II – Main Topics in Phlebology
- Chronic Venous Disease Overview: Epidemiology, Pathophysiology, Diagnosis, and Management
- Drugs in Phlebology
- Venous Reflux
- Recurrent Varicose Veins
- Pelvic Venous Disease
- Endovenous Interventions and Surgery
- Deep Vein Reconstruction
- Vena Cava Filters
- Thromboembolic Diseases
- Antiphospholipid Syndrome
- Interventional Radiology
- New Technologies
- Compression Therapy
- Leg Ulcers
- Vascular Anomalies
- Genetics
- Debates
Chronic Venous Disease Overview: Epidemiology, Pathophysiology, Diagnosis, and Management
Epidemiology of chronic venous disease
Varicose veins and chronic venous insufficiency are very common worldwide. The risk factors differ significantly between varicose veins and chronic venous insufficiency. Progression of reflux, varicose veins, and chronic venous disease is very frequent. A high proportion of uncomplicated varicose veins (C2) develop skin changes and chronic venous insufficiency (C3-C6). Significant risk factors associated with the progression of varicose veins toward venous leg ulcers include skin changes, corona phlebectatica, a higher body mass index, and popliteal vein reflux. During a 13.4-year follow-up period, 57.8% (4.3% per year) of all patients with chronic venous disease showed disease progression.
Phlebogonarthrosis: a clinical and physiopathological reality
Gonarthrosis is a chronic degenerative disease of the knee, characterized by cartilaginous and bone wear lesions, diminishing of the joint space, the coexistence of the osteophytes, bone condensation, and decalcification at the joint epiphysis; however, inflammatory tests are normal. There are several etiologic mechanisms involved, such as organic causes (frequently repeated microtrauma, flat foot, congenital hip luxation), functional disturbances (menopause, neuroendocrine diseases, obesity, old age), and blood flow disturbances (arterial theory, venous theory). Venous insufficiency may have the following effects on the knee joint: inflammatory circumscribed processes at the periosteum (ossifying periostitis, bone degenerative periostitis), osteoporosis, osteophytosis, bone neoformation, and cartilage injury. The simultaneous existence of gonarthrosis and varices on the same inferior limb was reported as follows by different investigators: 18% (San-Sola), 48% (Bourguesdon), 20% (Robecchi). A nonstripping ambulatory surgical treatment of the varicose veins was performed in 19 patients with gonarthrosis and concomitant voluminous varices on the same leg (great saphenous vein). During surgery, dilated insufficient genicular veins were observed in all cases. These veins were intercepted, sectioned, and ligated (the reflux and hyperpressure were eliminated), resulting in an improvement in the joint symptomatology, with the disappearance of joint pain and gonalgia (16 cases [84%]) and a significant reduction in pain (3 cases [16%]). In addition, there was an improvement in the magnetic resonance imaging and conventional radiography signs of gonarthrosis 3 to 6 months after the operation without any other concomitant treatment, and there was no longer a need to use complementary treatments, such as pain killers, anti-inflammatory drugs, and physiotherapy. The importance of the venous factor in a significant number of patients with simultaneous gonarthrosis and varicose veins on the same leg justifies the term phlebogonarthrosis. The pathway from the sufficient great saphenous vein through the joint of the knee is the insufficient genicular vein.
Update on clinical applications of venous hemodynamics
So far, attempts to correlate venous hemodynamic measurements with the symptoms and signs of chronic venous disease have produced poor results, probably due to a lack of methods to quantify obstruction, as well as the three variable protective mechanisms, ie, the ability of lymphatic drainage to increase 5 to 10 times in some individuals, but only 2 times in others (zero in patients with lymphedema), the variable fibrinolytic activity in blood and tissues, and the duration of the venous hypertension (years). Despite the above, quantitative air-plethysmographic measurements, such as venous filling index (VFI) in mL/sec (a measure of reflux), ejection fraction of the calf muscle pump, and outflow resistance in mm Hg/mL/sec can supplement duplex imaging and assign risk more accurately or predict the success or failure of reconstructive procedures. For example, a VFI <5 mL/min is associated with a low prevalence of chronic swelling (12%), skin changes (19%), and ulceration (0%); whereas, a VFI >5 mL/sec is associated with a high prevalence of chronic swelling (46%), skin changes (61%), and ulceration (46%). Thus, a reflux >5 mL/sec is an indication for an intervention to prevent disease progression. In patients with deep venous reflux, successful valvuloplasty decreases the VFI to <5 mL/sec; however, if the VFI is <5 mL/sec, valvuloplasty has no effect on ulcer healing or symptom relief. In addition, venous stenting is not likely to be beneficial with a VFI >5 mL/sec and an outflow resistance <0.2 mm Hg/mL/sec, indicating a well-developed collateral circulation. Such patients can be spared from an unnecessary stent. They are more likely to benefit from valve reconstruction.
Applications of capillaroscopy in phlebology and angiology
Videomicroscopy provides easy access to visualize the skin nutritional capillaries at the nailfold and all over the body surface. Nailfold capillaroscopy is useful for the early diagnosis of systemic sclerosis in patients with an isolated Raynaud phenomenon. It also provides prognostic information. Capillaroscopy generates information on the cutaneous microvascular damage in patients with advanced peripheral arterial disease and chronic venous insufficiency. In patients with chronic venous disease, lower leg mapping using capillaroscopy detects venous cutaneous microangiopathy early. The practical usefulness of this information remains to be further evaluated.
Venous mapping
Venous mapping is important, especially for the clinical efforts to provide evidence based best practices for safe patient outcomes. Venous mapping consists of duplex ultrasound mapping and generation of diagrams for consistent communication of globally comparable results. Mapping could mean mapping to use a vein as a vascular conduit, to assess the venous system in the presence of nonhealing or recurring ulceration, and mapping prevaricose vein interventions. An International Union of Phlebology consensus document on lower limb vein mapping already exists. The objective of a venous duplex exam of the deep veins is to determine the patency of deep vein outflow, normal deep vein lumen appearances, including valves, competent valve function, and anatomy with documentation and communication of findings to guide a management plan. The objective of a venous duplex exam of the superficial veins is to determine patency of vein outflow, obtain evidence of acute or chronic superficial venous thrombosis, normal vein appearances, including valves, competent valve function, and anatomy with documentation and communication of findings to guide a management plan. Many example diagrams were presented; for each diagram, the patient’s ID, the clinical question, and the patient’s position should be indicated. Deep veins are drawn in blue for normal and in red for abnormal; the same applies for superficial veins. Labels are color coded and adjacent to the location. Next, the speaker showed the symbols to use for treated segments (eg, patent and competent, patent and incompetent), perforating veins, tortuosity, occlusion or thrombosis, and residual lumen posttreatment. At the end of the presentation, Morgan showed a chronic venous insufficiency worksheet that she uses in her daily practice.
Venous distension in patients with aneurysmal arterial disease compared with venous distension in patients with arterial occlusive disease and with healthy controls
Elastin degradation in the vascular wall leads to a dilatation in patients with aneurysmal arterial disease and varicose veins. This finding is not restricted to arteries; similar changes can be found in the venous system. This study assessed venous distensibility in patients with aneurysmal arterial disease, in patients with arterial occlusive disease, and in healthy subjects. For patients with an aortic or popliteal aneurysm, the inclusion criteria were an aortic diameter ≥3 cm and popliteal artery diameter ≥1.5 cm, and, for patients with arterial occlusive disease, the inclusion criteria were an ankle brachial index <0.9 and positive criteria in the Edinburgh questionnaire. The control group was an age-matched group of people without arterial occlusive disease (ankle brachial index ≥0.9) or aneurysmal arterial disease. People with diabetes, acute deep venous thrombosis or a history of deep venous thrombosis, impossibility to stand, and <18 years old were excluded. Family and personal history, weight, height, medication, arterial occlusive disease symptoms (Edinburgh claudication questionnaire), pulse palpation, and ankle pressure were assessed. Arterial diameters in the aorta and leg arteries, venous reflux in superficial and deep leg veins, venous distensibility in the common femoral vein, the great saphenous vein, and the femoral vein were evaluated by duplex ultrasonography. In the common femoral vein, great saphenous vein, and femoral vein, venous diameter differences were significantly larger in patients with aneurysmal arterial disease compared with both patients with arterial occlusive disease and healthy subjects.
Drugs in Phlebology
Overview of venoactive drugs
Venoactive drugs are a heterogeneous group of synthetic or plant-based drugs. Several of these drugs can act on many targets that are responsible for the signs and symptoms of chronic venous disease (C0s-C6). The treatments result in an increase in venous tone through a mechanism related to the noradrenaline pathway, an increase in capillary resistances a reduction capillary filtration, an improvement in lymphatic flow, and an increase in the number of lymphatic vessels, an impact on hemorheological disorders, and prevention of inflammation in the vein walls and vein valves. Moreover, it seems they have a specific pain-killing effect. Wang Y et al recently demonstrated that diosmin might reduce radicular pain in much the same way as mannitol plus dexamethasone, the currently used active treatment. These effects might partly be attributed to its anti-inflammatory and analgesic components. The main indications for venoactive drugs are symptoms related to chronic venous disease and edema. They can also be used for the treatment of pelvic congestion syndrome, lymphedema, or venous ulcers and in adjunction with sclerotherapy or venous surgery. Side effects are rare and include skin reactions and digestive problems. Studies of the efficacy of venoactive drugs in treating symptoms and edema related to chronic venous disease are rarely comparable, owing to disparities in inclusion criteria and primary end points. The main guidelines in the field of venous disease recommend using different venoactive drugs according to the principles of the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) system.
Pediatric population: how to adjust the dose
Randomized controlled trials on pediatric anticoagulation are lacking, so physicians rely on evidence-based consensus guidelines. The most comprehensive guidelines published are those of the American College of Chest Physicians (AT9). Unfractionated heparin has some advantages, primarily a short half-life and the ability to be completely reversed with protamine if necessary; however, the difficulties of using unfractionated heparin include the need for venous access, frequent monitoring, and activated partial thromboplastin time (aPTT), as well as monitoring issues in the laboratory. The correlation between aPTT and the effect of heparin as measured by anti–Factor Xa (anti–FXa) (r2=0.51) and protamine titration (r20.55) is relatively weak. aPTT was less predictive of the effect of anti–FXa in children <2 years old. Therefore, it is suggested that both aPTT and anti–FXa assays be used for the monitoring of unfractionated heparin therapy in neonates.
The results of coagulation assays depend on the type of reagent, commercial kits, and analyzers used in the laboratory. Ideally, each laboratory should set up its own pediatric reference ranges for aPTT and anti–FXa assays. Regarding low-molecular weight heparin (LMWH) for neonates, the recommended starting dose is 1.5 mg/kg, but a recent study suggested a higher starting dose of 1.7 mg/kg every 12 hours for term neonates and 2.0 mg/kg every 12 hours for preterm neonates in the absence of a considerable bleeding risk. Another retrospective chart review evaluating enoxaparindosing requirements in infants and children showed that a higher starting dose of enoxaparin (1.7 mg/kg) compared with the starting standard dose (1.5 mg/kg) may result in a faster attainment of therapeutic anti–FXa levels, with significantly fewer venipunctures and dose adjustments and no increase in adverse outcomes. This study suggested that younger children required a higher weight-based dose of enoxaparin (<3 months: 1.83 mg/kg [SD=0.31]; 3 to 12 months: 1.48 mg/kg [SD=0.36]; 1 to 5 years: 1.23 mg/kg [SD=0.21]; and 6 to 18 years: 1.13 mg/kg [SD=0.16]) to reach therapeutic anti–FXa levels.
The guidelines suggest, that, for neonates and children receiving either once- or twicedaily therapeutic LMWH, the drug be monitored to a target anti–FXa activity range of 0.5 to 1.0 units/mL in a sample taken 4 to 6 hours after a subcutaneous injection or 0.5 to 0.8 units/mL in a sample taken 2 to 6 hours after a subcutaneous injection. Vitamin K antagonists may be more practical for older children, but the optimal intensity of therapy in the management of childhood venous thromboembolism has not been fully elucidated. The target international normalized ratio of 2.5 (range, 2-3) is still based on adult data and is generally accepted as appropriate for the pediatric population with a venous thromboembolism. Warfarin international normalized ratio monitoring can be performed in an outpatient or home setting with formal training on the system for whole blood capillary monitoring, thus negating the need for repeated venous access.
Diosmin: when to use it and when it is useful
Diosmin is a flavonoid compound with antioxidant properties that can be extracted from fruits or obtained from chemical synthesis. Micronized purified flavonoid fraction (MPFF) (Servier), which is obtained from orange peels and contains 90% diosmin and 10% hesperidin, is the most widely used venoactive drug worldwide and the most evaluated diosmin compound. It can potentiate the norepinephrine-induced vein constriction to reduce leukocyte adhesion, migration, and protein leakage and to increase the lymphatic pulsatile flow, resulting in an effective reduction in venous symptoms.
Recently, a new, once-daily 1000 mg oral suspension of MPFF was evaluated in an international, randomized, double-blind, parallel-group study. A total of 1139 symptomatic individuals classified as C0s to C4s according to the clinical, etiological, anatomical, and pathophysiological (CEAP) classification were randomized to either treatment arm and treated for 8 weeks. Lower limb symptoms (discomfort, pain, and heaviness) were assessed using a visual analog scale (VAS), and quality of life (QOL) was measured with the ChronIc Venous dIsease Questionnaire (CIVIQ-20). Both MPFF treatment regimens were well tolerated and associated with a significant reduction in lower limb symptoms. There was a noninferiority of the once-daily treatment with the MPFF 1000 mg oral suspension compared with the twice-daily treatment with MPFF 500 mg tablet (P<0.0001) for lower limb discomfort (-3.33 cm for MPFF 1000 mg vs -3.37 cm for MPFF 500 mg), leg pain (-3.27 cm for MPFF 1000 mg vs -3.31 cm for MPFF 500 mg), and leg heaviness (-3.41 cm for MPFF 1000 mg vs -3.46 cm for MPFF 500 mg). The patients’ QOL improved by about 20 points on the CIVIQ scale in both groups (19.33 points for MPFF 1000 mg and 20.28 points for MPFF 500 mg).
Therefore, the MPFF 1000 mg oral suspension and the MPFF 500 mg tablet treatments were associated with similar reductions in lower limb symptoms and improvements in QOL. The new once-daily MPFF 1000 mg oral suspension has a similar safety profile as two tablets of MPFF 500 mg, with the advantage of a once-daily intake, potentially associated with improved patient adherence and easier management of chronic venous disease. Regarding the clinical efficacy of this drug on edema, eight trials evaluating ankle perimeters and a recent meta-analysis showed positive results; however, three studies estimating water displacement volumetry failed to show a clear efficacy. Therefore, due to methodological problems in assessing edema, no clear conclusions can be made.
Finally, the clinical efficacy of the compound in the treatment of venous ulcers was investigated in two randomized controlled trials. A significant reduction in healing time was observed, but the primary end point of the studies was not achieved. In conclusion, MPFF (and probably other diosmin compounds) is effective in improving venous symptoms in patients with chronic venous disease for all CEAP “C” classifications, with a very good safety profile. They probably also have mild positive effects on venous edema and venous ulcer healing, although further evaluations are needed. They are complementary treatments that should never be prescribed alone and should not be given without an etiological evaluation and treatment of the associated venous disease or venous dysfunction secondary to locomotor problems or lifestyle. They should be prescribed for at least 1 month before evaluating their efficacy in a given patient and their usefulness should be reassessed every 3 to 6 months.
Platelet inhibitors: what is new?
Inhibition of platelet aggregation can reduce the rate of vascular events in patients with coronary artery disease, carotid artery stenosis, and symptomatic peripheral arterial disease. The choice of platelet inhibitors either for monotherapy or combination therapy, as well as the duration of dual platelet inhibition depend on the clinical situation and individual patient characteristics. A large number of randomized trials on platelet inhibition in different clinical situations have been performed, allowing evidence-based recommendations on the choice of drugs and duration of treatment. Moreover, new guidelines from the European Society of Cardiology have recently been published. Based on all of this evidence, a number of recommendations on platelet inhibition after acute coronary syndromes (ACS) and elective percutaneous coronary interventions (PCI) can be made. Combined antiplatelet and anticoagulant therapy should be used in the presence of coronary artery disease (PCI/stenting) and/or peripheral vascular disease with coexisting atrial fibrillation (AF) or venous thromboembolism. After an ACS, it is recommended only in the short-term phase of treatment. Moreover, combined therapy might also be considered in patients with antiphospholipid syndrome and arterial events or in patients suffering from myeloproliferative neoplasm with thrombosis.
In the WOEST trial (What is the Optimal antiplatElet and anticoagulant therapy in patients with oral anticoagulation and coronary StenTing), patients receiving warfarin and undergoing PCI were randomized to clopidogrel alone (double therapy) or clopidogrel and aspirin (triple therapy). The use of clopidogrel without aspirin was associated with a significant reduction in bleeding complications and no increase in the rate of thrombotic events. More recently, a number of randomized controlled trials have been performed to assess direct oral anticoagulants combined with antiplatelets in these settings. The PIONEER-AF trial (Prevention of Bleeding in Patients with AF Undergoing Coronary Stent Placement) compared rivaroxaban with warfarin and randomized 2124 patients to rivaroxaban 15 mg once daily with a single P2Y12 inhibitor for 12 months (group 1; WOEST-like); rivaroxaban 2.5 mg twice daily with dual antiplatelet therapy (DAPT) for 1, 6, or 12 months at the operators discretion, then, as needed, rivaroxaban 15 mg once daily plus aspirin until 12 months (group 2; ATLAS ACS 2-like [Anti-Xa Therapy to Lower cardiovascular events in Addition to Standard therapy in subjects with Acute Coronary Syndrome]); or warfarin with DAPT for 1, 6, or 12 months at the operator’s discretion, then, as needed, warfarin plus aspirin until 12 months (group 3; triple therapy). DAPT duration was 1 month in 16%, 6 months in 35%, and 12 months in 49% of the patients. Clopidogrel was the P2Y12 inhibitor used in 95% of cases. Clinically relevant bleeding was reduced in patients receiving rivaroxaban vs warfarin (group 1 [16.8%] and group 2 [18%] vs group 3 [26.7%]; P=0.001 for both).
In the COMPASS trial (Cardiovascular Outcomes for People using Anticoagulation StrategieS), 27 395 participants with stable atherosclerotic vascular disease (coronary artery disease [CAD] or peripheral artery disease [PAD]) were randomly assigned to receive rivaroxaban (2.5 mg twice daily) plus aspirin (100 mg once daily), rivaroxaban (5 mg twice daily), or aspirin (100 mg once daily). The primary outcome was a composite of cardiovascular death, stroke, or myocardial infarction. The study was stopped due to the superiority of the rivaroxaban plus aspirin group after a mean follow-up of 23 months. In the RE-DUAL PCI trial (Randomized Evaluation of DUAL antithrombotic therapy with dabigatran versus triple therapy with warfarin in patients with nonvalvular AF undergoing a PCI), 2725 patients with AF who had undergone a PCI were randomly assigned to triple therapy (warfarin + a P2Y12 inhibitor [clopidogrel or ticagrelor] + aspirin) for 1 to 3 months or dual therapy (dabigatran [110 mg or 150 mg twice daily] + a P2Y12 inhibitor [clopidogrel or ticagrelor], but no aspirin. The risk of bleeding was lower among those who received dual therapy than among those who received triple therapy. Dual therapy was not inferior to triple therapy with respect to the risk of thromboembolic events. Other ongoing studies assessing the combined therapy with apixaban (AUGUSTUS) and edoxaban (ENTRUST-AF-PCI) in this setting are still ongoing.
Role of sulodexide in the management of venous thrombosis
Sulodexide is a natural glycosaminoglycan with antithrombotic and profibrinolytic activities that can be administered orally or parenterally and affects normal hemostasis to a lower extent than heparin with a very low risk of bleeding. Sulodexide exerts its actions by forming a complex with antithrombin and heparin cofactor II and by inhibiting some factors of the coagulation cascade. These pharmacological and clinical profiles suggest that sulodexide may have a role in the prevention of a venous thromboembolism when a vitamin K antagonist is discontinued. In the recent SURVET trial (SUlodexide in secondary prevention of Recurrent deep VEin Thrombosis), 615 patients with a first venous thromboembolism who had completed 3 to 12 months of oral anticoagulant treatment were randomly assigned to sulodexide 500 lipasemic units twice daily or placebo for 2 years, in addition to elastic stockings. Venous thromboembolism recurred in 15 of the 307 patients who received sulodexide and in 30 of the 308 patients who received placebo (hazard ratio, 0.49; 95% CI, 0.27- 0.92; P=0.02). Therefore, sulodexide given after discontinuation of anticoagulant treatment reduced the risk of recurrence in patients with an unprovoked venous thromboembolism, with no apparent increase in the risk of bleeding.
An update on antifibrinolytic agents
Tranexamic acid (TXA) is a lysine analog that, by reversibly binding to plasminogen, inhibits its interaction with fibrin and therefore its activation of plasmin. TXA is used clinically for its ability to inhibit fibrinolysis. Moreover, it also showed beneficial anti-inflammatory properties in cardiac surgery. Protective effects can also be expected with respect to the blood brain barrier opening based on in vitro studies. Therefore, a possible reduction in hemorrhage and edema due to inhibition of tissue plasminogen activator (tPA)-plasmin mediated disruption of the blood brain barrier has been suggested. However, other effects of the tPA-plasmin system could become impaired by competition with lysine residues with TXA or related agents. Although this remains to be formally demonstrated, TXA might attenuate tPA-plasmin–mediated wound healing, as well as the clearance of misfolded proteins after cell death; both processes are highly dependent on plasminogen. TXA could also potentially block various central nervous system functions that are known to be associated with tPA activity, including glutamate receptor activation, behavior, and learning, although the plasminogen dependency in these processes is unclear. The use of TXA in cancer in vivo has yet to be reported, but it has been shown to potentially limit metastatic cell migration in vitro by modulating the proteolytic profile of the tumor microenvironment. With respect to its use in severe trauma patients, in the CRASH-2 trial (Clinical Randomization of an Antifibrinolytic in Significant Head injury), a prospective, randomized, placebo-controlled multicenter study, TXA significantly decreased the risk of death due to bleeding if injected within 3 hours after injury and it was more effective when administered within the first hour. However, when TXA was administered after 3 hours, the risk of death due to hemorrhage was higher than in the placebo group. In traumatic brain injury, TXA treatment did not show a significant difference compared with placebo regarding the outcome, yet a trend suggesting beneficial effects was observed. This trial has been criticized mainly because blood samples were not drawn, so it was not possible to relate the effects of TXA to the presence or absence of acute traumatic coagulopathy. The need for a prospective randomized trial, with coagulation monitoring and standardized transfusion protocols, has been proposed and is currently underway. TXA is certainly considered a very safe drug and is generally used for short-term fibrinolytic blockade purposes only, potentially minimizing its potential adverse effects. On the other hand, investigations on prospective applications, unrelated to its traditional indications, might provide new challenges.
