may not benefit to the same extent.
Elastic compression elicited beneficial cardiovascular effects: a complex clinical study in healthy,
lymphedematous, and lipedematous individuals
Győző Szolnoky, Hungary
Research on compression therapy is mostly focused on venous and lymph flow; however, the effects of medical compression stockings on cardiovascular responses have been poorly studied, which means that the systemic effects of elastic compression still needs further clarification. Medical stockings with mild compression improved pulse wave velocity, which is the gold-standard measurement of aortic elastic properties. Sports stockings are considered efficient at improving running capacity, but their mode of action remains to be elucidated. Nongraduated stockings exert remarkable venous hemodynamic effects, but their systemic cardiovascular effect has never been measured. Recent studies showed high aortic stiffness in the legs ofpatients with secondary lymphedema and lipedema. Sustained compression with elastic material is the cornerstone of controlling limb volume, despite the fact that its cardiovascular impact has been poorly investigated.
This project will test the hypothesis that sports and nongraduated knee stockings for healthy individuals and compression hosiery for patients with lymphedema and lipedema may provide beneficial cardiovascular effects. Patients eligible for the research will undergo blood pressure assessment, two-dimensional echocardiography, and pulse wave velocity measurements to determine aortic elastic properties before and after the use of compression garments.
Hemodynamics of chronic venous disease and clinical significance
Andrew Nicolaides, Cyprus
Venous hemodynamic concepts are useful in understanding the pathophysiology of chronic venous disease, the significance of the results of different investigations, and the hemodynamic changes associated with symptoms and different methods of treatment. Venous hemodynamic changes consist of changes in pressure, volume, velocity, flow, resistance, venous compliance or elasticity, function of the calf muscle pump, and changes in microcirculation. Velocity and flow are the only hemodynamic changes that can be measured using duplex ultrasound scanning. Hemodynamic testing was routine practice in the 1970s and 1980s until duplex ultrasound scanning was invented. Subsequently, routine hemodynamic measurements were abandoned in favor of duplex ultrasound scanning. Since then, it has been repeatedly stated that there is a poor correlation between hemodynamic measurements and the clinical severity of chronic venous disease.
Nicolaides addressed three questions: (i) what is the relationship between hemodynamic measurements (changes in volume, pressure, and flow) and severity of chronic venous disease?; (ii) what is the significance of this relationship?; and (iii) do hemodynamic changes affect our practice? Venous hypertension is the key hemodynamic abnormality that underlies the development of symptoms and signs of chronic venous disease. In the 1990s, it was shown that patients presenting with venous symptoms had prevalent skin changes, increased rates of ulceration, and increased ambulatory venous pressure. If the ambulatory venous pressure is <40 mm Hg, the prevalence of ulceration in patients with symptomatic chronic venous disease is less than 10%; however, if the ambulatory venous pressure is >90 mm Hg, the prevalence increases linearly to almost 100%.
Two protective mechanisms tend to improve the effects of increased ambulatory venous pressure: (i) lymphatic drainage can increase up to 10 times in normal individuals, but only 2 times in some individuals and not at all in patients with lymphedema; and (ii) the high fibrinolytic activity in the blood and extracellular compartment found in some individuals, can effectively remove extravascular fibrin deposits and other proteins. For patients with moderately raised ambulatory venous pressure (35 to 65 mm Hg), measurements of global fibrinolysis (expressed in mg of fibrin lysed per hour), which were made in the late 1980s, showed that, if fibrinolytic activity was low, 90% of patients had skin changes and ulcerations. However, if fibrinolytic activity was normal or high, only 16% of patients had an ulcer. The variable response of the lymphatic and fibrinolytic systems can explain most of the variability in clinical severity found among different patients with the same hemodynamic abnormality.
Reflux, measured as mL/min using the volume flow facility of duplex scanners or as mL/sec using air plethysmography, has the highest correlation with clinical severity. Peak reflux velocity has a moderate correlation and reflux time. In one study using air plethysmography, reflux venous filling index was 0.5 to 0.8 mL/sec in normal controls; 0.7 to 1.8 mL/sec for the clinical, etiological, anatomical, physiological (CEAP) classification C1; 2.8 to 4.5 mL/sec in classes C2 to C3; and 4.0 to 10.1 mL/sec in classes C4 to C6. Axial reflux, ie, reflux extending from the common femoral vein to the calf veins, is associated with high clinical severity, which is even higher when associated with outflow obstruction. However, the presence of competent popliteal valves, even in the presence of outflow obstruction, result in a normal or an almost normal leg, which is asymptomatic, even in the presence of outflow obstruction.
The effect of high saphenous ligation, stripping, and phlebectomies in limbs with varicose veins and normal deep veins (n=1756) at 1 month have been shown to decrease venous volume, venous filling index, and residual venous volume by 25%, 71%, and 30%, respectively, and increase the ejection fraction by 20%. The effect of high saphenous ligation, stripping, and phlebectomies in limbs with varicose veins and reflux in deep veins (n=102) at 3 months have been shown to decrease venous filling index from 8.4}6.3 to 2.7}2.6 mL/sec, increase the ejection fraction from 44% to 54%, and decrease residual venous volume from 48% to 35%. The prevalence of femoral vein reflux decreased from 65% to 32%. These changes were associated with ulcer healing in 97% of patients at 6 months.
In patients with axial reflux in the deep veins (n=140), valvuloplasty decreased venous filling index from 4.1}2.8 mL/sec to 3.1}2.8 mL/sec. In another study, it was shown that patients with a venous filling index >4.0 mL/sec have a 43% and 60% risk of ulcer recurrence at 1 year and 2 years, respectively. These patients benefit from deep venous valve reconstruction. However, patients with deep venous reflux and a venous filling index <4.0 mL/sec do not benefit from valvuloplasty. The measurement of venous filling index (reflux [mL/sec]), outflow resistance (mm Hg/ mL/min), and their combined parameter hemodynamic index has a linear relationship with the venous clinical severity score (r=0.83). These quantitative measurements of venous filling index and outflow resistance indicate whether the main hemodynamic abnormality is reflux, outflow obstruction, or both, and subsequently assist in the development of a rational plan for management. A list of anatomic and hemodynamic factors associated with increased severity of chronic venous disease has been produced and include an increase in the anatomic extent of reflux, reflux involving 2 or more systems (superficial, deep, or perforating veins), reflux >5 mL/sec on air plethysmography, severe obstruction with an outflow resistance >0.03 mm Hg/mL/min, and reflux >4 mL/sec combined with an ejection fraction <40%. This work has five main conclusions: (i) there is a high correlation between the venous clinical severity score and the combined measurements of reflux and resistance; (ii) the statement “there is a poor correlation between hemodynamic measurements and clinical severity of chronic venous disease” should be modified to “there is a poor correlation between duplex scanning measurements and clinical severity of chronic venous disease”; (iii) duplex scanning provides information on the presence and anatomic extent of the reflux or obstruction; (iv) if quantitative information is needed (how much reflux or obstruction is present) for clinical decisions, duplex scanning should be complimented by air plethysmography; and (v) resistance outflow and reflux venous filling index should be measured before and after stenting, so the baseline readings can be correlated with those that derive clinical benefit. This should provide a better selection of patients for stenting.