Venous Reflux
Venous reflux is not sufficient to assess venous disease
Van Rij stated that the treatment of reflux is ablation, which it seems to work most of the time, and that duplex ultrasound is very efficient and productive for diagnosis of venous reflux. However, venous disease is not all about reflux, as in the case of obstruction, muscle pump disorders, perforators, wall compliance, vascular remodeling, and microcirculation. The speaker emphasized that we do not even fully understand reflux and its relationship to function/clinical severity, treatment response, ultrasound test, disease severity, quality of life, symptoms, and symptom severity. Reflux ablation is not the only treatment for reflux in venous disease, but also weight loss, compression, valve reconstruction, banding, reassurance. To assess venous disease, we need other tools, such as clinical classification (clinical, etiological, anatomical, and pathophysiological [CEAP]), clinical severity (venous clinical severity score [VCSS]), imaging segmental score (venous severity scoring [VSS]), and patient-focused tools (QOL). Historically, we used ambulatory venous pressure measurements, plethysmography, and capillaroscopy to evaluate hemodynamic and functional parameters. In the future, efforts should be invested in quantitative hemodynamic/functional biomarker research; for example, the Parana and Vasculab maneuvers, venous recirculation index, venous drainage index, skin microcirculation, and elastography.
Progression of reflux patterns in saphenous veins
A distribution of the clinical, etiological, anatomical, and pathophysiological (CEAP) classifications in the population showed that the worldwide prevalence of varicose veins and chronic venous insufficiency (CVI) was 23.2% and 17% for both sexes, respectively. In a study done by Labropoulos et al, of 116 limbs, 11% showed a progression in the clinical stage several months after the first exam, 14.7% had an extension of the preexisting reflux, and 14% had reflux in a new segment. After 5 years, there were new sites of reflux in 52% of the limbs and 50% of the patients with unilateral varicosities developed chronic venous disease in the contralateral and initially asymptomatic limb. Independent risk factors for chronic venous disease (CVD) progression were obesity, orthostatism, and noncompliance with compression. Another Italian study on 104 limbs showed that, after a mean follow-up of 4 years, there was an extension of the reflux. In most cases, the reflux progressed from a lower to a more proximal location in the leg. In a follow-up study on 304 patients who were on a waiting list for varicose vein surgery, after 4 years, 64% reported progression of the disease, 5% developed a superficial vein thrombosis, 22% developed skin changes, and 12% developed venous leg ulcers. The risk factors for chronic ulceration in patients with varicose veins include lipodermatosclerosis, corona phlebectatica, eczema, higher body mass index, and popliteal vein reflux. Rabe emphasized that corona phlebectatica is a predictor for the development of CVI. In summary, varicose veins and CVI are very common in the worldwide population, the risk factors differ significantly between varicose veins and CVI, and the progression of reflux, varicose veins, and CVD is very frequent. A large proportion of uncomplicated varicose veins develop skin changes and CVI. In a 13.4-year follow-up period, 57.8% of all patients with chronic venous disease showed disease progression.
Venous reflux may not be relevant when ablating veins
Bradbury stated that there is no relationship between varicose veins and venous symptoms. The Edinburgh vein study, a cross-sectional population survey, concluded that, even in the presence of trunk varices, most of the lower limb symptoms probably have a nonvenous cause. Therefore, surgical extirpation of trunk varices is unlikely to ameliorate such symptoms in most patients. This study showed no relationship between reflux and venous symptoms. A randomized controlled trial comparing endovenous laser ablation, radiofrequency ablation, foam sclerotherapy, and surgical stripping for great saphenous varicose veins showed a poor relationship between abolition of truncal reflux and patient-reported outcomes after varicose vein treatment. In this study, recanalization and reflux after ultrasound-guided foam sclerotherapy were much worse, but there was absolutely no difference in the Venous Clinical Severity Score or Aberdeen Varicose Vein Questionnaire score between all treatments. Another study investigated the rates of duplex-detected recanalization 5 years after ultrasound-guided foam sclerotherapy and the relationship with clinical signs, hemodynamics, and patient-reported outcome measures. Although there were considerable rates of recanalization on duplex ultrasound, the overall patient satisfaction did not significantly differ between patients with fully occluded veins and patients with partially occluded or open veins. A review of randomized controlled trials comparing ultrasound-guided foam sclerotherapy with endovenous laser ablation for the treatment of the great saphenous vein indicated that differences in technical success did not relate to differences in clinical (patients-reported) outcomes in any of the randomized controlled trials and the value of “technical success’ as a useful end point is questionable.
Recurrent Varicose Veins
Results of treatments of recurrent varicose veins, history-based review
Duplex ultrasound scans make it possible to observe all details and reasons for recurrences including: (i) neovasculogenesis, demonstrating the importance of lymph nodes veins in postsurgical recurrences; (ii) importance of junctional tributaries moving into the junction (preserved during ablation therapy); (iii) recognition of the association of pelvic reflux with pelvic congestion syndrome; (iv) distinction between the great saphenous vein trunk (intrafascial) and larger tributaries (extrafascial); and (v) moderate recurrent reflux in reduced trunks: to treat or just to follow-up? (thermal and chemical ablations).
Recurrences sometimes occur at the saphenofemoral junction, especially if thermal ablation has been stopped at a distance from the junction (Nelzén O. Br J Surg. 2016;103(8):939-940), and sometimes at the same site by recanalization, mostly after endovenous laser treatment, but frequently at another site, especially after surgery (Rass K et al. Eur J Vasc Endovasc Surg. 2015;50(5):648-656; O’Donnell TF et al. J Vasc Surg Venous Lymphat Disord. 2016;4(1):97-105). Since high ligation and division was considered the cause of REVAS, stripping without high ligation (comparable with ablations) has been proposed (insufficient studies). Surgery without stripping has been proposed too (CHIVA, ASVAL) with very limited evidence so far. However, modern open surgery gives good results too (Rasmussen L et al. J Vasc Surg. 2013;58(2):421-426).
The truth about surgery is that good surgeons using a good modern surgical technique have good results (preoperative duplex marking, limited/ambulatory anesthesia, either no ligation/division or correct ligation and careful division of tributaries beyond the second branch, invagination stripping, or pin stripping (Rasmussen), microphlebectomy in the same session, immediate ambulation, and reduced compression). There is slightly more immediate discomfort than ablations. Certain treatments, such as mechanochemical endovenous ablation, laser-assisted foam sclerotherapy, and cyanoacrylate glue, still lack long-term follow-up. Recurrences from these treatments may be similar in aspect, if not in figures, to that of endovenous ablations. Ultrasound-guided sclerotherapy is fit for almost all cases of recurrence (except a major mistake in the initial management, such as error concerning the trunk or side). In the short-term, ultrasound-guided sclerotherapy is the best and surgery is the worst, but in the long-term, all methods are comparable.
Ultrasound examination of recurrent varicose veins
The recurrence rate of varicose vein treatment may vary up to 50% 5 years postsurgery. The duplex-based recurrence rate is usually higher than the clinical one, as many refluxing veins may not be clinically relevant. Color duplex ultrasound highlights different morphohemodynamic patterns related to recurrence after surgery or endovenous thermal/chemical ablation. Adequate settings (eg, low PRF) and operator skill objectively influence the accuracy of color duplex ultrasound investigations. A few of the possible causes of recurrence include progression of the disease with newly formed (refluxing or not) varices in the treated limb or pelvic refluxes, (neo) vascularization in the groin and popliteal areas or in the saphenous compartments, technical and tactical mistakes with residual refluxing veins, subsiding deep vein abnormality. Color duplex ultrasound after the treatment of varicose veins is used to detect any new or persistent source of reflux from a residual saphenous junction stump, inguinal or popliteal varicose network, accessory saphenous vein, perforators, nonsaphenous veins (eg, pelvic, perineal, gluteal, sciatic nerve varices). In a few cases, recurrent refluxes are not associated with any escape points from the deep veins. Color duplex ultrasound–based follow-up has a 100% predictive value for clinical recurrence at 5 years. Postsurgery recurrence may differ from postendovenous ablation recurrence, as the latter presents a much lower groin/popliteal neovascularization rate (typical of surgery) and possibly degree of recanalization of the treated stem. After treatment of varicose veins, the combination of color duplex ultrasound investigation with clinical assessment (symptoms in primis) represents the best approach to followup and possibly suggest an adequate retreatment.
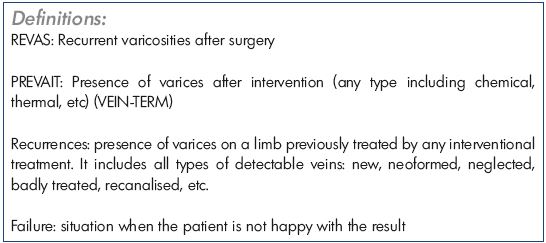
Are recurrent varicose veins after endovenous treatment or after surgery so different?
The term PREVAIT (PREsence of VArices after Interventional Treatment) has replaced the term “recurrent varicose veins”. The residual and recurrent varicose veins have to be differentiated in patients with PREVAIT. Residual varicosities depend on the pretreatment distribution of varicose tributaries. Varicosities in direct connection with the refluxing trunk may tend to shrink after endovenous ablation (EVA), whereas other varicosities, related to other “escape points” may persist. Such residual varicose veins may be treated after a certain interval by means of phlebectomies or foam sclerotherapy. Surgery (consisting of high ligation and stripping) usually includes phlebectomies from the start, which means there should not be residual varicose veins immediately after a well-performed surgery. Hence, the difference in residual varicose veins after both approaches mainly depends on the timing of the assessment. Recurrent varicose veins reappear at the same site or a different site of the previously treated truncal and tributary veins. Randomized clinical trials with a long-term follow-up of at least 5 years (so far mainly comparing endovenous laser ablation with surgery) have clearly shown there is absolutely no difference in the incidence of clinically obvious recurrent varicose veins (40% to 50%), which is also reflected by the lack of difference in the venous clinical severity score and the disease-specific quality of life scores containing the presence of varicose veins as an item to be scored (eg, Aberdeen Varicose Vein Symptom Severity Score and Homburg Varicose Vein Severity Score). On the contrary, what is clearly different is the duplex ultrasound appearance, with different duplex ultrasound patterns of recurrence after EVA compared with those after surgery. At the saphenofemoral junction (SFJ), recurrent reflux may be observed. After surgery of the great saphenous vein (GSV), neovascularization is seen more frequently, whereas, after EVA, refluxing SFJ tributaries appear to be more frequent, which results in a significantly higher rate of recurrent varicose veins originating from the SFJ region after EVA than after surgery. A typical anatomic pathway of recurrence after EVA is (persistent or recurrent) reflux at the SFJ and the anterior accessory saphenous vein (AASV), reported in 20% to 40% of treated limbs. In 5% to 15% of treated truncal veins, segmental or complete recanalization may occur after an initial successful obliteration of the trunk, which is obviously not the case after successful stripping of the target vein, although so called “revascularization of the strip track” may occur and result in clinical recurrence. Perforating veins may also play a role in recurrence, although the available literature is conflicting and it cannot be concluded whether their incidence and role in recurrence is different between surgery and EVA. Finally, new sites of reflux may be due to progression of the disease resulting in clinical recurrence, both after EVA and after surgery.
Sclerotherapy of recurrent varicose veins (strategy and technique)
According to the literature, the rate of recurrent varicose veins is between 13% and 65%. All types of recurrent varicose veins can be treated by foam sclerotherapy, including: (i) residual, recurrent, recanalized varicose veins, with or without intraluminal adherences; (ii) tortuous, straight, interfascial, subcutaneous varicose veins; (iii) thermal ablation or foam sclerotherapy after surgery; (iv) with or without an existing connection with the femoral vein and/or popliteal vein; and (v) perforating veins, accessory saphenous veins, communicating veins, lymph node veins, pudendal veins, reticular veins, telangiectases, etc. The most common situations are recurrence at the trunk, the upper thigh, and in the popliteal fossa. Recurrent varicose veins are a major indication for foam sclerotherapy. Foam sclerotherapy is efficient, helpful, economical, fast, and well accepted by patients. The technique varies little from that used for primary varicose veins, but good skills are required and a direct puncture technique with a needle appears to be more adequate. Treatment of small recanalizations is questionable.
Varicose veins after treatment: recurrence or progression?
The prevalence of varicose veins (C3-C6) is 23.2% and the prevalence of chronic venous insufficiency is 17%. The reasons for recurrence of varicose veins after treatment include early recurrence due to an insufficient primary treatment (technical failure), late recurrence due to recanalization of the treated veins (insufficient energy level, insufficient sclerotherapy application), and new varicose degeneration in previously untreated veins. Recanalization of treated veins after endovenous thermal ablation occurs at a higher rate with a linear endovenous energy density (LEED) below 60 J/cm, a greater diameter of the great saphenous vein, and untreated side branches may lead to recanalization of the connected saphenous segment. Recanalization may occur after sclerotherapy when: (i) a low concentration of sclerosant (liquid or foam) is used in vein diameters >0.7 cm, as this leads to insufficient damage to the venous wall; (ii) foam is injected into the saphenous junction in a site that is too distal, as this causes incomplete damage of the proximal intima due to absorption of the sclerosant at surfaces near the injection site; and (iii) side branches are untreated as this may lead to recanalization of the connected saphenous segment. Treatment of existing varicose veins may ablate the varicose veins, but it cannot cure the varicose disease itself. A genetic predisposition may lead to further development of new varicose veins or to the progression of existing varicose veins, which may happen close to the initial treated veins, at other sites, or even in the other leg, and untreated side branches may progress to multisegmental varicose veins.
Recurrent varicose veins after thermal ablation of the great saphenous vein
All published long-term results after endovenous laser ablation (EVLA) have been performed with bare fibers and 2 cm from the junction, which leads to a higher rate of persistent flow and reflux in the persisting great saphenous vein stump, and new reflux in the anterior accessory saphenous vein (AASV) during follow-up is a possible consequence. Overall recurrence rates and improvement in quality of life and symptoms are equal with high ligation and stripping. With higher wavelengths and radial fibers, an occlusion close to the deep vein can be achieved, avoiding a longer stump, which may influence AASV recurrence rates, but long-term results are not available. A relatively long stump after EVLA may lead to persistent reflux and to later clinical recurrence. With radial fibers, the stump could be reduced to a quasi-high ligation situation.
In the last 15 years, the treatment of varicose veins has changed. The most important clinical outcomes are improvements in quality of life and the severity of the disease (symptoms). EVLA has become a standard treatment option, and higher wavelengths and radial fibers significantly reduce side effects, such as pain and bruising. Recurrent varicose veins after EVLA develop after early recanalization (technical failure), as incompetent AASV, or as natural history with progression of the disease. A long stump after EVLA may be the reason for persisting or recurrent reflux in the saphenofemoral junction region and for AASV recurrences. An initial laser crossectomy may not lead to stable results, but to a shorter stump. Recurrent varicose veins from groin reflux develop after years, which may be easily treated by foam sclerotherapy or other methods. All methods show similar results concerning improvement in quality of life and symptoms.
How to prevent progression and recurrence of varicose veins?
Varicose veins are present in 23% of the adult population and chronic venous insufficiency is present in 11% to 17% of the adult population. For chronic venous disease (CVD), the progression rate to higher clinical stages reaches 4% per year. Half of the patients with unilateral varicosities develop contralateral CVD in several years. One-third of patients with varicose veins (C2) will develop skin changes in 13 years. The recurrence rates for varicose veins are very high: 40% to 50% at 5 years and 70% at 10 years. Of the surgical procedures, 20% are carried out to treat recurrent disease. Poor surgery (failure to identify the source of reflux, surgical ligation without stripping, etc), treatment failure (recanalization after ultrasound-guided foam sclerotherapy, recanalization after EVTA, etc), recurrence of pelvic origin (recurrent varicose veins of the upper medial thigh, perianal, gluteal, or posterior thigh), changes in hemodynamics (incompetent anterior accessory saphenous vein after great saphenous vein ablation), perforating veins, neovascularization, progression of the disease (accounts for 20% to 50% of recurrences) can be the causes. Risk factors for venous disease include a positive family history of CVD, pregnancy, obesity, standing/ sitting habit, smoking, lack of regular exercise, female sex, and age. Among these risk factors, age, sex, and family history are immutable; however, weight, physical activity, and smoking can be modified. Compression improves venous pump function and enhances venous flow velocities. At various stages of CVD, compression significantly reduces edema, improves symptoms, and has a positive effect on patients’ quality of life. There is insufficient information from randomized controlled trials on preventing CVD progression with compression; however, the incidence of CVD progression is higher among patients who are noncompliant with compression stockings. Antiinflammatory treatment options, such as micronized purified flavonoid fraction (MPFF), reduces the expression of adhesion molecules, reduces the adhesion of leukocytes to the endothelium, decreases capillary permeability, and improves venous tone, suggesting a reduction in the progression of CVD. Sclerotherapy (foam), surgery, endovenous techniques, and other interventional techniques provide clinically significant improvements to patients’ quality of life. Progression of disease in most patients is not preventable, as the causes of varicose recurrence are multifactorial and only some of them can be prevented.
Pelvic Venous Disease
Abdominal and pelvic venous anatomy and pathophsyiology – the need for a new descriptive instrument
The female pelvic venous drainage is complex, with contributions from the ovarian veins, the internal iliac veins, and the common femoral vein. These three drainage territories are interconnected with frequent cross-pelvic drainage. Pelvic congestion syndrome (PCS) arises from reflux in the ovarian and/or internal iliac veins leading to pelvic varicosities and associated symptoms. Communications from the internal iliac veins via the saphenofemoral junction may also lead to vulvar, perineal, and lower extremity varices. Pelvic reflux is possibly related to both mechanical factors, primarily a 60-fold increase in pelvic blood flow during pregnancy, and endocrine factors. At least some data suggest that the ovarian veins, which are typically exposed to very high estrogen concentrations during the menstrual cycle, are disproportionally sensitive to estrogen-mediated vasodilation. Venodilation of the ovarian and internal iliac tributaries leads to valvular incompetence, venous reflux, and pelvic varices. Less commonly, reflux in the left ovarian and internal iliac systems arises from proximal compression of the left renal or iliac veins. Pelvic symptoms related to venous reflux most commonly occur in multiparous women of reproductive age, an important consideration in the management of these patients. PCS is characterized by chronic pelvic pain present for at least 6 months with variable symptoms of dyspareunia, dysuria, and dysmenorrhea. Pelvic pain is noncyclic, meaning that it is a background symptom and it is often present throughout the month, but typically worsens with menstruation as well as intercourse and prolonged standing. Postcoital pain is often described as a bursting or aching sensation that may take several hours to resolve. Pelvic venous reflux may also manifest as varicose veins, occurring either alone or in combination with chronic pelvic pain. These may develop in atypical locations (vulva, perineum, or buttocks) or, by way of communication with the superficial and deep external pudendal veins, in a great saphenous distribution. Although not all women with atypical varices have pelvic pain, approximately one-third of those with PCS have vulvovaginal varices and up to 90% may have lower limb varices. Conversely, approximately 5% of women presenting with lower extremity varicose veins will have concurrent pelvic symptoms. It is important to note that pelvic varicosities do not uniformly lead to disabling symptoms. Asymptomatic varicosities have been reported in 38% to 47% of women patients undergoing CT or MRI.
Treatment algorithm for pelvic reflux
Patterns of pelvic reflux can be diverted to two anatomic components as superior and inferior. Superior reflux has a competent floor leading to uncompensated pelvic hypertension presenting with pelvic symptoms. On the contrary, inferior reflux occurs on an incompetent floor with compensated pelvic hypertension with/without pelvic symptoms. The indication of an inferior component is leg symptoms, which requires treating the pelvic source from below and treating the leg varicosities. Treatment of a superior component consists of treating the reflux and releasing the compression. For symptomatic pelvic veins, sclerotherapy and embolization are therapeutic options, while ultrasound-guided and fluoroscopy-guided sclerotherapy can be used for lower extremity varices.
Pelvic venous reflux or obstruction
Primary pelvic congestion syndrome (PCS) is due to an increase in ovarian, uterine, and pelvic volumes due to multiple pregnancies and estrogenic effects; primary PCS comprises 10% of all cases of PCS. Secondary PCS is present in the other 90% of PCS cases, and it is due to venous outflow obstruction, which can result from a nonthrombotic iliac lesion (NIVL), a retroaortic left renal vein, or the nutcracker phenomenon. NIVLs result from a high-pressure zone at the origin of the left common iliac vein. The cause of the thrombosis is May-Thurner syndrome leading to iliofemoral reflux and this effect is enhanced in obese patients. In a patient series, 18 patients with NIVL and PCS, of which 7 also had ovarian reflux, were treated with iliac vein stenting. The pelvic pain was completely resolved in 15 patients, and further dyspareunia disappeared in 14 of these 15 patients with a follow-up to 59 months. Hemodynamic assessment of venous outflow obstruction and an intravascular ultrasound are essential for determining the ovarian/iliac vein origin. Stenting of the iliac venous outflow in a properly diagnosed pathology provides significant relief of symptoms.
Treating ovarian veins with laser and glue ablation
For pelvic congestion syndrome (PCS), imaging consists of transvaginal duplex ultrasound, venography, CT, and MRI. PCS can be separated into three grades with increasing severity, and, depending on the severity, therapeutic options can be listed as drugs, hysterectomy, open and laparoscopic surgery, and endovascular treatments. In one series of eight patients, the average age was 26.21±3.14 years with grade 3 reflux in all patients. The most common symptoms and signs of PCS were listed as pain, prolonged postcoital discomfort, and lack of positive changes upon vaginal examination. A Doppler ultrasound revealed a dilatation of the uterine venous plexus and left ovarian vein, retrograde ovarian venous flow, and reflux of the pelvic vein without any obstructing anatomic anomalies. A CT examination revealed dilatation of the pelvic veins, no signs of pelvic inflammatory disease, and no signs of obstructing lesions. In this series, all patients were treated with a combination of endovenous ablation and distal foam sclerotherapy. After the ablation procedures, repeat venography was performed to confirm occlusion of the ovarian vein. In the series, there was a 12-year-old girl with PCS, suggesting that congenital venous malformations may also be a causative factor in PCS.
How common is nutcracker syndrome in patients presenting with pelvic congestion syndrome?
Nutcracker syndrome occurs when the left renal vein is compressed in the aortamesenteric angle, resulting in impedance of flow from the left renal vein to the inferior vena cava. Anterior nutcracker syndrome is more common. Nutcracker syndrome is not caused solely by aorta mesenteric compression, but it can also result from pancreatic neoplasm, abdominal aortic aneurysm, left inferior vena cava obstruction, persistent left superior vena cava with hemiazygous continuation. The symptoms and signs vary between hematuria and PCS. In a study by Takobayashu et al, 44 patients with hematuria and nutcracker syndrome were analyzed by Doppler ultrasonography, retrograde renal venography, and renocaval pressure measurement. The flow patterns were characterized by left renal vein distension on ultrasound and reflux on venography. Of these patients, 21 showed no distension of the left renal vein, with 19 patients showing no collateral pelvic veins or hypertension. It is difficult to define the true incidence of nutcracker syndrome in PCS. About one-third of patients with nutcracker syndrome show pelvic venous collateralization with increased renocaval pressures and two-thirds of the patients improve with iliac vein stenting. One-third of the cases of secondary PCS may stem from the nutcracker syndrome and the rest from nonthrombotic iliac lesions. Renal vein embolization in PCS without intraprocedural evaluation of retrocaval gradients should not be done. All patients with PCS who are considered for an intervention should have an iliac vein evaluation for nonthrombotic iliac lesions, including an intravascular ultrasound. Duplex assessments must include renal vein velocity.
Patterns of pelvic venous duplex findings in patients who present with varicose veins
In this series of 313 patients, all had been scanned for iliac vein pathology (compression), renal vein compression, gonadal vein reflux/dilation, and internal iliac vein reflux. Veins were checked for reflux, thrombus, and diameter ratios. Gonadal vein dilatation relationships for left renal vein compression and left inferior vena cava compression were investigated, and, in this protocol, normal was considered to be up to 4 mm at the largest point. In addition, the junction with the renal vein at the pelvic brim and the relationship between nutcracker syndrome and incompetence of the gonadal vein was evaluated. The results from this patient series showed a decrease in both the incidence of May-Thurner syndrome with age and the incidence of renal vein compression after 50 years of age. Left ovarian vein insufficiency tends to increase in the middle age, but then it decreases. In conclusion, the considerations should be directed to the pattern of pathology, recording the diameter as well as the direction of flow in the ovarian vein, the cause of the dilation of the ovarian vein, and the precision of the treatment plan.
Does left ovarian vein reflux cause a pseudo-nutcracker effect creating mesoaortic narrowing of the left renal vein?
In this series of 58 patients, to control for the successful embolization/abolition of reflux, it was suggested to examine the exclusion of coil migration and reflux in previously nonrefluxing (untreated) veins, compare any changes in appearance or caliber of the left renal vein, and document residual labial varices 6 to 8 weeks after pelvic vein embolization. The diameters and ratios of the hilar and mesoaortic left renal vein were recorded at diagnosis and after pelvic vein embolization. A hilar to mesoaortic diameter ratio >5 raised the suspicion of nutcracker phenomena.
In group 1 (n=24 patients), all patients exhibited proximal and distal left ovarian vein reflux prior to pelvic vein embolization. In this group, 5 patients demonstrated reflux in both internal iliac veins and both ovarian veins, 9 patients demonstrated reflux in the left ovarian vein and both internal iliac veins, 3 patients presented with debilitating pelvic congestion syndrome (PCS), but no leg varicose veins, and 15 patients presented with leg varicose veins and moderate to severe pelvic symptoms, while 6 patients presented with leg varicose veins and pelvic communication/pelvic varices, but no significant pelvic symptoms. In group 2 (n=26 patients), 14 of whom had no reflux observed in the left ovarian vein and 12 exhibited reflux in the distal segment of the left ovarian vein, 3 patients presented with debilitating PCS, but with no leg varicose veins, and 23 patients presented with leg varicose veins and pelvic varicosities. In group 3 (n=6 patients), all exhibited proximal and left ovarian vein reflux prior to pelvic vein embolization.
This study showed that left ovarian vein reflux appeared to cause a syphon effect with left renal vein drainage preferentially following the left ovarian vein reflux path, which results in a physiologic narrowing of the mesoaortic left renal vein.
Analysis of a retrospective pelvic embolization audit for the evaluation of postembolization symptoms
In this study, the type, severity, and duration of postembolization symptoms up to 30 months were analyzed. Pelvic vein embolization was performed by coil embolization and foam sclerotherapy under local anesthesia, and contrast venography was used with a transjugular or transbrachial approach. A questionnaire was sent to 206 patients and the response rate was 32%. The most common symptoms were postprocedural pain (69%) and flu-like symptoms (39%). The mean follow-up was 13 months, and the age range was 33–76 years old. Of these patients, 40% showed a total absence of reflux, 44% had mild distal reflux, and 1.6% experienced a technical failure. Flu-like symptoms lasted 1 to 2 days in 42% of patients, 3 to 4 days in 29%, and >5 days in 29%. In conclusion, the majority of these patients said that the procedure affected their ability to perform daily activities for 1 week to 1 month.
Assessing reflux patterns and the results of endovascular obliteration of ovarian veins in patients with symptomatic pelvic venous incompetence
The clinical clues of pelvic venous incompetence (PVI) can be outlined as vaginal varicosities during pregnancy, dyspareunia, lower abdominal pain, or atypical varicose veins sites, such as the groin, posteromedial thigh, and vulvar, gluteal, and perineal areas. A duplex ultrasound study analyzed both the cranial (epigastric) and medial (pubic and pudental) areas. The study included 154 female patients who were between 20 and 50 years old, with at least 1 full-term pregnancy. Risk factors were pregnancy, estrogen exposure, obesity, pelvic surgery, phlebitis, prolonged standing, and heavy lifting. The venous patterns observed were posterior thigh (36.84%), gluteal (13.15%), vulvar (42.10%), pubic (5.26%), right sided (52.63%), left sided (65.78%), and bilateral (50%). All patients were scanned by venous duplex scan with linear, convex, and transvaginal probes in a standing and a lying position. The prevalence of pelvic venous reflux was 31.46%. During pregnancy, the vein capacity increases up to 60% and may remain enlarged for 6 months postpartum. Estrogen, nitric oxide, and polycystic ovaries are physiological factors for PVI, while absent valves of the ovarian and internal iliac veins, as well as mechanical compression are anatomic factors. In case of combined ovarian vein and internal iliac vein reflux, complete embolization is warranted to improve symptoms. Besides an ultrasound, CT, MR, and venography can be used as diagnostic tools, while direct venography is the gold-standard tool.
Proposal for a clinical score of pelvic congestion syndrome and its validation
Pelvic congestion syndrome (PCS) is one of the possible causes of chronic pelvic pain in women. PCS is described as chronic pelvic pain (CPP) arising from dilated and refluxing incompetent pelvic veins. The diagnosis is based on patient-reported symptoms, clinical examination, anatomical features, duplex scanner ultrasound, magnetic resonance examinations, and venography findings. There are no generally accepted, well-defined clinical criteria for the diagnosis of PCS. The identification of incompetent pelvic veins is essential for the diagnosis of PCS. Noninvasive methods, such as ultrasound and magnetic resonance imaging, are inevitably the first-line investigations, with the assessment of blood velocity and flow pattern being a crucial part of any assessment of pelvic vein incompetence. The authors suggest a simple scoring system to identify the clinical symptoms and signs and the noninvasive diagnostic data (transvaginal ultrasound and magnetic resonance images). The maximum clinical score is 27 (9 signs and symptoms with values from 0 to 3: chronic pelvic pain, dyspareunia, vulvar/perineal varices, atypical leg varices, dysmenorrhea, vulvar congestion, hemorrhoids, premenstrual and menstrual varices pain, sudden urination) and the instrumental score is 10 (1 point for each of the 10 venous districts). The most common ultrasound criteria are tortuous pelvic veins with a diameter >6 mm, mean diameter in PCS ≈8 mm, slow blood flow <3 cm/second or reversed caudal flow in the left ovarian vein demonstrated by Doppler waveforms, and dilated arcuate veins in the myometrium that communicate between the bilateral pelvic varicose veins.
Duplex ultrasound imaging in pelvic venous reflux disease and lessons learned about nutcracker syndrome and “pseudo-nutcracker” syndrome
Whiteley et al (Phlebology. 2015;30(10):706-713) evaluated the use of transvaginal duplex ultrasonography (TVUS) in the diagnosis of pelvic congestion syndrome (PCS) and proposed TVUS as the new gold-standard diagnostic technique. However, this diagnostic imaging modality is limited by the inability to demonstrate the course of the ovarian veins and potential higher obstructions, which may include the nutcracker phenomenon or May-Thurner syndrome. By adding transabdominal duplex ultrasound (TADUS) to TVUS, according to a standardized protocol (Phlebology. 2017;32(9):608- 619), Holdstock et al noticed several common clinical presentations, such as distal ovarian vein reflux in the absence of proximal reflux and the nutcracker phenomena in the presence of proximal left ovarian vein reflux, and, in 10% of patients, variant anatomy, such as collaterals or bifid veins. Furthermore, by placing the patients in the Trendelenburg position and thus inducing postural hemodynamic changes, they were able to exclude a true nutcracker syndrome in many patients. They noted that a pseudo-nutcracker phenomenon is very common rather than a true nutcracker syndrome.
Treatment of pelvic congestion syndrome with foam sclerotherapy: advantages and limits
The definition of pelvic congestion syndrome includes two infrequently overlapping scenarios: (i) pelvic venous engorgement with lower abdomen symptomatology and (ii) lower limb varicose veins fed by pelvic escape points that are generally less prone to the development of the abdominal clinical manifestation that is typical for pelvic congestion syndrome. In a retrospective evaluation, 985 female patients (43±11 years old; 23±5 kg/m2 BMI) had lower limb varicose veins of a pelvic origin. Second-level imaging was needed for 229 patients, and the remaining 756 patients underwent direct echo-guided foam sclerotherapy in the proximity of the pelvic escape points. At a mean follow-up of 4.1±1.4 years, 595 patients were successfully treated. Among the successfully treated group, mild lower abdomen heaviness and occasional dyspareunia was reported by 14 and 11 women, respectively, prior to the injection. At the end of the follow-up period, a significant reduction in the symptomatology was reported for both lower abdomen heaviness and dyspareunia. In traditional pelvic congestion syndrome, an accurate diagnosis protocol eventually ends in an interventional radiology suite. Conversely, in the opinion of the author, in cases of lower limb varicose veins of pelvic origin, the phlebologist can assume a pivotal role both in the diagnostic and therapeutic part.
Transperineal ultrasound-guided foam sclerotherapy for leg varicosities of pelvic origin
Morrison illustrated the main advantages of the transperineal approach of the ultrasound-guided foam sclerotherapy for the treatment of pelvic varicosities. The posteromedial approach can be more comfortable for patients and more physiological for the examiner. It allows for the treatment of difficult escape points with a lower probability of technical errors.
Complications of pelvic vein embolization due to pelvic congestion syndrome
The author presented the results of an observational single-center study that evaluated the complications after pelvic vein embolization in patients with pelvic congestion syndrome caused by primary reflux in pelvic veins. A total of 134 women (mean age, 29.3 years [range, 21-46]; number of pregnancies, 2.9 [range, 1-7]) were followed up for a 60-month period and underwent a clinical examination, a pelvic ultrasound, and a chest x-ray 1, 12, and 60 months after treatment with selective transcatheter pelvic vein embolization. Exclusion criteria were another pelvic pathology, another treatment (surgery, stenting), presence of compression syndrome, and allergic reaction on contrast media, technically unsuccessful cases. A transbrachial access was performed in 38 patients (29%), whereas a transfemoral access was preferred in 96 patients (71%). Coils plus sclerosing foam was the most commonly used treatment (86%). An assessment of severity (grading from 1 to 6 points) was reported for all detected complications. The procedure was technically unsuccessful in only two cases.
No changes in reproductive function were observed (27 patients became pregnant after the treatment). They concluded that pelvic vein embolization is an effective method for the treatment of pelvic venous insufficiency, and it is characterized by high technical success (96% to 100%). The number and severity of complications are very low; this method can be considered safe. Multicenter registries based on unified protocols are needed to make the evidence stronger.
Outflow problems causing pelvic congestion syndrome: being aware!
Routine treatment options for pelvic congestion syndrome (PCS) include embolization of the incompetent veins (99%) and stenting of the obstructive lesions (rare). Treatment of PCS provides around 80% success in the short term and 50% in the long term (>1 year). The 10% increase in complaints could potentially be due to embolization of the kidney outflow in patients with a nutcracker embolization of collaterals and in patients with May-Thurner syndrome or persistent incompetence. The incidence of obstructive lesions causing PCS might be around 10%. In those cases, the treatment should first resolve the obstruction and as a second step, if necessary, treat the incompetence with coiling. For the future, we need disease-specific questionnaires for PCS, better diagnostics, a better follow-up plan, in addition to research analyzing the best treatment options.
Modern understanding of pelvic venous disorders: a new paradigm
According to Mark Meissner, the term “pelvic congestion syndrome” is nonsense and it should be abandoned in favor of “chronic pelvic venous disorders.” Pelvic venous disorders can include four different clinical presentations: chronic pelvic pain (pain, dyspareunia, dysuria); pelvic varices (gluteal, perineal, vulvar); renal symptoms (flank, pain, hematuria); and leg symptoms (pain, swelling). Two patterns of primary reflux (ovarian and internal iliac reflux) and two patterns of obstruction (iliac vein or left renal vein) can be distinguished that determine, in turn, a secondary reflux either in the internal iliac vein or in the ovarian vein. All of the symptoms seem to be related to the abdomen and pelvis venous reservoir distension. All reflux and obstruction can occur according to two patterns: uncompensated (no outflow from the distal reservoir) or compensated (collateral outflow from the distal reservoir). However, these mechanisms can all coexist, so patients can manifest similar symptoms with concordant mechanisms or similar symptoms with discordant mechanisms. In conclusion, four interconnected systems (left renal vein, ovarian veins, internal iliac veins, and great saphenous veins) and two abdominal-pelvic reservoirs (renal hilum and pelvis) should be considered. Symptoms are usually related to reservoir distension, and different patterns of reflux or obstruction can produce identical reservoir distension and symptoms. In uncompensated reflux or obstruction, pressure is transmitted to the distal reservoir. In compensated reflux or obstruction, pressure is decompressed via the collaterals.
Endovenous Interventions and Surgery
What are the new venous devices for great saphenous vein ablation?
Unlike laser and radiofrequency ablation (RFA), which uses thermal energy to close veins from the inside, the mechanochemical endovenous ablation (MOCA), otherwise known as ClariVein® in the US, uses a blunt-ended, rotating fiber that gently, but rapidly, spins inside the veins, agitating the lining, while a chemical used to normally treat veins is then injected to assist in the closure of the abnormal vein. Laser and RFA are limited in that they require numbing around the vein to protect the tissue from being injured by the heat. The numbing is effective, but laser and RFA cannot be used in the lower calf due to potential nerve injury. As ClariVein® works strictly inside the vein, there is no risk of nerve injury. It is safe and no anesthesia is necessary. Endovenous cyanoacrylate closure (VeClose®) is a new therapy approved by the US Food and Drug Administration for the treatment of clinically symptomatic venous reflux in the saphenous veins. In a randomized controlled trial comparing cyanoacrylate ablation closure vs RFA for incompetent great saphenous veins, treatment with both cyanoacrylate and RFA resulted in high occlusion rates at the 24-month follow-up visit. Quality of life scores improved equally with both therapies.
Biolas VariClose® is an embolization polymer (n-butyl cyanoacrylate based) indicated for ablation by polymerization for the endovenous treatment of incompetent lower extremity varicose veins. VariClose® offers advantages, such as ease of use, shortening of the procedure time, can be performed in outpatient conditions, eliminates the necessity of tumescent anesthesia in thermal ablation, and prevents complications in thermal ablation (eg, nerve damage, hematoma, rush, burn, etc). The 1-year results of a prospective comparative study (n=310 patients) and comparing the new cyanoacrylate glue vs endovenous laser ablation for the treatment of venous insufficiency (Bozkurt AK, Yilmaz MF. Phlebology. 2016;31(suppl 1):106-113) showed that cyanoacrylate ablation is a safe, simple method that can be recommended as an effective endovenous ablation technique.
Varithena® (FDA approved) is a patented device that produces cohesive, low nitrogen microfoam. It is an O2:CO2 (65:35) gas mixture with <0.8% nitrogen, and its small bubbles (median diameter <100 μm; all ≤500 μm) are rapidly absorbed. A randomized, placebo-controlled, multicenter study was conducted to evaluate the safety and efficacy of polidocanol endovenous microfoam (Varithena®). Patients (n=77) with symptomatic, visible varicose veins were randomized to treatment with either Varithena 1% or placebo. Varithena provided significantly greater relief from symptoms and improvement in leg appearance compared with placebo. Adverse events were generally mild and transient. The newest procedure, the Amsel Occluder Device (FDA premarket 510k), is intended for use in open general surgery procedures on tubular structures or vessels wherever a metal ligating clip is indicated and within the size range of 2.0 mm to 7.0 mm diameter.
Evidence for nonthermal, nontumescent ablation techniques
Ultrasound-guided foam sclerotherapy is indicated for the superficial venous system and acts as an adjunctive treatment following endovenous thermal ablation or surgical excision. It is performed by a long-indwelling catheter. Varithena® is an endovenous manufactured foam ablation system. The indications for a mechanochemical endovenous ablation (MOCA) procedure are the same as any endovenous ablation device, but with no nerve injury and heat complications. It can also be applied in a retrograde fashion down to the malleolus. Large veins and synechia are contraindications. Cyanoacrylate adhesive is applied using a proprietary catheter engineered to be inert to adhesive and a dispenser gun designed to deliver a precise amount of adhesive. Polyglycolic acid implant is an implantable system that still needs to be modified. Polytetrafluoroethylene (PTFE)-covered nitinol venous implant and Medusa coils are other systems in this class. Holmium laser shrinkage (low power setting without the need for anesthesia) is designed to produce collagen crosslinking to reestablish vein competency; it is used with foam following laser shrinkage. Comparison of MOCA vs RFA revealed significantly lower pain scores in the MOCA group without significant anatomic success and a lower venous clinical severity and Aberdeen varicose vein questionnaire score. Comparison of cyanoacrylate adhesive vs endovenous laser ablation revealed significantly shorter procedural time and less pain in the cyanoacrylate adhesive group with no differences in the occlusion rates.
Randomized controlled trial comparing mechanochemical ablation to radiofrequency ablation: the multicenter Venefit vs ClariveinR for varicose veins (VVCVV) trial – longterm follow-up
This trial included 170 patients, where 87 were randomized to the mechanochemical endovenous ablation group. The primary outcome was procedural pain, while the secondary outcome was improvement in clinical and quality of life scores. Maximum pain was significantly less in mechanochemical endovenous ablation compared with RFA. Similar improvements were achieved in clinical and quality of life scores in both groups at 2 years with similar occlusion rates.
Randomized controlled trial of cyanoacrylate (VenaSeal) vs radiofrequency ablation: 36-month results
The primary end point of the study was complete closure of the target vein at 3 months, and the secondary end point was ecchymosis at day 3 using a point grading scale. Assessments related to venous disease severity and quality of life (QOL) were performed, and a comparison of adverse event rates related to the target great saphenous vein was made. The venous clinical severity score (VCSS) demonstrated a statistically significant improvement out to 6 months, which was sustained through 12, 24, and 36 months in the Venaseal group; subjects also experienced a statistically significant improvement from baseline and improvement over time through 36 months. The majority of adverse events reported in 12 to 24 months were unrelated to the treatment or the device across all groups. Among the Venaseal adverse events from 0 to 36 months, there were no reports of deep vein thrombosis, no allergic events, and no unanticipated adverse events. The Venaseal procedure resulted in a reported 94.4% closure rate, demonstrating continued, noninferiority compared with radiofrequency ablation (P=0.005) through 36 months. The VCSS, Aberdeen varicose vein questionnaire (AVVQ), and EQ-5D outcomes demonstrated a statistically significant improvement from baseline with sustained results over time and no difference between treatment groups out to 36 months. The roll-in phase analysis of a clinical study of cyanoacrylate closure for an incompetent great saphenous vein revealed a 3-month closure rate up to 100%, with similar postprocedural pain. The WAVES clinical trial (Lake Washington Vascular VenaSeal Post-Market Evaluation) also revealed similar beneficial results. The CAPE study (Cyanoacrylate closure for incompetent perforating veins) revealed a 76% occlusion rate at 3 months, with no deep vein thrombosis.
The Swiss Registry of Thermic Endovenous Catheter Therapy (SWISS TECT Registry) in varicose veins. A multicenter case study
In 2005, endovenous treatment in Switzerland was not covered by insurance due to a lack of security and monitoring data, which sparked the creation of a central registry. The main criteria were security monitored as deep vein thrombosis (endovenous heat-induced thrombus and legs) and/or pulmonary embolism within 4 weeks after the intervention. Efficacy was monitored as failure (no occlusion at 1 week) and recurrence (partial or no occlusion) after 4 weeks. All doctors of the Swiss Society of Phlebology were invited to participate in the study. In this registry, failure at 1 month was 3.3%, recurrence at 1 year was 3.6%, and thrombosis at 1 week was 0.86%.
Randomized controlled trial of compression therapy following endothermal ablation
A randomized study was conducted to evaluate the effect of wearing compression stockings after varicose vein treatment. Patients with saphenous vein incompetence presenting for endothermal truncal ablation were randomized to receive either 1 week of compression stockings (group A) or no stockings (group B). The pain scores, compliance, clinical scores, and quality of life scores at 2 weeks and 6 months were assessed. This summary focuses on the interim results at 2 weeks. Of the 110 patients randomized, 49.3% received compression stockings. The follow-up rate at 2 weeks was 66%. The clinical scores and quality of life scores improved in both groups. The mean improvement in the Venous Clinical Severity Score was -1.6±2.5 in the group with compression compared with -1.9±2.2 in the group without compression (P=0.542). While these interim results show no significant difference between the two groups, it appears that the extent of quality of life improvement observed in the group without compression is smaller than in those receiving compression stockings, indicating that wearing compression stockings after endothermal ablation may be advantageous following treatment. This study is currently active and still recruiting patients.
A single-center, randomized controlled trial comparing radiofrequency ablation and mechanochemical endovenous ablation of varicose veins in patients with bilateral involvement: initial experience
Mechanochemical endovenous ablation (MOCA) and glue injections allow entire trunks to be treated with single anesthetic injections. Previous nonrandomized work has shown that postoperative pain is reduced with these techniques. However, the difference in pain perception from the same technique can vary considerably between patients, as younger patients and patients with higher economic strata have more pain. In this study, patients with bilateral varicose veins underwent both MOCA and radiofrequency ablation under local anesthesia. Pain scores were determined using a visual analog scale. Patients (n=20) were followed-up at 1 and 6 months postprocedure, and the clinical scores, quality of life scores, and duplex ultrasounds were acquired. Patients in the MOCA group experienced less pain during the procedure. Postoperative pain scores were similar in both groups. Occlusion rates, clinical severity scores, disease-specific and generic quality of life scores were similar between groups at 1 and 6 months. The duration of the procedure was significantly less in the MOCA group.
Cryostripping as an alternative to endovascular approaches in the treatment of varicose veins
The cryostripping technique represents the modern alternative to saphenectomy through a stripping procedure. It is done by using a special freezing probe that is inserted in a retrograde manner in the saphena magna or parva vein after performing the crossectomy. By freezing the vein with nitrogen (-85 C), the vein adheres to the probe and it can then be extracted. The results show that this procedure results in minimum tissue trauma, which helps patients with phlebolymphedema of the lower limbs avoid the postoperative cutaneous paresthesia by intercepting the saphenous nerve. From an economical point of view, this method is cost-effective because the probes can be resterilized. The patient can undergo this procedure under surgical ambulatory conditions, meaning that there is a faster return to normal activies.
Varicose vein worldwide trends in public digital interest
Technological advancements, growth in health care expenditures, and population factors increase the incidence of venous disease, which is driving the market for varicose vein procedures. The Internet has become a source of health care information used by patients and physicians to research symptoms, diagnoses, and treatments. Google is the most popular search engine for online health-related information. All of these factors urged the authors to conduct this study to evaluate the worldwide trends in patient varicose vein research and treatment, using Google search behavior as a proxy. Data from the Google trends on the worldwide topic of varicose veins over the last 10 years was analyzed to identify changes in population search activity and thus interest in varicose veins symptoms, recurrence, and treatment. Subanalysis by region was also performed. Interest in varicose veins worldwide steadily increased by >35%. Commonly associated search terms were surgery (75%), pregnancy (80%), pain (60%), alternative and nonoperative treatments (10% to 20%), and laser (40%). An interest spike occurred in May 2008, coinciding with an increase in the publication of medical literature on varicose veins. Search behavior exhibited a regular, cyclic pattern that was seasonal – higher in summer months, lower in winter. The most rapid increase has been in non–English searches for varicose veins.
Comparison between foam sclerosis, radiofrequency, and laser in the treatment of large varicose veins in Mexico
The authors made a comparison between different treatment modalities for varicose veins in Mexico. They followed the patients for 18 months postprocedure. A clinical, etiological, anatomical, pathophysiological (CEAP) classification was made for each patient. The patients were evaluated for total closure of the saphenofemoral junction, changes in the quality of life scale, postoperative pain score at day 3 postprocedure, associated morbidities, and cost of the procedures. They concluded that new minimally invasive procedures end up with less morbidity and at least the same rates of closure as the older techniques.
A comparison of adjunctive tributary laser ablation and foam sclerotherapy in patients undergoing truncal endovenous laser ablation for lower limb varicose veins
This study compared outcomes of patients receiving simultaneous endovenous laser ablation (EVLA) or foam sclerotherapy (foam sclerotherapy) of tributaries and EVLA of the great saphenous vein (GSV) trunk. Complications, Aberdeen varicose vein questionnaire (AVVQ), EuroQOL 5-dimension (EQ-5D), numerical rating scale, and condition of residual varicosities were assessed at 3 days, 4 weeks, and 6 months after the procedure. All residual varicosities were identified and eliminated with a staged foam sclerotherapy at 6 months. Except for ecchymosis, the incidence of other complications was not significantly different between the groups at 6 months. The pain numerical rating score in the EVLA/foam sclerotherapy group was remarkably elevated at 4 weeks, and then declined to a level comparable with EVLA alone group at 6 months. EVLA/foam sclerotherapy group exhibited a significant improvement in both AVVQ and EQ-5D scales vs the EVLA group at 6 months, but there was a poor improvement at 4 weeks. EVLA/foam sclerotherapy group had a significantly lower rate of residual varicosities than the EVLA group, thus reducing the need for the staged foam sclerotherapy.
Deep Vein Reconstruction
Deep vein reconstruction
When a direct valve repair is possible, valvuloplasty is the best option, but when it is not feasible, the following techniques can be used: transposition of the femoral vein onto the great saphenous vein or onto the deep femoral vein as long as their terminal valve is competent, vein transplant (usually axillary vein transfer), neovalve, and nonautologous artificial venous valve. Valvuloplasty is also possible without a phlebotomy by narrowing the lumen with some stitches at the cusp insertion angle, termed transmural valvuloplasty. Restoring valve competence without opening the vein is also the purpose of external banding (or prosthetic sleeve or external cuffing). If the ipsilateral deep femoral or great saphenous veins have a proximal competent valve and adequate caliber, transfer of a femoral vein distal to the competent valve can be performed. The vein transplant principle consists of inserting a segment of a competent valvulated vein in an incompetent deep venous network. The donor segment can be the axillary vein or brachial vein. The neovalve principle is to construct an autologous valve by using the patient’s venous tissue. Outcomes are different in primary deep venous insufficiency when the valve is restorable compared with outcomes in postthrombotic syndrome, where the valves are usually destroyed. It is sometimes difficult to evaluate the results of deep venous reconstructive surgery for reflux because the outcomes are generally based on a decrease in pain, an absence of ulcer recurrence, and restored valve competence. Correcting the deep venous reflux is the corner stone of the treatment for venous ulcers as long as the deep venous obstruction and superficial reflux are corrected first. Healing of a venous ulcer can be achieved with very good results in both primary and secondary deep venous pathology with these techniques.
Deep vein reconstruction: an update – what’s new in 2018?
The principle of the neovalve is to construct an autologous valve by using the patient’s venous tissue. In the technique by Plagnol et al, the neovalve is created with the great saphenous vein termination, opportunely sectioned, shaped, and invaginated into the femoral vein to function as a valve. In Maleti’s technique, the neovalve is obtained by dissecting the vein wall to obtain a flap that will work as a valve after adequate fixation. The wall dissection is possible due to the thickened vein wall. In the event of valve agenesis, the entire wall can be utilized, restoring the vein continuity using bovine pericardium. The postthrombotic lesions frequently create an intraluminal fibrotic septum that facilitates the neovalve elaboration. The technique for constructing a neovalve is not always the same; it depends on the anatomical condition of the wall and, therefore, the most suitable option is determined only after a phlebotomy. Generally, in the presence of a double channel, the first option is a neovalve using the intraluminal septum; when the vein wall is thickened, a neovalve is created according to the usual manner of dissecting the vein wall. If none of these conditions are found, the vein wall is invaginated to create a flap featuring a valve and the vein itself is reconstructed with bovine pericardium or polytetrafluoroethylene. The flap is maintained in position using stitches that are fixed at both corners of the flap. This method is applied using bovine pericardium to reconstruct the wall in a few cases when it was impossible to create a neovalve using the classic technique.
Varicose vein surgery in deep vein aplasia and hypoplasia cases
Possible devascularization procedures are classic surgical or new endovascular interventions. In some cases of venous truncular defects, removal of varicose veins even in the case of a hypoplastic deep venous system is possible. In other cases, a systematic management should be advised to reroute the venous flow from the superficial enlarged vessels to the deep veins. In 12 patients, hypoplasia, aplasia, or stenosis was present in the deep axial veins, but no signs of obvious arteriovenous shunts were found. These patients were selected for surgery using a new modification to the Perthes test. Instead of a rubber strip tourniquet, a tensiometer cuff was placed on the limb just below or just above the knee. The cuff was inflated to 110 mm Hg and the patients were asked to walk quickly for 5 minutes. In positive cases, when deep veins were absent and superficial veins were compressed by the cuff, the limb became livid and the patient complained of strong pain within 1 or 2 minutes. In negative cases, when collateral channels in the subfascial space were sufficient in number and diameter to drain the venous blood from the leg, patients informed the authors that their legs felt better. In these cases, the dilated pathologic superficial veins were removed without any circulatory complications.
Deep venous valve reconstruction: femoral transposition and neovalve
The indications for the deep venous surgery in this series were the patients who had deep venous insufficiency and persistent active ulcers even after compression treatment, suppression of superficial reflux and perforator insufficiency, and endovascular iliac vein stenting. From July 2013 to April 2017, deep venous surgery was performed on 14 patients (5 femoral transpositions and 10 neovalves) in this series. The femoral vein transposition was performed if the ipsilateral great saphenous vein has a proximal competent valve and adequate caliber. The neovalve procedure was carried out if the superficial reflux and perforator insufficiency had been suppressed previously. Although the numbers were too small to analyze the outcomes, this study demonstrates both the feasibility and effectiveness of reconstructive deep venous surgery for recalcitrant venous ulcers.
Surgical treatment of severe deep venous valve dysfunction in the lower extremities
Surgery for deep venous reflux in the lower has had, for various reasons, a more limited development vs arterial surgery, including endovascular techniques. The importance and frequency of deep venous reflux in chronic venous disease and particularly in chronic venous insufficiency (CVI) has been identified only in the last 20 years, due to the development of duplex ultrasound scanning. Despite its effectiveness, deep reconstructive surgery remains controversial; this may explain why this specific surgery is performed by few units worldwide. Furthermore, as deep reconstructive surgery is usually combined with superficial and perforator vein surgery, assessment of its specific benefit is difficult. In patients with severe CVI, venous valvular reflux involves deep veins as an isolated abnormality in less than 10% of cases, but it is associated with superficial reflux and/or perforator incompetence in 46% of cases. The most common etiology in deep venous reflux is postthrombotic syndrome, which accounts for an estimated 60% to 85% of patients with CVI. Primary reflux is the result of structural abnormalities in the vein wall and the valve itself. A very rare cause of reflux is the absence of valves secondary to agenesis. Surgical techniques for treating deep venous reflux can be classified into two groups: those that do and those that do not involve a phlebotomy. Techniques for the first group include internal valvuloplasty, transposition, transplantation, neovalve, and cryopreserved allograft, and the techniques for the second group involve wrapping, Psathakis II procedure, external valvuloplasty (transmural and transcommissural) assisted or not by angioscopy, external valve construction, and percutaneously placed devices. Some clinical features help distinguish superficial venous insufficiency from deep venous insufficiency, but they are not reliable enough because both conditions are frequently present. In addition, primary reflux is difficult to identify from secondary deep reflux.
Clinical result of surgery for retroperitoneal leiomyosarcoma with involvement of the inferior vena cava
Leiomyosarcomas of the inferior vena cava represent a rare form of soft tissue sarcomas. Limited data are available regarding the surgical management of the inferior vena cava and long-term survival. The aim was to review the authors’ institutional series of inferior vena cava resections and reconstructions for retroperitoneal leiomyosarcoma, focusing on the type of vascular replacement, morbidity, mortality, and long-term outcomes. From 2005 to 2015, 96 patients with retroperitoneal leiomyosarcoma involving the inferior vena cava who underwent surgery were collected. The results confirmed that resection of retroperitoneal leiomyosarcoma combined with reconstruction of the inferior vena cava can be performed with very low morbidity and mortality even when extensive repairs are necessary. Routine replacement of the inferior vena cava with a prosthetic graft can avoid venous complications of the extremities and likely contributes to the quality of survival. Survival depends on the tumor grade and the completeness of the resection. Patient survival will improve with experience and expertise.
Vena Cava Filters
An update on inferior vena cava filters: what is new?
Since 2005, the Food and Drug Administration (FDA) received >1000 reports of inferior vena cava filter complications from several brands. Subsequently, the FDA recommended that physicians and clinicians who implanted the inferior vena cava filters and who are responsible for the ongoing care of these patients should consider removing the filter as soon as protection from pulmonary embolism is no longer needed. Between 2005 and 2010, there was a 22% increase in inferior vena cava filter placements in the US, but, between 2010 and 2014, there was a 29% decrease. The implantation rate in the US was 25 times higher than in Europe. In a randomized controlled trial on the effects of a retrievable inferior vena cava filter + anticoagulation vs anticoagulation alone on the risk of a recurrent pulmonary embolism, the results were similar at 6 months in both groups. The current recommendation is that filters should not be used in patients receiving anticoagulation (grade 1B) and filters should be used if the patients cannot receive anticoagulation (grade 1B). Lyon presented the filter retrievability algorithm, absorbable inferior vena cava filters, and filters with a thrombolysis protection system used in a study on absorbable inferior vena cava filters (Radiology. 2017;285[3]:820-829). Leon summarized that the trend of inferior vena cava filter placement in the US is still much greater than in the rest of the world, despite a trend for a decrease after the FDA warning. New designs are being developed to overcome the morbidity associated with not retrieving inferior vena cava filters.
Technical safety, feasibility, and accuracy of ultrasound-guided bedside placement of inferior vena cava filters
This study was conducted to report the feasibility and safety of inferior vena cava filter placement under ultrasound-guided bedside placement. The medical records of all 2856 patients who had inferior vena cava filters placed under ultrasound guidance between 2007 and 2016 were retrospectively reviewed for pertinent history, results, and complications. All filters were placed using an ultrasound-guided filter deployment technique. Venous access was via the right femoral vein, left femoral vein, or right internal jugular vein. Filters were successfully placed within the inferior vena cava in 99.7% of the patients. Complications included groin hematoma (0.07%), deep venous thrombosis at the site of vascular access (0.31%), and filter tilt >15° along the long axis of the inferior vena cava (0.03%). The bedside ultrasound-guided inferior vena cava filter placement is technically feasible and safe with improved placement accuracy and it is cost-effective compared with filter deployment under fluoroscopic venogram imaging.
How to deal with thrombus of vena cava filter?
Inferior vena cava filter thrombosis is a complex problem. A thrombus within an inferior vena cava filter may range from an asymptomatic small thrombus to a critical inferior vena cava occlusion that affects both lower extremities. Even with the paucity of published data, endovascular treatment methods appear to be safe and effective in patients with filter-related inferior vena cava thrombosis, with results comparable to those reported for catheter-directed iliofemoral deep vein thrombosis therapy. The pulse-spray technique was commonly used at several institutions, eventually evolving into combined techniques used in conjunction with mechanical thrombectomy devices. Although pulse-spray and/or mechanical devices may be successful in isolation in select patients, large thrombus burdens in the inferior vena cava typically require catheter-directed thrombolytic infusion that may last 24 to 72 hours. In theory, due to a large thrombus burden and the potential involvement of bilateral iliofemoral veins, patients with an inferior vena cava thrombosis often require higher thrombolytic doses than patients who have an isolated deep vein thrombosis in an extremity. Furthermore, the indwelling inferior vena cava filter creates an obstruction to establishing venous outflow, producing further potential difficulties for the endovascular procedure.
Thromboembolic Diseases
Chronic venous thrombosis… Is there such a thing?
Labroupolus compared the ultrasound features of acute thrombosis and the chronic changes that occur after a thrombosis. In acute thrombosis, the vein is dilated and noncompressible, there are filling defects on color-flow duplex examination, absence of a signal, smooth borders, and a homogenous texture, and it is echolucent. In chronic cases, the vein has a decreased diameter, wall thickening, rough borders, and heterogeneous texture and it is echogenic, with intraluminal webs and reflux. The speaker explained how we could diagnose recurrent deep vein thrombosis: if the thrombus is in a new location – this could be a different vein segment, different extremity, or propagation to a new level. If the thrombus is in a previously affected segment, thrombus thickness increases >4 mm in proximal veins and >2 mm in calf veins. Labropoulos pointed out that the problem is that many patients receive anticoagulation therapy and sometimes thrombolysis for a diagnosis of “chronic deep vein thrombosis,” which can result in significant costs and put the patients at risk for bleeding. The histological and functional description of the tissue causing chronic postthrombotic venous obstruction showed abundant and loose collagen, neovascular channels, recanalization channels, and inflammation. Postthrombotic changes also included wall remodeling with vein wall thickness. In the speaker’s opinion, the term chronic deep vein thrombosis is erroneous and can be dangerous; therefore, a new term is needed, such as chronic postthrombotic luminal changes, chronic venous fibrosis, or another option.
Time to bury the term “chronic venous thrombosis”
Parsi argued that, while we are all familiar with deep vein thrombosis and its biochemical nature, there are two other entities that must be defined/refined–sclerosis of deep veins after sclerotherapy and chronic venous thrombosis. The speaker discussed results from his research showing that high concentrations of sclerosants reduced platelet lysis, reduced levels of fibrinogen, and reduced clotting factors to inhibit clot formation. In contrast, low concentrations of sclerosants increased platelet activation, which induced clot formation. A sclerosant-induced thrombus is denser and more stable, with a tendency for sclerosis and fibrosis. Parsi suggested the term sclerothrombus could be used for a sclerosant-induced thrombus and the term sclerocoagulum could be used for trapped blood. Then the speaker asked the question “Is there such a thing as chronic venous thrombosis? Histology shows endovascular fibrosis and ultrasound echogenic occlusion and noncompressibility; therefore, Parsi suggested the term chronic venous fibrosis.
The natural history of deep vein thrombosis
Meissner explained that deep vein thrombosis is a multicausal disease and the risk factors are synergistic, not additive. The risk factors can be congenital, acquired, situational, or a combination. The mean recanalization percent after deep vein thrombosis was 52% after 6 months and 59% after 12 months. The determinants of recanalization were sex (females [66%] vs males [55%]), location (calf vein thrombosis [71%] vs proximal thrombosis [52%]), initial thrombus score, and a risk score. Next, the speaker presented a study that included 1626 patients with venous thromboembolism in which the predictors of recurrent venous thromboembolism were unprovoked venous thromboembolism, thrombophilia, deep vein thrombosis, pulmonary embolism, shorter anticoagulation, and age. The conclusion was that deep vein thrombosis is a chronic coagulation disease. In another trial, the risk of postthrombotic syndrome was associated with ipsilateral recurrent deep vein thrombosis, popliteal thrombosis, occlusive thrombosis, and the extent of the thrombosis, demonstrating again that deep vein thrombosis is a chronic coagulation disease. Meissner emphasized that an early natural history is a dynamic balance between recanalization and recurrent thrombotic events. Late natural history dominated by recurrent venous thromboembolism is determined by underlying thrombotic risk factors, the extent of recanalization, and the degree of activated coagulation. The long-term outcomes related to natural history depend on rapid recanalization, which protects valve function, and recurrent deep vein thrombosis, which predicts reflux and postthrombotic syndrome.
Novel ways to target venous thrombosis
Mechanisms of deep vein thrombosis are not completely understood. Platelets play a role in deep vein thrombosis, but the impact on specific platelet receptors remains unclear. Platelet C–type lectin-like receptor 2 (CLEC-2) is known to maintainthe physiological state of blood vasculature under inflammatory conditions. Deep vein thrombosis is a thromboinflammatory disorder, developing largely as sterile inflammation in the vessel wall. Recently, Watson’s team hypothesized that CLEC-2 might play a role in deep vein thrombosis. Using a murine deep vein thrombosis model of inferior vena cava stenosis, they demonstrated that mice with a general inducible deletion of CLEC-2 or a platelet-specific deficiency in CLEC-2 are protected against deep vein thrombosis. No phenotype in the complete stasis model was observed. Transfusion of wild-type platelets into platelet-specific CLEC-2 knockout mice restored thrombosis. Deficiency in CLEC-2, as well as the inhibition of podoplanin, a ligand of CLEC-2, was associated with reduced platelet accumulation on the inferior vena cava wall 6 hours after the stenosis. Podoplanin was expressed in the inferior vena cava wall, where it was localized near the abluminal side of the endothelium. The extent of podoplanin increase in the inferior vena cava 48 hours was higher in mice with a thrombus vs those without a thrombus. Treating the animals with an antipodoplanin neutralizing antibody resulted in the development of smaller thrombi. Thus, they propose a novel mechanism for deep vein thrombosis, whereby CLEC-2 and upregulation of podoplanin expression in the venous wall trigger thrombus formation.
Venous thromboembolism epidemiology and patient’s data base in China
The morbidity of venous thromboembolism is increasing; therefore, it is important to set up a database with data on the epidemiology and the diagnosis and treatment information of Chinese patients with a venous thromboembolism. By August 31, 2017, 10 520 patients from 76 hospitals had been registered (males, 49.3%; average age, 58 years). The most important risk factors were surgery and immobilization, injury, bone fracture, hypertension, and tumors. In China, venous thromboembolism is more common in females than males, where swelling is the most common symptom and increased muscular tension is the second most common symptom. Ultrasound was the most commonly used diagnostic method, accounting for 93.9% of all cases. Most cases (87.5%) were diagnosed within 3 months after symptom onset. Surgical and nonsurgical methods were used to treat 35.7% and 64.3% of the patients, respectively. Surgical therapy included thrombectomy, thrombolysis, and filter implantation, and nonsurgical therapy included anticoagulation, vasoactive drugs, compression. In the efficacy evaluation, no statistically significant difference in tension/range of motion was observed between surgical and nonsurgical methods. The probability of a perimeter difference <1.0 cm in the affected limb after nonsurgical treatment was greater than after surgical treatment. The probability of the contrast/ vascular ultrasound showing the highest degree of recovery was greater after surgical treatment than after nonsurgical treatment.
Cancer-associated thrombosis: an Asian perspective
Of all cases of venous thromboembolism (VTE), about 20% occur in patients with cancer, with an annual incidence around 1 in 250, and cancer leading to a 4- to 6-fold increased risk of a VTE. Of all patients with cancer, 15% will have a symptomatic VTE, but as many as 50% have a VTE at autopsy. The risk is the highest in the first few months after diagnosis of cancer and in the presence of distant metastases. VTEs are more common with certain types of cancer; the top 5 most common sites include the lung, prostate, colorectal, urological, and lymphomas. In 105 consecutive adult Thai patients with an objectively confirmed history of VTE, where a complete clinical summary was obtained, 19% had a malignancy and the site of the primary cancer was gynecological (38%), lung (16%), lymphoma (6%), gastrointestinal (10%), and breast (5%).
The guideline recommendations for treating cancer-associated thrombosis include low-molecular-weight heparin (LMWH) or unfractionated heparin (UFH) as an initial treatment (5 to 10 days) and LMWH as an extended treatment (3 to 6 months). A retrospective analysis of a US medical database showed that the limitations of LMWH and vitamin K antagonist treatment result in poor adherence to guideline recommended therapies for cancer-associated thrombosis. A simplified, oral anticoagulant treatment will overcome the limitations of the standard of care and improve both treatment adherence and quality of life. The efficacy and safety profiles of direct oral anticoagulants are similar to warfarin in patients with cancer and an acute VTE. Head-to-head data on direct oral anticoagulants vs LMWH in patients with cancer is required.
The latest evidence from the SELECT-D pilot phase 3 trial (anticoagulation therapy in SELECTeD cancer patients at risk of recurrence of venous thromboembolism), which compared rivaroxaban to dalteparin, demonstrated lower recurrent VTE events, low major bleeding events in both groups, which were numerically higher with rivaroxaban, and more clinically relevant nonmajor bleeds with rivaroxaban. In the Hokusai VTE-cancer study, oral edoxaban was noninferior to dalteparin for the composite primary end point of recurrent VTE and major bleeding. The rates of severe major bleeding and the survival rates free of recurrent VTE or major bleeding were similar. There is no clinical trial evidence on the optimal duration of anticoagulation in cancer-associated thrombosis.
The consensus recommends continuing anticoagulation as long as the cancer is active, to continue if chemotherapy is ongoing, and to discontinue if the risk of serious bleeding outweighs the risk of a recurrent VTE. Reported risk factors for bleeding in patients with cancer-associated thrombosis are age >75, recent major bleeding, renal or liver impairment, severe thrombocytopenia, metastatic or advanced cancer, intracranial lesion, and selected tumor types (eg, colorectal, bladder). Cancer associated thrombosis is common, and the guidelines support the use of LMWH. Direct oral anticoagulants were recently shown to be at least equivalent to LMWH. The risk of VTE recurrence and bleeding should be assessed when deciding on anticoagulation therapy.
Incidence of venous thromboembolism in Asia
Previously, venous thrombosis was perceived as rare in Asia; however, 40 to 50 years later, incidences of deep vein thrombosis have been increasing in hospitals. The main risk factors identified were malignancies, immobilization, surgery, and old age. In a systematic review on the incidence of venous thromboembolism in Asian populations, nine studies of Asian hospital registries or databases were analyzed, showing an increasing population incidence of venous thromboembolism in South Korea and China. The earlier low incidence rates could be explained by low incidence awareness, underdiagnosis, and the near absence of factor V Leiden and prothrombin gene mutations. The rising trend could be due to an aging population, increasing number of patients with cancer, increasing surgical procedures, increasing clinician awareness, and lower threshold for diagnostic tests. In conclusion, Heng emphasized that available data should not be directly extrapolated to places with different health care systems and less extensive databases. Recommendations for anticoagulant prophylaxis on international guidelines derived from Western data for Western populations may not be the same in Asia. The speaker stressed that advice on anticoagulation and prophylaxis in Asia should be based on local data and evidence.
The risk of bleeding with direct oral anticoagulants in East Asia
East Asians have a lower body weight and kidney function than Caucasians with an approximate 20 kg lower body weight. Kidney function is correlated with body weight. East Asians also have a relatively low incidence of myocardial infarction; in contrast, East Asians have a relatively high incidence of cerebrovascular accidents compared with Caucasians and a markedly higher incidence of intracranial hemorrhage compared with Westerners. East Asians have lower warfarin time in the therapeutic range. There were many Asian countries participating in international trials on direct oral anticoagulants. In the ENGAGE AF study, East Asians had higher stroke or systemic embolic events during the treatment period. The causes of the higher rate of intracranial bleeding in Asians are not clearly understood. Some antithrombotic drugs show differences in the risk of major hemorrhage and intracranial hemorrhage. Dabigatran is expected to be of particular benefit to Asians, and the same could be valid for rivaroxaban, apixaban, and edoxaban. Generally, the incidence of intracranial bleeding with direct oral anticoagulation is lower vs warfarin. In guidelines prepared by the Japanese Circulation Society, dabigatran and apixaban are recommended, and rivaroxaban and edoxaban are in the “use may be considered” category. Asian physicians keep the prothrombin time to international normalized ratio (PT-INR) lower than in Western countries. A great risk of intracranial hemorrhage is anticipated when warfarin is used for Asian patients. When compared with warfarin, direct oral anticoagulants reduced the incidence of intracranial bleeding. The use of direct oral anticoagulants seems to be a good option for stroke prevention when Asian patients with nonvalvular atrial fibrillation are treated. East Asian patients are more likely to have body weight <60 kg and a creatinine clearance of 30 to 50 mL/min. A dose reduction of direct oral anticoagulants should be considered in Asian patients. FXI and XII are targets for new anticoagulants.
Iliocaval obstruction stenting – results of 100 consecutive limbs
In 100 consecutive cases of iliocaval obstruction treated with surgical intervention collected over the last 5 years, the obstructions were thrombotic and nonthrombotic as well as chronic, acute, and subacute. The most frequently performed interventions were endovascular repair by angioplasty and stenting, femoral vein endophlebectomy with or without an arteriovenous fistula, and thrombolysis of acute and subacute deep vein thrombosis affecting iliofemoral veins or the inferior vena cava. Data were collected on the overall stent patency rates, failure rates, complications, and the revascularization effect on the symptoms. The results showed that iliac-caval venous stenting is a satisfactory clinical option for patients with severe manifestations who need a fast relief from their symptoms.
Use of superior vena cava filters in the management of upper limb venous thrombosis
While the incidence of upper limb deep vein thrombosis is uncommon, it will undoubtedly increase as the use of central venous access devices become more common. Even though no gold-standard treatment exists, multiple treatment strategies are available that are similar to established strategies for lower limb deep vein thrombosis. Indications for superior vena cava filter placement are failure or contraindication to therapeutic anticoagulation or for presurgical prophylaxis in the setting of substantial thromboembolic risk factors. The placement of superior vena cava filters remains controversial because there has not been a well-documented study with routine imaging and surveillance of patients with pulmonary embolism and upper limb deep vein thrombosis that excludes the lower extremity as the source of the presenting pulmonary embolism. When possible, the procedure should be performed from a common femoral vein approach. Similar to inferior vena cava filter placement, superior vena cava filter placement should begin with superior vena cavograms to exclude underlying venous stenosis and to document superior vena cava patency. Theoretically, though yet unproven, it is believed that patients with some degree of superior vena cava stenosis on venogram are at a decreased risk for pulmonary embolism because the stenosis could potentially halt the progress of a large embolism through the stenotic vessel lumen. However, any vascular stenosis can impede blood return and eventually be the cause of thrombus formation. Ideal filter placement has been described with the filter hooks within the superior vena cava at the confluence of the right and left brachiocephalic veins with the apex of the filter directed toward the right atrium. Placement in this location helps prevent associated thromboembolic complications in the azygous vein. The two superior vena cava filters that have been extensively studied are the Greenfield filterTM; (Boston Scientific, Watertown, MA) and the TrapEase® filter (Cordis, Miami Lakes, FL). Due to the large numbers of each of these filters used when compared with a very limited number of other filter types studied in the superior vena cava, it is difficult to determine the superiority of one filter over another. Complications of superior vena cava filter placement are rare, but potentially more severe compared with inferior vena cava filter placement. These complications include superior vena cava perforation, cardiac tamponade, aortic perforation, superior vena cava thrombosis, and pneumothorax. In the case of strut perforation, there is little to no structure in the mediastinum equivalent to the retroperitoneal cavity to provide any form of barrier to protect the surrounding organs. Whereas strut perforation in the inferior vena cava occurs often without consequence, perforation through the wall of the superior vena cava may result in injury to the lung, aorta, pulmonary artery, heart, or pericardium. Filter migration is also a concern, given the close proximity to the heart.
Associations between inferior vena cava thrombosis and pulmonary embolism risk in symptomatic venous thromboembolism: a prospective and observational cohort study
This prospective and observational cohort study evaluated the prevalence, clinical significance, and risk of pulmonary embolism of inferior vena cava thrombosis in patients with a venous thromboembolism. A total of 846 patients hospitalized for symptomatic venous thromboembolism in the author’s center were evaluated by inferior vena cava venography and pulmonary angiography. The clinical characteristics of the patients with a venous thromboembolism complicated with inferior vena cava thrombosis were analyzed. The patients were followed-up for 30 days for a short-term prognosis analysis. Pulmonary embolism was more common in patients with deep venous thrombosis and inferior vena cava thrombosis than in those without an inferior vena cava thrombosis. Multivariate logistic regression analysis showed that inferior vena cava thrombosis was an independent risk factor for pulmonary embolism. Trauma, immunological diseases, and previously diagnosed venous thromboembolism increased the risk for inferior vena cava thrombosis. No deaths occurred in patients with inferior vena cava thrombosis.
Correlation of various platelet indices in deep venous thrombosis
In this study, Kumar Khanna assessed a number of platelet parameters in 33 patients with deep vein thrombosis and in 33 controls. Patients taking antiplatelet drugs or anticoagulants were excluded. A Beckmann Coulter analyzer was used to study platelet indices. D-Dimer was also assessed. Total leukocyte count, red blood cell distribution width (RDW), mean platelet volume (MPV), platelet distribution width (PDW), and platelet larger cell ratio (P-LCR) results were high in patients with deep vein thrombosis vs controls. Correlation analysis revealed that MPV was directly related to P-LCR and inversely related to platelet count. Platelet count was directly related to plateletcrit (PCT) and platelet cell concentration (P-LCC). Comparison of all platelet indices between patients with deep vein thrombosis and controls showed that RDW, MPV, PDW, and P-LCR were significantly higher in patients with deep vein thrombosis (RDW: 57.8±15.2 fL vs 43.2±5.5 fL [P<0.001]; MPV: 9.9±1.2 fL vs 9.1}0.9 fL [P=0.004]; PDW: 16.5±0.7 fL vs 15.9±0.6 fL [P<0.001]; P-LCR: 40.9%±8.2% vs 34.2%±8.0% [P=0.001]). Receiver operating characteristic (ROC) analysis of MPV showed an area under the curve (AUC) of 0.664, P=0.022, a cut-off value of 9.25, sensitivity of 60%, and specificity of 58%. Comparison of all platelet indices with MPV <9.25 fL and MPV >9.25 fL showed that the platelet count was high in patients with an MPV <9.25 fL (309.6}79.1×10-3/μL vs 226.6±107.7×10-3/μL; P=0.023). All other indices showed a nonsignificant relation within both groups. In the authors’ opinion, the combination of various platelet indices with D-dimer analysis can increase the sensitivity of the diagnosis of deep vein thrombosis even in the absence of duplex ultrasound, and it can be used as a screening method to detect deep vein thrombosis.
H-NMR spectroscopy metabolic profiling of serum in the inferior vena cava ligation murine model may discriminate deep vein thrombosis age
Approximately 20% to 50% of patients with deep vein thrombosis will develop postthrombotic syndrome despite adequate anticoagulation therapy. The use of thrombolysis during acute deep vein thrombosis may reduce the long-term complications of postthrombotic syndrome; therefore, establishing thrombus age is critical. Currently the estimation of thrombus age is based on the patient’s description of time of symptom onset. Kafeza and her team aimed to identify metabolic markers of thrombus age in mice. The well-established inferior vena cava ligation mouse model was used to generate deep vein thrombosis and was compared with sham laparotomy controls. Serum was obtained from deep vein thrombosis and control mice at days 2 (acute deep vein thrombosis), 6, and 14 (chronic deep vein thrombosis). H-NMR spectroscopy untargeted metabolic profiling was performed. The data was subjected to multivariate and univariate statistical analysis. Twenty-four serum metabolites were identified. Lactate, choline, high-density lipoprotein, and low-density lipoprotein / very low-density lipoproteins were present at significantly different levels in the serum of mice with deep vein thrombosis compared with sham-controlled animals at day 2. These differences were not statistically significant at days 6 and 14, suggesting that metabolic changes in thrombus formation and maturation occur early in the deep vein thrombosis process. In conclusion, in the murine model, a metabolic disturbance was prominent in the early stages of deep vein thrombosis, which has important translational mechanistic and therapeutic applications for human deep vein thrombosis. Further work is required to examine the metabolic profile in the first 48 hours, exploring the underlying biological pathways.
Clinical outcomes of endovascular intervention and open surgery for Budd-Chiari syndrome in a single center
The Budd-Chiari syndrome is a heterogeneous group of disorders characterized by hepatic venous outflow obstruction at the hepatic venules, the large hepatic veins, the inferior vena cava, or the right atrium, regardless of the cause of obstruction. Pure inferior vena cava or combined inferior vena cava and hepatic venous obstruction is common in Asian countries, whereas, pure hepatic venous obstructions are frequent in Western countries. By the end of 2013, 20 191 cases of Budd-Chiari syndrome were reported from 258 Chinese hospitals (Zhang W et al., Gastroenterol Res Pract. 2015). Medical therapy and transjugular intrahepatic portosystemic shunts have become the mainstay treatment options in Western countries. Interventional treatment and surgery are the most common treatment modalities for Budd-Chiari syndrome in China. Currently, interventional treatment is much more common than surgery for Chinese patients (Qi XS et al. World J Gastroenterol. 2014). The aim of the study presented by Zhai was to evaluate the clinical outcomes of endovascular intervention or open surgery in patients affected by Budd-Chiari syndrome treated in a single Chinese center. A total of 418 patients (mean age, 48.5; 219 males) underwent an endovascular intervention or open surgery from January 2010 and October 2016. All were followed up for a median period of 48 months (range, 2–84). The hepatic venous balloon angioplasty (92 patients) and inferior vena cava balloon angioplasty (n=259) were the most common treatments used in the management of this cohort. Thrombolysis (n=19) and thrombectomy (n=6) were performed in patients with inferior vena cava thrombosis; surgical bypass was reserved for patients with a long occlusion of the inferior vena cava segment (12 patients). Overall, technical success was obtained in 427/429 subjects (99.5%). Immediate complications were identified in 10 patients (2.3%), 15 patients (3.5%) required reinterventions, and the overall mortality rate was 1.4% (6 patients). Thus, endovascular interventions played an important role in the management of Budd-Chiari syndrome. In addition, thrombectomy and surgical bypass were used to treat patients with complicated Budd-Chiari syndrome.
Tumor patients with peripherally inserted central venous catheter (PICC) correlation between upper limb deep vein thrombosis: risk factor analysis
Wu et al. analyzed risk factors related to upper limb deep vein thrombosis from 892 patients with cancer with a peripherally inserted central venous catheter. In the whole cohort, 22 upper limb deep vein thromboses were observed (incidence 2.5%). Catheter type, catheter-related complications, prothrombin time, and fibrinogen content were significantly associated with deep vein thrombosis at univariate and multivariate analysis (P<0.05). Sex, age, cancer type, associated diseases, catheter indwelling time, platelet count, prothrombin time, D-dimer, chemotherapy drugs, and chemotherapy reactions did not reach statistical significance (P>0.05). Therefore, a number of factors should be taken into account before and after a peripheral insertion of a central venous catheter to minimize peripherally inserted central venous catheter–related thrombosis.
Update on fibrinolysis
Fibrin formation drives fibrinolysis and plasminogen binds dead cells; hence, plasmin formation is driven by misfolded proteins. Medcalf stated that fibrinolysis should be viewed as a means to remove unwanted proteins, of which fibrin is one example. Removal of necrotic material is a key feature of the innate immune response, and plasmin can promote immunosuppression; consequently, tPA thrombolysis might increase the risk of infection. Next, Medcalf emphasized that the fibrinolytic system plays an important role in the central nervous system and tPA is abundantly expressed in the brain. Moreover, tPA is involved in memory and learning, cytokine activation of central nervous system immune cells, processing of neurotrophic factors, alteration of normal synaptic neurotransmission, fear, and anxiety. tPA/plasmin is a major regulator of blood-brain barrier permeability. In patients with ischemic stroke treated by tPA thrombolysis, symptomatic intracranial hemorrhage (sICH) can occur in 5% to 8% of patients. There is ≈1% risk of sICH in patients subjected to thrombolysis for myocardial infarction and pulmonary embolism. In conclusion, the speaker stated that fibrinolysis extends way beyond fibrin removal. Plasminogen activation is initiated whenever exposed lysine residues are presented (fibrin, misfolded proteins). There is a major role for this system in the central nervous system and in the immune response. Antifibrinolytic agents might do more than initially thought.
Targeted theranostic microbubbles: concurrent ultrasound diagnosis of thrombin and fibrinolytic treatment of thrombin
Imaging of thrombi provides an “on the spot” diagnosis, facilitates early treatment before the heart muscle is damaged, allows for direct monitoring of the success or failure of fibrinolytic therapy to lead to an early decision toward an interventional approach. Peter emphasized that, overall, such a technical advance could substantially reduce morbidity and mortality of cardiovascular diseases. Peter presented the activated GPIIb/IIIa as the ideal target for molecular imaging of thrombi. Platelets are the central component of clots and each platelet expresses ≈80 000 GPIIb/IIIa, which is specific for platelets. The concept is to produce recombinant antibodies to target specific activated GPIIb/IIIa receptors only. These recombinant antibodies are nonimmunogenic single-chain antibodies (scFv) with a small recombinant antibody fragment that are modifiable. Coupling can be promoted via genetic, biological, and chemical coupling methods. These antibodies have high yield of expression in bacteria, insect cells, and mammalian cells. The imaging modality is an ultrasound because it is noninvasive, has no ionizing radiation, is highly portable, provides real time images, and has no known side effects. The contrast agents are microbubbles. The speaker emphasized that bleeding is the major limitation of the current treatment of thrombosis. Theranostic microbubbles are a combination of diagnosis and therapy that are an emerging tool for personalized medicine. Theranostic microbubbles allow dual use of microbbubles for ultrasound imaging of thrombi and for localized delivery of a fibrinolytic drug. Peter concluded that targeted-theranostic microbubbles have a strong enrichment at the thrombus and allow real-time visualization of thrombi by ultrasound. They provide high thrombolytic potency and enable monitoring of the success or failure of therapy. Moreover, they avoid bleeding complications as the major limiting problem of current fibrinolytic therapy. Future potential applications of theranostic microbubbles include myocardial infarction, left atrial thrombi in atrial fibrillation, left ventricular thrombi, deep vein thrombosis, and pulmonary embolism.
Thrombophilia in nonthrombotic chronic venous disease of the lower limb – a systematic review
Chronic venous disease (CVD) represents a significant health care burden, presenting with a spectrum of clinical signs, including varicose veins and venous ulceration. Studies have proposed thrombophilia as a risk factor, particularly with respect to postthrombotic CVD. Its relationship to nonthrombotic CVD has not been comprehensively reviewed. Case-control studies, cohort studies, or randomized clinical trials (1946 to March 2017) reporting on the relationship of thrombophilia to nonthrombotic lower limb CVD in adult patients were included in the presented systematic review. Overall, 15 studies met the eligibility criteria, reporting on 916 cases and 1261 controls. Studies largely focused on venous ulceration and investigated multiple hemostatic factors. A direct relationship between thrombophilia and nonthrombotic CVD was identified, with greater prevalence and factor concentration alteration reported in patients compared with controls. The presence of multiple concomitant thrombophilia was also associated with earlier CVD onset. Targeting hyperhomocysteinemia with folic acid and factor VIII, PAI-1, and von Willebrand factor with aspirin shows promise in enhancing CVD treatment. Relationship strength between each case of thrombophilia and CVD varied, with the most common etiologies, such as factor V Leiden and elevated factor VIII, showing a clearer correlation than rarer ones, such as antithrombin deficiency. In conclusion, thrombophilia is associated with nonthrombotic CVD, but causation cannot be determined. Future research should focus on prospective studies with larger study populations to establish causation and then identify adjunct therapies targeting thrombophilia.
Villalta scores: is this time to bury it?
The Villalta scale is a clinical severity score for postthrombotic syndrome. It was originally proposed by Prandoni et al in 1992. It was introduced as an abstract in 1994, where it was termed the VS. It has been recommended as a reporting standard for use in clinical research by the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis. It is considered the gold standard instrument in comparison to the Ginsberg, Brandjes, and Widmer scoring systems because it was able to fulfill all necessary validation criteria. Lattimer, who referred mostly to a previously published paper (Lattimer CR et al. J Vasc Surg Venous Lymphat Disord. 2014;2(1):8-14), focused on a number of limits and points of weakness in this scale. First, in the aforementioned study, any relationship between the patient-reported clinical symptoms and the physician-recorded signs was found. Therefore, patients with severe symptoms may have minimal signs and vice versa. Second, in the Villalta scale, there is no provision for assessing the degree of venous ulceration or for venous claudication. Third, the scale may be somewhat nonspecific as some of the symptoms and signs it assesses are not specific to venous disease and are poorly defined. Finally, other problems might be cardinality and illogical weighing in favor of symptoms. In conclusion, in the opinion of the author, the Villalta scale has limited value in the assessment of postthrombotic syndrome and its gold-standard status should be revoked.
Correlation of clinical and ultrasound parameters used to assess the severity of postthrombotic syndrome in patients after popliteal-femoral deep vein thrombosis
Patients with a first unprovoked proximal deep vein thrombosis who had completed a 6-month course of anticoagulation and presented a clinical picture of postthrombotic syndrome (5 or more points on the Villalta scale) other than signs of residual vein thrombosis of the popliteal-femoral venous segment were enrolled in this study. Residual vein thrombosis was defined as a residual thrombus occupying at least 20% the cross-section of the vein. All patients were followed up for 12 months and underwent clinical and ultrasound examination at enrollment, at 6 months and at 12 months. The clinical evaluation was performed using the Villalta scale, venous clinical severity score (VCSS), Venous Segmental Disease Score (VSDS), chronic venous disease questionnaire (CIVIQ-20), and the modified Marder score. Overall, 60 patients were included; 7 were excluded from the final analysis because they developed a recurrent deep vein thrombosis. During the 12-month follow-up, a direct, significant correlation (Pearson index) among VCSS, Villalta, and CIVIQ-20 scores was observed. The correlation between the severity of the hemodynamic changes (VSDS and Marder scores) and the clinical severity of postthrombotic syndrome (VCSS, Villalta, and CIVIQ-20 scores) was variable and characterized by low and moderate strength. The dynamic changes in the mean values of VCSS, Villalta, CIVIQ-20, and Marder scores were characterized by a strong and significant correlation. Dynamic changes in the mean value of the VSDS score did not correlate with other parameters. The parameters investigated showed a good correlation with each other during the follow-up. In the author’s opinion, they should be used together for a comprehensive assessment of clinical severity and hemodynamic disturbance in postthrombotic syndrome.
Postthrombotic syndrome is reduced by lipid-lowering therapy
Recently, atorvastatin and rosuvastatin were shown to inhibit the development of varicose veins (Eschrich J et al. J Am Heart Assoc. 2016;5(2):e002405). In this study, the influence of lipid-lowering therapy with statins on postthrombotic syndrome development was tested. Between January 2002 and March 2017, 551 patients were treated for deep venous thrombosis in their institution. The Villata scoring system was used for the assessment of the severity of postthrombotic syndrome, and 421/551 (76%) patients developed postthrombotic syndrome and 61/551 (11%) received lipid-lowering therapy. All patients were treated conservatively with compression stockings and all patients received therapeutic anticoagulation, except for 2 patients who refused therapy. Patients underwent ultrasound examination after 2 weeks, 3 months, 6 months, and annually thereafter; of these patients, 192/551 (35%) had recurrent deep vein thrombosis and received life-long therapeutic anticoagulation, 381/487 (78%) patients without lipid-lowering therapy presented with postthrombotic syndrome, and 40/61 (65%) patients with lipid-lowering therapy presented with postthrombotic syndrome (P=0.027). Severe postthrombotic syndrome (mean Villata score, 16.8) appeared in 12/381 (3%) patients not receiving lipid-lowering therapy, but no events were observed in the lipid-lowering group. In their study, the risk of recurrent deep vein thrombosis was not lowered by lipid-lowering therapy. The low number of patients receiving lipid-lowering therapy might be explained by a higher incidence of deep vein thrombosis in patients <35 years old since 2011 (77/310 [25%]). In conclusion, postthrombotic changes and severe postthrombotic syndrome might be reduced by lipid-lowering therapy.
Combined use of micronized purified flavonoid fraction with oral rivaroxaban reduce the incidence of postthrombotic syndrome at six month after proximal deep vein thrombosis
Lobastov talked about a pilot, randomized, open-label study enrolling 40 patients (mean age of 57.1±14.3 years; 27 men) suffering from a first acute femoral-popliteal deep vein thrombosis. All participants were randomized into two groups. In the control group (n=18), all patients received a standard treatment with oral rivaroxaban and graduated compression stockings (20 to 40 mm Hg) for 6 months. In the treatment group (n=22), an additional treatment with MPFF 1000 mg per day was prescribed for the whole treatment period. After 6 months, patients were assessed with Villalta score and venous clinical severity score (VCSS) score. The median Villalta score in the group treated with MPFF was significantly lower compared with the control: 2.0 vs 6.0 (P<0.0001); the same difference was found for the VCSS score. According to the Villalta score, postthrombotic syndrome was diagnosed in 6 of 22 patients in the experimental group and in 13 of 18 patients in the control (P=0.01). Nobody manifested a severe postthrombotic syndrome. In conclusion, MPFF use seems to reduce the incidence of postthrombotic syndrome at 6 months from the index deep vein thrombosis in patients treated with oral rivaroxaban without any additional adverse effect.
Reducing sludge in deep veins with neuromuscular stimulation
When the blood flow slows or stops for an instant, echobright aggregates appear within the vein lumens. Lattimer explained that this “erythrocyte sludge” can be quantified using a grey-scale index (0-255) termed the “venous sludge index” (VSI). The aim of the submitted study was to investigate the effect of the common peroneal nerve stimulator (CPNS) on venous sludge formation. For this purpose, the right popliteal vein of 25 healthy volunteers was evaluated using B-mode ultrasound in longitudinal and transverse views, with patients in standing and lying positions. A single frame out among 154 frames (7 seconds) was selected from the video records using a random number generator (Random.org). Image analysis (ImageJ®) was used to measure the VSI. The CPNS device significantly reduced the VSI irrespective of the subject’s position or the view of the transducer (P<0.0005, Wilcoxon). Namely in the transverse view, CPNS reduced the VSI from a median value of 20.7 (IQR, 13.6-32.2) to a median value of 1.1 (IQR, 0.6-2.7) when standing and from 11.4 (IQR, 6.3-15.9) to 0.8 (IQR, 0.5-2.1) when lying. Similar results were obtained in the longitudinal view (from 27.7 [IQR, 18.8-41.4] to 2 [IQR, 1.1-3.2] when standing; from 11.7 [IQR, 5.5-17.5] to 1.5 [IQR, 0.5-3.1] when lying). The author concluded that venous sludge and stasis are significantly reduced using the CPNS device. Since stasis is a significant component of Virchow’s triad, this may explain the principle mechanism of action of CPNS in reducing the risk of venous thromboembolism. However, the exact relationship between stasis, aggregation, and thrombosis requires more research.
Clinical efficacy of electrical calf muscle stimulation in patients with residual venous obstruction and postthrombotic syndrome
The author presented the results of a prospective observational study involving 60 patients (mean age, 58.5±11.4; 38 men) suffering from a first unprovoked femoralpopliteal deep vein thrombosis, presenting with a residual venous obstruction, and a Villalta score >5 points after a 6-month course of anticoagulation therapy. During the 12-month follow-up, the patients underwent monthly ultrasonography to reveal any recurrent deep vein thrombosis. In the overall cohort, postthrombotic syndrome was treated by active walking, below-knee graduated compression stockings, and micronized purified flavonoid fraction. The efficacy of electrical calf muscle stimulation was tested in 30 patients (treatment arm) using the Veinoplus VI device (30 minute treatment sequences, 3 times a day). Villalta, venous clinical severity score (VCSS), and chronic venous disease questionnaire (CIVIQ-20) scores were assessed at baseline and every 6 months of treatment. Recurrence of deep vein thrombosis was found in 7 of 30 patients in the control group and in 0 of 30 patients in the treatment group (P=0.011). All the recurrent deep vein thromboses were excluded from subsequent analysis. Patients in the treatment group showed a significant tendency for a decrease in the scores throughout the day: VCSS score (9.9±1.6 / 7.8}1.6 / 6.1±1.5 [P<0.0001], Villalta score (18.9±3.9 / 12.8±4.0 / 8.3±2.7 [P<0.0001], and CIVIQ-20 score (67.8±8.4 / 51.3±8.4 / 40.0±10.5 [P<0.001)]. In the control group, a similar trend was observed for the VCSS score (8.1±2.8 / 7.3±2.1 / 7.2±2.1 [P=0.014]); for the Villalta score (12.7±6.7 / 10.9±5.6 / 10.2±5.4 [P=0.002]), but not for the CIVIQ-20 score (48.2±19.3 / 46.7±17.3 / 47.4±16.2 [P>0.05]). The author concluded the use of electrical calf muscle stimulation technology can reduce the clinical severity of postthrombotic syndrome and increase quality of life in patients with residual venous obstruction.
Antiphospholipid Syndrome
Antiphospholipid syndrome: a history over 30 years
Antiphospholipid syndrome is an autoimmune disease in which thrombosis and/or pregnancy morbidity occur in patients with persistently positive antiphospholipid antibodies (aPLs). The role of aPLs in thrombosis is widely recognized, but the pathogenic mechanisms triggering thrombosis in antiphospholipid syndrome are only partially understood. Over the last decades, intensive research on the mechanisms of aPL-mediated thrombosis has substantially advanced the knowledge of the pathophysiology of antiphospholipid syndrome. In 1984, Koike at al described the enzyme-linked immunosorbent assay system that detected circulating anticardiolipin antibodies (aCL) directly in patients with systemic lupus erythematosus who revealed a biological false positive serological test for syphilis. In 1990, three groups, including their group, independently reported the necessity of a cofactor for the binding of autoimmune aCL to the solid phase phospholipids. β2-glycoprotein I (β2GPI) was identified as this cofactor. In 1994, the epitope for aCL was shown to develop when β2GPI is adsorbed on polyoxygenated polystyrene plates. In 2000, Koike et al described that antiprothrombin antibodies bind to prothrombin exposed to immobilized phosphatidylserine and established a phosphatidylserine-dependent monoclonal antiprothrombin antibody. In 2004, a novel role of nicked β2GPI was identified in the negative feedback pathway of extrinsic fibrinolysis. Nicked β2GPI was found to bind angiostatin and attenuate its antiangiogenic property. In 2004, Koike et al demonstrated that, in the cells stimulated by human monoclonal anti–β2GPI antibodies, p38 mitogen-activated protein kinase phosphorylation was observed in the presence of β2GPI. Furthermore, they found that complement activation was essential for thrombus formation in patients with the antiphospholipid syndrome in vivo. Very recently, β2GPI was identified as a complement regulator. The crosslink between complement activation and prothrombotic status in patients with antiphospholipid syndrome has drawn much attention. Genetic factors are hypothesized to play a role in the susceptibility to antiphospholipid syndrome based on several family studies in patients with aPL and/or clinical manifestations of antiphospholipid syndrome.
Antiphospholipid syndrome: classification and diagnosis
The antiphospholipid syndrome is a prothrombotic disorder that can affect both the venous and arterial circulation. The deep veins of the lower limbs and the cerebral arterial circulation are the most common sites of venous and arterial thrombosis, respectively. However, any tissue or organ vascular bed can be affected. According to the revised classification criteria in 2006, a diagnosis of antiphospholipid syndrome is made if at least one of the clinical manifestations and one of the laboratory criteria are met. Clinical criteria include vascular thrombosis or pregnancy morbidity, such as unexplained fetal deaths at or beyond the 10th week of gestation; premature births before the 34th week of gestation because of eclampsia or severe preeclampsia or placental insufficiency; three or more unexplained consecutive spontaneous abortions before the 10th week of gestation. Laboratory criteria involve the persistence (for >12 weeks) of lupus anticoagulants or of high titers of autoantibodies of the IgG or IgM isotype for anti–β2-glycoprotein I or anticardiolipin antibodies, detected by enzyme-linked immunosorbent assay or by lupus anticoagulant assays. A diagnosis of antiphospholipid syndrome should not be made if a period of greater than 5 years separates the clinical event and the positive laboratory results.
The classification criteria have been designed for the group level and the research purposes are to compare like populations, to reach high sensitivity and sensibility, and to omit patients with rare manifestations. However, patients who do not fulfill the criteria can be diagnosed as having the disease. As an example, thrombocytopenia, autoimmune hemolytic anemia, heart valve thickening and dysfunction, and live do reticularis, which are not part of the formal clinical classification criteria for antiphospholipid syndrome, have been associated with patients diagnosed with antiphospholipid syndrome. Screening should be limited to patients with a significant probability of having antiphospholipid syndrome. The probability can be considered low if venous or arterial thrombotic events occur in elderly patients; moderate in asymptomatic patients with a prolonged activated partial thromboplastin time (aPPT), in provoked venous thromboembolism events occurring in young patients, or in recurrent early pregnancy loss. On the other hand, the probability of having antiphospholipid syndrome should be considered high in the presence of unprovoked venous or arterial thrombotic events in patients younger than 50 years, in atypical thrombosis, in late pregnancy loss, or in manifestations of thrombosis or pregnancy morbidity occurring in patients with autoimmune diseases.
The commonly used term antiphospholipid antibodies is a misnomer. Indeed, the antiphospholipid antibodies that characterize antiphospholipid syndrome do not directly bind to phospholipids. The main antiphospholipid syndrome autoantigen is β2-glycoprotein I (β2GPI), an abundant plasma protein that binds to anionic phospholipids. The lupus anticoagulant test measures the ability of antiphospholipid antibodies to prolong phospholipid-dependent clotting reactions. Both aPTT-based assays and dilute Russell’s viper venom time (dRVVT) are suitable for lupus anticoagulant tests, if the aPTT used for lupus anticoagulant testing is lupus anticoagulant sensitive. In a case-control study, which focused on the stroke risk factors in women in the general population <50 years old, 17% of the patients with stroke were positive for lupus anticoagulant vs 0.7% of controls (odds ratio, 43.1). The risk was further increased by taking oral contraceptive pills (odds ratio, 201.0) or smoking (odds ratio, 87.0). Approximately 1% of women trying to get pregnant have recurrent miscarriages; of these women, approximately 10% to 15% are estimated to have obstetrical antiphospholipid syndrome. Positivity for lupus anticoagulant is the strongest predictor of subsequent thrombosis in purely obstetrical antiphospholipid syndrome.
The specific antiphospholipid antibodies responsible for lupus anticoagulant activity are anti–β2GPI and anti–PT. Although both anti-β2GPI and anti–PT can be responsible for a positive lupus anticoagulant result, it has been noted that the lupus anticoagulant due to anti–β2GPI antibodies correlates the strongest with thrombosis. Simultaneous anticardiolipin antibodies, anti–β2GPI, and lupus anticoagulant (socalled “triple-positive” patients) do not predict an adverse pregnancy or thrombotic events better than lupus anticoagulant alone does.
Management of thromboembolism (venous & arterial) in patients with antiphospholipid syndrome
Erkan discussed the management of patients with antiphospholipid syndrome: clinical manifestations of antiphospholipid syndrome represent a spectrum, not every positive antiphospholipid syndrome result is “clinically significant,” and thrombosis is multifactorial. The speaker emphasized that the optimal agent for secondary thrombosis prophylaxis is warfarin, but there is an increased risk of bleeding and frequent blood monitoring is required. In a noninferiority open-label study, rivaroxaban was compared with warfarin. The results showed that rivaroxaban was inferior to warfarin. The 15th international congress task force on antiphospholipid syndrome stated that insufficient evidence exists to make recommendations at this time regarding the use of direct oral anticoagulants in patients with antiphospholipid syndrome. The optimal international normalized ratio (INR) for secondary venous thromboembolism prophylaxis is 2.0 to 3.0 and for secondary AT prophylaxis, the target INR is 2.0-3.0 with consideration for the use of low-dose aspirin. The optimal duration of secondary thrombosis prophylaxis is unknown because of poor-quality data describing the risk of recurrence in patients with antiphospholipid syndrome and prior venous thromboembolism. The speaker emphasized that the ideal strategy should be stratified by risk. High-intensity anticoagulation is not supported by randomized controlled trials. The role of warfarin alternatives is unknown and the necessity of life-long anticoagulation is controversial. Erkan introduced the catastrophic antiphospholipid syndrome as a rare condition associated with high mortality. Early and aggressive treatment with anticoagulation + corticosteroids + intravenous immunoglobulin / plasma exchange (±rituximab) is critical. The microthrombotic antiphospholipid syndrome is a vasculopathy characterized by endothelial proliferation resulting in nephropathy, decidual vasculopathy, cognitive dysfunction, livedo, and pulmonary hypertension. The treatment with sirolimus works by inhibiting the mTOR pathway (Canaud G et al. N Engl J Med 2014;371(4):303-312).
Antiphospholipid syndrome: Management
Antiphospholipid antibodies (aPL) are a family of autoantibodies directed against phospholipid-binding plasma proteins, most commonly β2-glycoprotein I. Thromboembolic manifestations of aPL range from microthrombosis to arterial/ venous thrombosis to catastrophic antiphospholipid syndrome. Primary thrombosis prevention in persistently aPL-positive individuals requires a risk-stratified approach, elimination of reversible thrombosis risk factors, and prophylaxis during highrisk periods. The effectiveness of low-dose aspirin is not supported by prospective controlled studies; it can be considered in aPL-positive patients with additional cardiovascular disease risk factors. Laboratory evidence of aPL in patients with a first episode of venous thromboembolism is often considered an indication for indefinite anticoagulant therapy, but it is uncertain if this practice is justified. A recent systematic review showed that the unadjusted risk ratio for recurrent venous thromboembolism after stopping anticoagulant therapy in patients was 1.53 with an anticardiolipin antibody (95% CI, 0.76-3.11) and 2.83 with a lupus anticoagulant (95% CI, 0.83- 9.64). However, all studies included had important methodological limitations and the authors judged the overall quality of the evidence as very low. Thus, prevention of secondary thrombosis lacks a risk-stratified approach; the effectiveness of high intensity anticoagulation is not supported by prospective controlled studies. Moreover, at this time, insufficient evidence exists to make recommendations regarding direct oral anticoagulation in antiphospholipid syndrome. More data will be drawn from the results of three ongoing trials: the Rivaroxaban in Thrombotic Antiphospholipid Syndrome trial (RAntiphospholipid syndrome), the Apixaban for the Secondary Prevention of Thromboembolism Among Patients With the Anti Phospholipid Syndrome trial (ASTRO Antiphospholipid syndrome), and the Rivaroxaban for Antiphospholipid Antibody Syndrome trial (TRAntiphospholipid syndrome). Patients with antiphospholipid syndrome usually receive a combination of anticoagulation, corticosteroids, and intravenous immunoglobulin and/or plasma exchange. Recent studies, based on newly understood mechanisms, suggest that novel approaches that target new immunomodulatory pathways, eg, statins, hydroxychloroquine, B-cell inhibition, complement inhibition, and mammalian target of rapamycin (mTOR) pathway inhibition, can be considered in the management of selected aPL-positive patients.
Update on classification of antiphospholipid syndrome
Erkan introduced the updated Sapporo criteria for antiphospholipid syndrome. Antiphospholipid syndrome is diagnosed when vascular thrombosis and/or pregnancy morbidity and laboratory criteria are present. An international consensus statement was published in 2006. The speaker discussed the distinction between diagnostic and classification criteria. Classification criteria are standardized definitions that are primarily intended to enable clinical studies to have uniform cohorts for research. Diagnostic criteria are a set of signs, symptoms, and tests developed for use in routine clinical care to guide the care of individual patients. The goal of classification criteria is to define the study sample representative of the majority well, and the goal of the diagnostic criteria is to recognize all patients, including unusual presentations. Classification criteria are for research, have no treatment implications for patients, and should have little or no impact on billing and reimbursement. Diagnostic criteria are for diagnosis, have treatment implications, and implications for billing and reimbursement. Erkan reported on the limitations of current antiphospholipid classification criteria. He gave representative examples of heterogeneous manifestations of antiphospholipid syndrome, such as livedo reticularis, thrombocytopenia, or heart valve disease. Also, a clear definition of pregnancy morbidity criteria for a definition of a “positive” antiphospholipid syndrome test is missing. ACR/EULAR published new recommendations for the development and validation of criteria sets, based on contemporary standards of measurement. Then the speaker presented ACR/EULAR endorsed methodology for the development of classifications and response criteria for rheumatic diseases. Phase 1 is item generation, phase 2 is item reduction, phase 3 is item reduction, weighting, and scaling, and phase 4 is refinement and validation. In conclusion, Erkan emphasized that there are no diagnostic criteria for antiphospholipid syndrome, but development of new classification criteria is in progress. Classification criteria are commonly used for antiphospholipid syndrome diagnosis, which is not ideal, but acceptable as a guide to prevent over diagnosis or misdiagnosis.
An update on the diagnosis and management of antiphospholipid syndrome
New clinical, laboratory, and experimental insights since the 1999 publication of the Sapporo preliminary classification criteria for antiphospholipid syndrome were addressed at a workshop in Sydney, Australia, before the Eleventh international congress on antiphospholipid antibodies. According to the revised classification criteria (2006), a diagnosis of antiphospholipid syndrome is made if at least one of the clinical manifestations and one of the laboratory criteria are met. Clinical criteria include vascular thrombosis or pregnancy morbidity, such as unexplained fetal deaths at or beyond the 10th week of gestation; premature births before the 34th week of gestation because of eclampsia or severe preeclampsia or placental insufficiency; three or more unexplained consecutive spontaneous abortions before the 10th week of gestation. Laboratory criteria involve the persistence (for >12 weeks) of lupus anticoagulants (LA) or of high titers of autoantibodies of the IgG or IgM isotype for anti–β2-glycoprotein I or anticardiolipin antibodies, detected by enzyme linked immunosorbent assays (ELISA) or by lupus-anticoagulant assays. A diagnosis of antiphospholipid syndrome should not be made if a period of greater than 5 years separates the clinical event and the positive laboratory results. The classification criteria have been designed for the group level and research, and their purposes are to compare like populations, to reach high sensitivity and sensibility and to omit patients with rare manifestations. However, patients who do not fulfill the criteria can be diagnosed as having the disease.
Thromboprophylaxis remains one of the major challenges in antiphospholipid syndrome. Conventional management of cardiovascular risk factors by lifestyle changes is key in primary thromboprophylaxis. The use of antiplatelet agents, such as low-dose aspirin should be limited to individuals at very high risk. Management of asymptomatic individuals with persistent antiphospholipid antibodies is assessed on an individual basis, taking the presence of additional cardiovascular risk factors into account. Individuals with a high-risk profile (that is, those with high antiphospholipid antibody titers, triple positivity, or additional cardiovascular risk factors) may be considered for primary prevention with low-dose aspirin or hydroxychloroquine. In high-risk situations, such as surgery and long-term immobilization and in postpartum women, all individuals with persistent antiphospholipid antibody positivity should receive thromboprophylaxis with low-molecular-weight heparin. Secondary thromboprophylaxis is based on anticoagulation, mainly with vitamin K antagonists (such as warfarin or heparin), although direct oral anticoagulants might have a role as well. Individuals who are positive for antiphospholipid antibodies and who have had an arterial or venous thrombosis, but do not meet criteria for antiphospholipid syndrome should be managed in the same way as antiphospholipid antibody-negative patients with thrombotic events. Patients with definite antiphospholipid syndrome and a first venous thrombosis should receive oral anticoagulant therapy to a target international normalized ratio (INR) of 2-3. Patients with definite antiphospholipid syndrome and arterial thrombosis should receive vitamin K antagonists with a target INR >3 or vitamin K antagonists with a target INR of 2-3 in combination with low-dose aspirin. For patients without systemic lupus erythematosus with a first noncardioembolic cerebral arterial event who have a low-risk antiphospholipid antibody profile and reversible triggers, antiplatelet agents should be considered on an individual basis. Duration of therapy in patients with definite antiphospholipid syndrome and thrombosis is indefinite. Anticoagulation could be limited to 3 to 6 months in patients with a first venous event with a low-risk antiphospholipid antibody profile and a known transient precipitating factor. Potential alternative therapies for patients who have recurrent thrombosis, fluctuating INR levels or major bleeding, or, for those who are at high risk of major bleeding, include long-term low-molecular-weight heparin, hydroxychloroquine, or statins.
Interventional Radiology
Interventional radiology
The National Venous Registry demonstrated favorable outcomes when using catheterdirected thrombolysis in the treatment of acute iliofemoral deep vein thrombosis. These outcomes were maintained at the 1-year follow-up. After the registry data, there have been several reports showing that local delivery of thrombolytics combined with mechanical thrombolysis provides good technical results with a lower use of thrombolytics and lower complication rates. Two randomized trials subsequently looked at venous patency and reflux after thrombolysis and demonstrated that successful thrombolysis results in improved venous function. If thrombolysis improves venous function with a lower incidence of reflux and obstruction, the expectation would be improved clinical outcomes and better quality of life. It was reported that patients who underwent thrombolysis had better overall physical functioning, less stigma, less health distress, and fewer postthrombotic symptoms when compared with those treated with anticoagulation. Quality of life results were directly related to the initial success of thrombolysis. To date, there is no large randomized prospective study available to support the use of these techniques. Recently, the 8th American College of Chest Physicians guidelines included a level 2C recommendation, the use of catheter-directed thrombolysis in combination with pharmacomechanical thrombectomy (PhMT) in extensive acute proximal deep vein thrombosis to reduce symptoms and postthrombotic morbidity. Venous thrombectomy has also been used for treating acute proximal thrombosis with good long-term outcomes, which were better when compared with anticoagulation alone. The number of patients with deep vein thrombosis that would benefit from thrombolysis is not known. It is important to mention that these guidelines were taken from a consensus statement and are not strictly based on evidence.
Interventional radiology
There have been two main treatments for acute pulmonary embolism: anticoagulant therapy alone or systemic thrombolytic therapy. Although systemic thrombolytic therapy is effective at preventing deaths from pulmonary embolism, it markedly increases bleeding, including intracranial and fatal bleeding. Catheter-directed thrombolysis (CDT) was initially developed for the treatment of arterial, dialysis graft, and deep vein thromboses (leg or arm). When used to treat acute pulmonary embolism, a wire is usually passed through the embolus, followed by placement of a multiside hole infusion catheter through which a thrombolytic drug is infused over 12 to 24 hours. The delivery of the drug directly into the thrombus is expected to be as effective as systemic therapy, but to cause less bleeding because a much lower dose of the drug is used. If more rapid thrombus removal is required, such as in a decompensating patient, then fragmentation, balloon maceration, and aspiration may be used as an adjunct to CDT or instead of it (ie, in patients with a high risk of bleeding).
These mechanical techniques, however, are avoided in stable patients because they may cause pulmonary artery injury. The addition of an ultrasound-emitting wire to a multiside-hole infusion catheter is thought to accelerate thrombolysis by ultrasonically disrupting the thrombus. Although this approach has been used to treat arterial and deep venous thromboses for about 10 years, there is uncertainty that the addition of ultrasound emission increases the efficacy of CDT, based partly on the findings of the SEATTLE II study (A Prospective, Single-Arm MultiCenter Trial of EkoSonic Endovascular System and Activase for Treatment of Acute Pulmonary Embolism). If there is need for active thrombus removal in patients with a very high risk of bleeding, it may be necessary to use catheter-based therapy without a thrombolytic drug or to use surgical embolectomy. We are not ready to encourage the use of CDT in preference to anticoagulation alone in stable patients with acute pulmonary embolism and right ventricular dysfunction. We suggest that there is a need for evidence that the short- and long-term benefits of CDT outweigh the associated risk of bleeding before CDT can be recommended for such patients. Randomized trials that compare CDT with systemic thrombolytic therapy in unstable patients with pulmonary embolism and compare CDT with anticoagulation alone in stable patients who have a large pulmonary embolism and right ventricular dysfunction are still needed.
New Technologies
News on artificial vein valves: chances and limits
Sail is a percutaneously applied monocusp PTFE valve with a physiologic leak. It was pivotally studied in the iliac veins of 10 pigs. Femoral vein access was conducted using a 6Fr system with a 100% deployment rate expanding to 10 mm. The results 4 weeks postprocedure, as documented by an ascending venogram, showed a 100% patency rate. Descending venogram applied to 8 valves revealed 5 with full competency. Histology showed no macroscopic thrombus on the valve. VenoValve is a porcine heart valve derived monocusp, which can theoretically tailor inflow/outflow size mismatch. Its open insertion allows exact placement, resulting in better flow dynamics and less size mismatch. InterVene is an endovenous valve formation system applied percutaneously the form a monocusp valve. The Maleti Neovalve, instead, necessitates a surgical procedure, creating mono or bicuspid neovalve generation using the fibrotic tissue within the native valve. The critical point is to determine who really needs these techniques and if these are first-line or final-line care. A realistic algorithm must be followed, and include C4-C6 patients with deep vein reflux is obligatory in this stage for these techniques.
Water-assisted liposuction
Since lipedema causes a lifelong growth in fat tissue, it is crucial to target a surgery during stage 1, when the first typical pain appears and a certain diagnosis can be made. The guidelines agree that gentle liposuction is the best treatment method. Waterjet-assisted liposuction is a groundbreaking method in the field. The fat tissue is infused with saline solution via thin cannulas. Highly concentrated anesthetics are added to the solution. The fat cells dilute after 1 to 2 hours, which is due to the solution used to drain the fat tissue. Subsequently, the slurry of fat and saline is suctioned via 3 to 4 mm thin, vibrating cannulas. A pulsating water jet sprays the tumescent solution into the fat tissue for anesthesia, and then the liposuction can start just a few minutes later. The waterjet flushes the fat cells out of the tissue like a pressure washer, which are simultaneously suctioned. The fat separates from the solution inside the collection container, so the removed amount of fat can be measured precisely. The waterjet-assisted liposuction method reduces the amount of surgery time by up to 1 hour, additionally removing more fat and leaving behind a visibly thinner leg.
Hyaluronan venoplasty: how to modify venous hemodynamics
In 2013, vein shaping with perivenous hyaluronan gel was introduced. The reason to use hyaluronan was that it has the best tissue compatibility of all known synthetic fillers and because of its simpler and smoother injection properties. It is applied intrafascially. Criteria for a good percutaneous valvuloplasty are listed as a selection of patients with intact and mobile cusps, hyaluronan gel with an appropriate injection technique to place a minimal amount of gel to the vein wall. The first study was conducted in 2013 in 23 patients with proximal valve incompetence of the great saphenous vein, with two additional studies, which followed the first. There were no considerable complications. The durability of the orthograde flow was 6 to 36 months, where the effect lasts longer than the detectable hyaluronan volume. In conclusion, it is a simple, easily adjustable, rechargeable, minimally invasive procedure suitable for early stages of venous valve insufficiency.
Real-time, cloud-based phlebologic documentation
By providing computing resources as a service rather than a product, cloud computing is revolutionizing access to software, processing power, and storage. When you take a picture, it appears automatically and wirelessly on a 4k HD screen. Each comment written may be seen on any other PC in real time, the person who wrote each phrase is known, and information is available about which device was used and at what time. In a case of loss, data can be restored by inserting in the date before it was lost. Documentation is saved for 35 years, fulfilling requirements of the Medical and Juridical standards. Data protection is provided by a dual password system. In the author’s experience, it is a speech recognition solution designed for physicians, which has been integrated into electronic health records.
Randomized control trial: dosing of electrical stimulation in venous insufficiency
The potential benefit of a footplate neuromuscular electrical stimulation device in patients with chronic venous disease was investigated in a pilot randomized controlled trial consisting of 22 patients with clinical, etiological, anatomical, pathophysiological (CEAP) classification C3 to C5. The results were consistent with a significant increase in venous blood flow parameters, a reduction in edema, and a significant improvement in the Aberdeen varicose vein questionnaire. A significant increase in local microcirculatory flux and temperature was obtained with neuromuscular electrical stimulation (NMES). In conclusion, it appears acceptable to individuals with chronic venous insufficiency, it improves hemodynamics, prevents orthostatic edema, and improves clinical severity, although no quality of life benefit was observed.
New generation of transilluminated powered phlebectomy (Trivex) procedures utilizing only tumescent anesthesia in appropriately selected patients: are the patients satisfied?
Classic phlebectomy can be a painstaking, lengthy procedure and the outcome can be compromised if segments of veins are missed due to a lack of visualization. The left hand pump of the system is dedicated to providing the tumescence anesthesia via the Trivex system illuminator, while the right hand pump is dedicated to providing saline to the Trivex Resector Handpiece for resector tip irrigation. Prior to the procedure, with the patient in a standing position, venous clusters are outlined with an ink marker. The results of 66 TIPP procedures in the author’s series revealed an average time of 61 minutes per leg with a satisfactory pain score. Patient satisfaction was 60%. Reasons for nonsatisfaction were pain and bad cosmetic results. In conclusion, use of the Trivex system results in one treatment session, no need for duplex skills, a lower rate of recurrent varicosities and less thrombophlebitis. It abolishes the risks of intra-arterial injection, skin necrosis, and residual hyperpigmentation. Compared with classic phlebectomy, the Trivex system results in fewer incisions, shorter procedure times, reduced postoperative pain, less chance of missed varicosities, and a lower rate of recurrent varicosities. Trivex also allows for removal of problematic veins.
Computational fluid dynamics analysis for the portal venous system and the simulation of a portosystemic shunt based on a CT scan feasibility study
Anatomically, the portal vein can be seen in tomography images by using either contrast-enhanced CT or MRI. However, no quantitative information, such as its flow velocity and pressure can be achieved. A transjugular intrahepatic portosystemic shunt (TIPS) is a kind of hemodynamic treatment for portal hypertension, but it is far from perfection. Computational fluid dynamics defines the physical bounds of the target vessel, divides the volume occupied by the fluid into discrete cells, and starts the simulation; a postprocessor is used for the analysis and visualization of the resulting solution. New perspectives may be found with further study, especially regarding stent graft design and the quality control of the TIPS procedure.
Ultrasound-guided foam phlebectomy
Ultrasound-guided foam phlebectomy was performed as an adjunctive treatment for eliminating residual varicosities in patients having undergone earlier truncal ablation in a small prospective “proof of concept” trial 11 on consecutive patients. Standard clinical marking of varicosities was performed. A 1.5% sodium tetradecyl sulfate foam solution (3 to 10 mL, 1:4 Tessari with 100% O2) was administered to the veins to be avulsed, allowing the target varicosities to be readily identified on ultrasound. Ambulatory phlebectomy was first performed in the usual surgical manner. Ultrasound guidance was then used to confirm completeness of the vein removal and direct further placement of incisions and guide hook placement if residual varicosities were identified. The number of additional incisions directly related to ultrasound guidance was recorded. Patients were reviewed clinically and with an ultrasound around 1 week (5 to 14 days) to determine the success of the treatment and exclude complications. All patients had additional incisions (2 to 4) that were a direct result of ultrasound guidance, allowing for a more complete removal of target veins than with a “standard” phlebectomy. No complications were encountered at follow-up. Early results suggest that ultrasound-guided foam phlebectomy is safe and improves the effectiveness of vein clearance with ambulatory phlebectomy.
Wise information technology (WIT) for venous thromboembolism
The Wise information technology uses ultrasound and CT for diagnosis. The system key words are venous thromboembolism and pulmonary embolism, and a warning is obtained with the PC_HIS system, mobile phone (APP, WeChat). Warning targets are doctors, nurses, vascular surgeons, or respiratory physicians. It is automatically generated for consultation with the aim of achieving a zero delay to treat all venous thromboembolisms in time.
IVUS in venous disease and the M2 core system
Saha introduced intravascular ultrasound (IVUS) as an established technique for identifying venous lesions. Venography has poor diagnostic sensitivity and in the recently published multicenter study VIDIO, IVUS was described as the gold-standard technique for identifying iliac vein obstructions. Several advantages of IVUS over venography were highlighted. The most specific advances are deciding the degree of lesion stenosis, deciding the landing zones, and providing quality control after intravascular procedures. Next, the New CORE M2 intravascular imaging system was introduced as an example of technological evolution. At the end of his lecture, Saha summarized the advantages of IVUS as reduced radiation, reduced contrast, repeatability, and improved sensitivity of diagnostic testing.
Can innovative compression textile technology keep up with recent research?
The study presented by Andreas Nilsonn won the Venartis Innovation Award. Nilsonn mentioned a recent study published by Mosti and Partsch on a new two component compression system, turning an elastic bandage into an inelastic compression device. The speaker emphasized that pressure can be controlled by smart textiles. The aim of the study was to evaluate if a stocking with novel textile technology can apply a uniform pressure on the lower leg regardless of leg shape and leg size. This was an early study of a new stocking with a smart textile (Lundatex Stocking, PressCise AB, Sweden) on 10 healthy subjects. Interface pressure was measured with a Picopress on different points of the leg. The results showed a consistent uniform pressure at the different points, no custom fitting, and maintaining pressure during deswelling/ swelling. The presenter concluded that further studies are required to study the hemodynamic effects and the clinical effectiveness.
Next generation micro-foam preparation
Roche discussed the pros and cons of physician-compounded foam and of the finished product Varithena®. He developed a former device to standardize the technology, offer more safety, expand the indications of treatment, and modernize and improve a well-accepted technique. Roche presented a comparison study of foamer device and the “Tessari” method. The results showed that the foamer device is useful in manufacturing foam, the foamer bubbles have a more homogenous size, and the foam from the foamer is up to 4x more stable. In conclusion, Roche emphasized that the foamer device is the first automated foam-preparation device for use in the treatment of varicose veins with sclerotherapy. Now, the final product has been designed, but technical and clinical validation as well as regulatory approval has to be completed.
VBAS (V Block Assisted Sclerotherapy) V-block™ procedure
Elias presented a new nonthermal and nontumescent endovenous ablation technique called V Block Assisted Sclerotherapy (VBAS). The procedure consists of a percutaneous delivery of a vascular occluding device (V Block Device) into the proximal great saphenous vein and concomitant liquid sclerotherapy of the vein using a proprietary dual procedure syringe system. The technique has the following advantages: office-based technique, no tumescent agent required, no hardware down payment, and no sclerosant-related major complications.
Why we need youth, courage, and innovations in phlebology
Ragg presented his vision to improve phlebology, namely to do more than ablation and compression, to fascinate young people, to admit to knowing almost nothing, to employ the best, and to be courageous. Next, the speaker described four causes of venous insufficiency: (i) congenital valve defects, (ii) acquisition by valve degeneration, (iii) acquisition by valve zone dilatation, and (iv) secondary causes, such as phlebitis and thrombosis. All of these causes lead to consecutive local overload and progradient valve incompetence. The speaker reported the results of a Berlin pilot kids study (n=63) in which 42% showed at least one valve lesion with reflux. High-resolution B-flow showed different grades of stasis: limitation of cusp movements by aggregates and hemodynamic disturbance of valve function. Then, the speaker presented another pilot study, which showed that newly started physical training and compression stockings were able to reduce aggregates in 81% of the evaluated patients. He pointed out that minimal disease deserves attention because it offers the opportunity of control, treatment, and prevention. In conclusion, Ragg emphasized that phlebology needs an update and requires youth and courage. He also believes that the early stages of the pathology have to be recognized as disease, prevention strategies have to be developed, and gentle vein repair should replace mere destruction.
Surgical and endoluminal neovalve
Lugli explained that the purpose of deep venous valve repair or creation is to correct deep vein reflux. Deep vein reflux can be classified by etiology, such as primary, secondary, or as valve agenesis. The speaker presented internal valvuloplasty as the best option in case of primary reflux. In secondary deep venous incompetence, valve cusps are usually destroyed and when a direct valve repair is not possible, alternative techniques are available, including transposition, neovalve creation, and valve transplantation. Valve reconstruction is a great opportunity for patients presenting with deep vein reflux.
Compression Therapy
Challenging dogmas in compression therapy
In May 2011, the International Compression Club (ICC) met in Brussels during the European Wound Management Association (EWMA) annual conference. Almost 50 members challenged a series of dogma’s and myths that exist when considering compression therapies. Mosti reported on a number of the issues and dogmas that were discussed. He confuted a number of dogmas, such as that concerning the assumption that compression pressure depends on the material. Indeed, compression pressure does not depend on the bandage and it can be extremely variable, depending on the health care provider (tension applied and turns overlapping). Another false dogma is that inelastic material can become ineffective after some days due to pressure loss. Indeed, several studies showed that stiff material maintains its effectiveness over time despite pressure loss. Furthermore, it seems untrue that lymphedema treatment requires strong to very strong pressure. New trials measuring edema reduction in relationship to the exerted pressure of compression products have indicated that there is obviously an upper pressure limit beyond which further increases in pressure seem counterproductive. This upper limit is around 30 to 40 mm Hg of initial pressure exerted by inelastic bandages on the arm and around 50 to 60 mm Hg on the lower extremity. The explanation for these findings may be based on a different threshold of efficacy of compression on the two main mechanisms of edema reduction, ie, the reduction in capillary filtration and an improvement in lymphatic drainage. In clinical practice, comfort and ease of application, which have decisive importance for compliance, will also favor lower compression pressure. Finally, the statement that compression is contraindicated in arterial impairment was debated. Indeed, if compression stockings are used, care should be taken to adjust the chosen compression class to the distal systolic pressure. Therefore, by knowing the distal systolic pressure in mm Hg and knowing the exerted pressure of the medical compression stockings in mm Hg, readymade medical compression stockings can be prescribed for patients with direct oral anticoagulants if the systolic ankle pressure is higher than 60 mm Hg. In patients with a perfusion pressure ≥60 mm Hg, compression with inelastic bandages exerting a pressure ≤40 mm Hg does not lead to a measurable reduction, but seems to increase the arterial inflow and improve venous pumping function significantly. Intermittent pneumatic compression (IPC) may be an excellent indication for treating ischemic disease of the extremities. Many products are on the market, providing different sequences of pressure that need to be validated concerning optimal performance in different clinical indications, which is especially important for pumps that were not specifically designed for the indication of arterial occlusive disease, but rather for prophylaxis of deep vein thrombosis and for the treatment of lymphedema. In conclusion, compression pressure and outcomes of compression therapy should be measured. The dose/response correlation between compression pressure and outcomes should always be assessed. Many dogmas must be critically reevaluated with a more scientific approach to compression therapy.
Comparison among different compression values in lower limb volume and perceived exertion control during intermittent walking
The speaker reported the effects of a comparison between 18 mm Hg and 23 mm Hg elastic stockings on leg volume and tiredness after golf. A leg volume increase was reported along an 18-hole competition in the absence of stockings. In the 18- and 23-mm Hg groups, only the latter demonstrated a significant reduction in leg volume and perceived fatigue. A second feasibility study: increasing public health awareness, physical activity, and medical check-up participation through open events on golf courses was discussed.
Influence of medical compression stockings on the skin moisture in patients with chronic venous disease
Westphal explained that medical compression stockings (MCS) damage the shield of moisture and lipids, reducing skin hydration and increasing skin roughness and desquamation. The presented study was designed as a randomized controlled trial with parallel groups and one-sided blinding. Patients with chronic venous disease with stages C1 to C5 were included. The primary end point was skin moisture and the secondary end points were skin roughness, leg volume of the lower limb, and interface pressure. Patients were randomized to wear below-knee stockings VenoTrain®cocoon (MCS with integrated skin care) or VenoTrain®micro (conventional MCS). Patients were wearing MCS for 8 hours a day for 28 days and they were examined at screening, after 1 day, and after 28 days from inclusion. Leg volume was measured using Bodytronic 600®, contact pressure using PicoPress®, skin moisture using Cutometer®, and skin roughness using FOITS®. Changes in skin roughness, pressure, and leg volume did not differ significantly between groups at the end of the study. The speaker highlighted the question of which patients benefit from MSC with integrated skin care VenoTrain®cocoon. A subanalysis showed that changes in skin moisture were sexspecific and skin moisture in male subjects wearing VenoTrain®cocoon increased. Another observation was that changes in skin moisture were under the influence of the clinical, etiological, anatomical, pathophysiological (CEAP) classification. Subjects with low skin moisture wearing VenoTrain®cocoon showed a higher increase in skin moisture compared with VenoTrain®micro. Westphal concluded that C3 subjects, subjects with dry skin, and male subjects benefited particularly from VenoTrain®cocoon.
Interface pressure, clinical efficacy, and hemodynamic effects of two compression stockings in healthy volunteers and in patients with chronic venous insufficiency
Konschake presented a study in which 32 patients with chronic venous insufficiency (CVI; clinical, etiological, anatomical, pathophysiological [CEAP] classification C3 and C4) and 32 healthy volunteers wore graduated elastic compression stockings (GECS) or inverse graduated elastic compression stockings (PECS) for 1 week, followed by a break of 1 week, and wearing a second stocking for another week. Outcome parameters were volume changes, interface pressure, hemodynamics of the leg, and wear comfort. There were no significant differences between the stockings in all parameters measured. No significant difference in sweating, skin dryness, and other adverse effects has been observed between the stockings. The speaker concluded that both compression stockings induced a volume reduction on the lower leg and improved venous hemodynamics. GECS showed a more pronounced volume reduction on the foot compared with PECS. Although not statistically significant, advantages in wearing comfort with PECS could be observed.
Novel medical compression stockings for patients with chronic venous insufficiency and concomitant PAD
Dörler presented a prospective, noncontrolled study on 20 patients with chronic venous insufficiency (CVI; clinical, etiological, anatomical, pathophysiological [CEAP] C3 to C5) and an ankle brachial index <0.9. The aims of the study were to investigate the safety, efficacy, and handling of the compression stockings VenooTrain®angioflow after 2 weeks of treatment. The stockings are characterized by moderate compression and high stiffness. At the end of the study, there was no significant difference in leg volume compared with baseline. The stockings significantly reduced edema, but did not show any significant effect on pain. The speaker summarized that treatment of chronic venous insufficiency with concomitant peripheral arterial disease with moderate compression stockings with high stiffness is safe. Efficacy and quality of life should be evaluated in further studies.
Elastic compression elicited beneficial cardiovascular effects: a complex clinical study in healthy, lymphedematous, and lipedematous individuals
The speaker explained left ventricular rotation and twist of the heart in normal situations. The experimental procedure on patients with lymphedema and lipedema consisted of 2D echocardiography and 3D echocardiography at baseline and 60 minutes postapplication of flat knitted panty hose (23 to 32 mm Hg). The experimental procedure on healthy volunteers consisted of 2D echocardiography and 3D echocardiography at baseline, after a 9-minute treadmill exercise, and after 60 minutes of wearlag 15- to 20- mm Hg sport socks followed by a 9-minute treadmill exercise in socks. The results of the study showed clearly that lymphedema and lipedema are distinguishable on left ventricular function parameters. Elastic compression showed beneficial effects on left ventricular rotation in lipedema and did not hamper left ventricular rotation in lymphedema. Minor beneficial effects might be attributed to sport socks.
Skin sonography in swollen legs: basic findings and effects of compression
Chronic venous edema is based upon visual inspection, different types of measurements, and finally, palpation. As examples, Caggiati mentioned tape measurement, water displacement, ortoelectronic volume estimate, leg volume measurement, and bioimpedance. The speaker summarized that characterization of chronic venous edema is currently based on a quantitative analysis, such as measurement of leg circumference, volume, and water content, as well on a qualitative analysis, such as resistance to compression and skin pinching. Caggiati uses sonography to refine data obtained by clinical inspection. This method uses the same investigation instrument during the same session, is not expensive, not dangerous, and not time consuming. Subsequently, the speaker explained his technique, which he has been using for a few years. The patient lies in the supine position and a large amount of gel is mandatory to avoid any contact between the probe and the skin. Caggiaty emphasized that skin sonography refines measurements and furnishes morphological information of skin tissues not available by clinical inspection. In dermal edema, the normal subepidermal low echogenic band (SLEB) appears anechoic and thickened and the whole dermis shows hypoechogenicity and rarefaction. In case of scleroderma, sonography demonstrates different patterns: diffuse soaking, anechoic lacunae, or a combination of both. By preparing a “squeezing” test, the compliance of compression can be evaluated. At the end, the speaker summarized that performance of skin ultrasound is easy and it allows the documentation of changes not visible with the naked eye and not demonstrated by palpation. In his opinion, the pathophysiology of these changes, their prognostic significance, and therapeutic implications need to be further investigated.
New awareness for compression postintervention
Lattimer presented the old awareness of compression: prevention of bruising, hematoma, and reduction in leg edema and postoperative inflammation. The new aims are to keep the target vein compressed/closed to induce sclerosis and to prevent sclerothrombosis, which is responsible for pigmentation, recanalization, and recurrence. There are different compression types: concentric (MSC), eccentric (dental swab), tangential (tape), and perivenous (tumescence). In concentric compression, pressure of more than 80 mm Hg is required to occlude the venous return. Eccentric compression is complicated to apply and not very comfortable. Tangential compression works by lateral collapse (steristrip principle), absolute pressure collapse (direct pressure principle), or ovalization (±volume reduction). The speaker reported on a clinical study of 28 patients with bulging varicose veins. Horizontal/vertical diameter and depth of the veins were assessed with and without tape by ultrasound. The results showed ovalization of the veins, area reduction, and increase in depth. The speaker concluded that adhesive skin tape for bulging varicose veins is simple, inexpensive, available, and easy to use. It does not compress the target vein, and it submerges and protects the vein from the skin. Such compression techniques may reduce the incidence of skin pigmentation, inflammation, and pain after sclerotherapy. A kind of perivenous compression with hyaluronic acid was presented. A recently published study on foam sclerotherapy of segments of the saphenous vein with adjuvant hyaluronan compression was discussed by the speaker. Lattimer stressed that, in the NICE clinical guidelines, compression is recommended for no longer than 7 days after interventional treatment. He pointed out the clinical evidence for medical compression stockings and compression bandages, namely to heal venous ulcers, to soften dermatoliposclerosis, to reduce pigmentation, and to provide comfort. The hemodynamic evidence is volume reduction, tone increase and reduction of reflux. At the end of his presentation, Lattimer concluded that chronic venous disease is a disease for life and an intervention is only part of the treatment for many patients.
Controversies in compression – no myths, just physics
Ragg began his lecture with the publication of Partsch about unexpected venous diameter reduction by compression stockings of deep, but not of superficial veins. The speaker emphasized that external concentric compression causes a general increase in tissue pressure, a decrease in the transmural gradient, and a reduction in the fluid load/edema. He discussed ways to develop venous insufficiency: congenital valve defects and acquisition by valve degeneration secondary to thrombosis. All of these processes lead to consecutive local overload and progressive valve incompetence. Congenital valve damage can be caused by missing valves, missing cusps or cusp defects. Ragg reported on case studies in kids aged between 8 and 12 years. All cases with visibly enlarged superficial vein segments had associated reflux. Another pilot study on kids between 6 and 18 years showed at least one valve lesion with reflux. The speaker could not answer the question “Should children wear compression stockings?,” but stressed that high-resolution ultrasound of minor congenital or early vein pathology seems to be relevant for at least 25% of children. Concerning acquired insufficiency by valve degeneration, Ragg described different grades of stasis shown by high-resolution ultrasound. Limitation of cusp movements by aggregates and hemodynamic disturbance of valve sinus function can cause potential cellular interaction. Stationary aggregates are a marker of stasis and vein disease and therefore may be suitable for the follow-up of vein treatments and prevention. The speaker presented pilot studies in which newly started physical training and compression reduced aggregates in 81% of the evaluated valves. In his opinion, even minimal disease deserves attention because it offers the options of control, treatment, and prevention.
Mild compression with a diabetic foot: conflict or opportunity?
The prevalence of diabetes is rapidly growing in the Western world (the estimated prevalence will more than double between 2000 and 2030; in the western population region, it is projected to be 183 million in 2045). One of the most serious diabetes-related complications for those affected is the diabetic foot syndrome, often leading to lengthy and costly treatments and a significant reduction in quality of life, even loss of independence. Lower extremity edema is often an early sign of significant fluid retention that can result in cardiac overload and conditions, such as heart failure, and is a common clinical finding in patients with diabetes. Patients with type 2 diabetes have a higher prevalence of peripheral edema than healthy subjects. In a prospective study of 314 patients with diabetic foot ulcers, 38% presented with lower extremity edema. The presence of lower extremity edema is an indicator of poorer prognosis; peripheral edema presented more commonly in patients who required amputation (58%) or who died (55%). Patients with diabetes have a 2 to 5 times greater risk of developing peripheral arterial disease (PAD) vs those without diabetes. Compression therapy has long been considered a risky practice in patients with diabetes due to the fear of compromising vascularity. Prior to treating lower extremity edema, a thorough history and physical examination must be performed to address any potential underlying pathology. Once systemic pathology has been managed or ruled out, peripheral edema is mainly treated with graduated compression therapy. However, compression therapy is generally avoided for fear of compromising arterial circulation. Usually diabetic patients do not receive compression therapy; they are often purposefully denied the treatment. Many patients suffer from concomitant diseases, which are often regarded as contraindications for compression: severe peripheral neuropathy with wounds, PAD with an ankle brachial index <0.6, an ulcerations and the foot.
Recent evidence and future prospects
There is an International Compression Club (ICC) consensus statement (2008) on the use of compression therapy in the management of venous and lymphatic diseases; there are several gaps in the available evidence. A working committee was developed to fill the gaps identified in the earlier consensus treatment and to provide graded recommendations for the clinical goals of treatment using medical compression stockings (MCS). A literature search was performed on PubMed between the 2007 and 2015, and the included articles (n=109) were based on the following criteria: randomized controlled trials, observational human studies, use of compression stockings reported. Reviews were not evaluated and the duplicates were removed. As a result; 25 recommendations were proposed; 24 recommendations were graded: grade 1A (n=4), 1B (n=13), 1C (n=2), 2B (n=4), and 2C (n=1). The use of MCS for lymphedema maintenance therapy was upgraded from 1B to 1A and the use of MCS to improve venous leg ulcer healing was upgraded from 1B to 1A; whereas the use of MCS as early as possible after diagnosis of deep vein thrombosis to prevent postthrombotic syndrome was downgraded from 1A to 1B and the use of immediate compression to reduce pain and swelling, thereby allowing instant mobilization in patients with acute deep vein thrombosis was downgraded from 1A to 1B. In conclusion, MCS in the treatment of venous and lymphatic disease continue to be supported by evidence. In certain cases, such as moderate arterial occlusive disease with ankle pressure between 60 to 90 mm Hg, cardiac failure (if not well compensated), peripheral nerve lesions or polyneuropathy, and skin disease with massive exudation, it was recommended to decide on a case by case basis, according to a benefit-risk assessment, to use low-pressure compression and to use modified compression strategies. The absolute contraindications included severe arterial occlusive disease with ankle pressure below 60 mm Hg, arterial bypass (if the conduit or anastomosis would be compressed), phlegmasia coerula dolens, decompensated cardiac failure with severe edema, and a confirmed allergy to the stocking material.
Stiff compression: old but still effective
The amount of compression applied to an extremity is defined by the force of the compression applied to a certain area. Following the law of Laplace, the resulting compression pressure is directly proportional to the tension of the applied fabric and indirectly proportional to the radius of the limb. This means that the same force applied to a sharp curvature (low radius) will produce higher pressure than when applied over a slightly curved structure (large radius) and thus the pressure will be zero over a completely flat part of the leg, eg, the plane part of the shin. The resulting force of a single layer depends on the elastic property of the product and the applied stretch. The pressure exerted by inelastic material with no extensibility (eg, zinc paste) is created only by the strength exerted during application. Adding several layers increases the pressure. In order to overcome the main disadvantages of inelastic bandages, which require being applied by a trained staff member and can undergo a drop in pressure due to an immediate reduction in edema, a number of compression devices have been created in the last few years. Among them, self-adjustable Velcro devices, consisting of Velcro straps, can be applied and readjusted by the patients themselves and offer great advantages with regard to self-management. A good indication for Velcro-band devices is the patient who, after bandaging, cannot maintain positive effects by using hosiery or who is unable to put on and remove compression stockings. In addition, in the acute ulcer stage, such Velcro devices may be recommended for patients who prefer self-management. Besides these devices, pneumatic pumps can play a role in addition to sustained compression. Finally, hybrid devices, which are a combination of sustained and intermittent pneumatic compression (IPC), can also be used. In sustained mode, pneumatic pressure chambers compress the leg continuously to a preset pressure level (“adaptive compression therapy”). During sitting periods, the patient can switch to intermittent pressure and the leg can be massaged. Basically, IPC mimics the action of stiff bandages plus walking exercises. In addition to sustained compression by using bandages, IPC pumps may be beneficial, especially in patients with restricted mobility. The pumps can be applied over a bandage and should be used for at least 2 hours per day.
Effect of medical compression stockings on local inflammatory markers that are expressed in healthy volunteers and CVI patients during gravitational stress of prolonged standing
The hypothesis is that prolonged standing causes inflammation, leading to tissue damage. Compression stockings/leg elevation may offer recovery. This presentation demonstrated that gravitational positioning with local blood samples are proposed as a model for studying biomarkers of chronic venous insufficiency, annexin V and microparticle levels are reduced significantly with antigravitational positioning and compression, local metalloproteinases are reduced in response to antigravitational positioning and compression. These effects were observed to have a great effect in patients lying down. The hypothesis is that prolonged standing causes inflammation, leading to tissue damage. Compression stockings/leg elevation may offer recovery. This presentation demonstrated that gravitational positioning with local blood samples are proposed as a model for studying biomarkers of chronic venous insufficiency, annexin V and microparticle levels are reduced significantly with antigravitational positioning and compression, local metalloproteinases are reduced in response to antigravitational positioning and compression. These effects were observed to have a great effect in patients lying down.
Practical therapeutic concepts in compression: why Velcro devices?
Compression therapy is a key component in the effective management of people with lower limb problems associated with venous and lymphatic disorders. Individuals with lymphedema and venous ulceration often require long-term compression therapy to prevent and manage problems, such as chronic ulceration, skin changes, persistent swelling, and shape distortion. Challenges remain in achieving acceptable, safe, effective, and cost-efficient compression therapy choices. Compression devices should achieve a simultaneous improvement in hemodynamics, by reducing venous refluxes and promoting venous pump, and improvement in symptoms, by reducing edema and promoting lymphatic drainage and microcirculation. The static stiffness index may be defined as the difference in subbandage or wrap pressure from the lying to the standing position. A rise of 10 mm Hg or more is considered a good value to increase the flow of blood out of the leg. Stockings, however, show little or no increase in pressure when comparing the lying with the standing position, and these properties help explain why many patients with significant leg swelling are not helped by the stockings. Calf-length compression stockings with low ankle pressure and stiffness (range between 11 and 21 mm Hg) are able to reduce or totally prevent moderate evening edema and may therefore be recommended for people with a profession connected with long periods of sitting or standing. To improve hemodynamics in severe chronic venous insufficiency, higher stiffness is necessary. Inelastic bandages are usually recommended for the initial treatment phase. The disadvantages of inelastic bandages are that they lose pressure quickly following application and need to be reapplied by specialized staff. Adjustable compression wrap devices using hook and loop fasteners, commonly called Velcro brand fasteners, present opportunities for improving treatment outcomes, thereby supporting patient independence and self-management in the use of compression therapy. They have an indication in severe chronic venous insufficiency (venous leg ulcers) and in the initial phase of edema reduction (eg, lymphedema).
Evidenced-based compression with Velcro devices
Pannier presented the main results of four trials conducted using Velcro devices. In the randomized controlled trial performed by Mosti et al (Eur J Vasc Endovasc Surg. 2015;50(3):368-374), forty affected legs from 36 patients with untreated venous edema were randomized to receive inelastic bandages (n=20) or adjustable Velcro compression devices (AVCDs) (n=20). Both compression devices were left on the leg day and night, and were renewed after 1 day. Patients in the AVCD group were asked to readjust the device as needed when it felt loose. Leg volume was calculated using the truncated cone formula at baseline (T0), after 1 day (T1), and after day 7 (T7). The interface pressure of the two compression devices was measured by an air filled probe, and the static stiffness index calculated after applying compression at T0 and T1, and just before removal of compression on T1 and T7. At T1, the median percent volume reduction was 13% for the inelastic bandages group vs 19% for the AVCD group; at T7 it was 19% vs 26%, respectively (P<0.001). The pressure of the inelastic bandages was significantly higher compared with the AVCDs at T0 (63 vs 43 mm Hg), but dropped by >50% over time, while it remained unchanged with AVCDs due to the periodic readjustment by the patient. Comfort was similar with the two compression devices. In conclusion, readjustable AVCDs with a resting pressure of around 40 mm Hg resulted in a more effective reduction in chronic venous edema than inelastic bandages, with a resting pressure of around 60 mm Hg. AVCDs were effective and well tolerated, not only during maintenance therapy, but also in the initial decongestive treatment phase of patients with venous leg edema.
In the randomized controlled trial performed by Damstra RJ et al (J Vasc Surg Venous Lymphat Disord. 2013;1(1):13-19), 30 hospitalized patients with moderate to severe unilateral lymphedema (stages 2-3) were randomized to receive adjustable compression wraps (ACW) or received inelastic multicomponent compression (IMC) bandages. Classic water displacement volumetry was performed before compression and after 2 and 24 hours of compression. The interface pressure was measured immediately after application of compression, 2 hours after compression, before and after compression renewal, and finally, after 24 hours. Patients in the ACW group were allowed to adjust the wrap themselves when they considered it necessary. The reduction in median volume after 2 hours was 109 mL (interquartile range [IQR], 64-271 mL; -3.1%) in the ACW group and 75 mL (IQR, 41-135; -2.4%) in the IMC group (not significant). After 24 hours, the reduction in median volume was 339 mL (IQR, 231-493 mL; -10.3%) in the ACW group and 190 mL (IQR, 113-296 mL; -5.9%) in the IMC group (P<0.05). The interface pressure dropped significantly after 2 and 24 hours in the IMC group (-50% and -6%), but significantly less in the ACW group (-26% and -44%), mainly due to self-readjustment. The median pressures achieved after self-application of ACW (52 mm Hg; IQR, 44-61 mm Hg) were of the same order as those produced by the nurses after the first application of ACW (53 mm Hg; IQR, 39-59 mm Hg), with less variation. Thus, in patients with moderate to severe lymphedema of the legs, ACW achieved a significantly more pronounced reduction in volume after 24 hours than IMC bandages. Patients were able to apply and adjust the device after being instructed on its use and initially being worn for a 2-hour period.
Blecken SR et al (J Vasc Surg. 2005;42(6):1150-1155) compared a four-layer elastic bandage with a nonelastic garment (CircAid) in patients with bilateral venous leg ulcers (n=12). The 24 limbs were randomized to have a four-layer elastic bandage on 1 extremity and a nonelastic compression garment CircAid in the contralateral limb. Every 4 weeks, patients had the ulcer area measured in square centimeters by a computerized scanning method and had the limb girth measured in centimeters at the foot, ankle, and calf. Results were assessed at 12 weeks. Group A received CircAid and group B received a four-layer elastic bandage. The ulcer healing rate was significantly faster in group A vs group B (hazard ratio, 0.56; 95% CI, 0.33- 0.96; P=0.0173). Therefore, in compliant patients, venous leg ulcers randomized to nonelastic compression had a significantly faster healing rate per week than ulcers treated by the conventional four-layer compression system.
Finally, Mosti G and Partsch H (Vein Lymphatics. 2017;6(3):7003) investigated if patients are able to apply a Velcro-band compression device (Circaid Juxta Lite™) themselves with sufficient pressure. Thirty-one patients (clinical, etiological, anatomical, pathophysiological [CEAP] C6=23, C5=5, C3=2, mixed ulcer=1) applied Juxta Lite™ on their own legs after a short instruction and were asked to readjust the pressure according to their subjective feeling. Subbandage pressure was measured after application and 24 hours later. In 30 patients without arterial occlusive disease, the median subbandage pressure values on day 1 and day 2 were 44.5 mm Hg (interquartile range [IQR], 42-48) and 46 mm Hg (IQR, 44-48.25), respectively. One patient with an arterial-venous leg ulcer showed pressures of 34 and 36 mm Hg. All measured pressure values corresponded to the pursued target range, demonstrating that adequate self-application of Velcro bands is feasible and that patients can maintain this pressure by readjustment.
Self-management with new innovative Velcro device
Self-care management by trained relatives or inexpert wound care professionals for the right patients, with the appropriate training, may provide the solution to an increasing demand for care in a world of dwindling resources. This care is only possible with therapies that lend themselves to simple methods of use and the support from manufacturers to provide training, clear instructions, and on-going customer care. The Velcro adjustable compression wrap is a simple solution that has the potential to cut costs by reducing treatment times, facilitating self-care, and early resolution with transfer to hosiery for long-term care. More importantly, patient participation and comfort improve compliance and independence. Self-application and the adjustability of the garments provide the opportunity for patients to take control of their care, promoting independence and involvement. These characteristics suggest the value of this technology for elderly patients who may be able to participate in their own care or who may have nonmedical assistance. The financial implication of incorporating the device into a compression treatment regime cannot be overlooked. The role of the reviewed Velcro wrap to reduce clinic visits from three times a week to twice a week and then to once a week in some cases have cost implications for those patients with co-pays per visit, as well as for clinic efficiency where available appointments may be limited. Further studies to specifically document cost savings would be beneficial to justify the one-time cost of the Velcro wrap to the consumer as well as to commercial/government payers.
Velcro devices after varicose vein procedures
Noppeney discussed several randomized controlled trials published in the last few years comparing postoperative treatment with or without compression and suggesting the beneficial effect of compression therapy after invasive vein procedures. The common rationale for compression after ablation of varicose veins is the reduction in side effects, such as hematomas or pain (after surgery, laser, or radiofrequency ablation), the prevention of deep vein thrombosis or hyperpigmentation, superficial thrombosis or matting, and the anti-inflammatory or anti-edema effect. However, as suggested by Partsch’s studies, stiff, nonyielding material applied with adequate pressure provides hemodynamically superior effects compared with elastic material and that relatively low pressure reduces edema. Compression over the calf is more important to increase the calf pump function compared with graduated compression. However, successful treatment with compression bandaging requires knowledge of the appropriate materials and the ability to employ them. A study investigating 891 German health care providers for their knowledge of bandage materials and their practical ability in applying short-stretch compression bandages, showed that compression material and its application are unfamiliar to most practice employees (Protz K et al. J Dtsch Dermatol Ges. 2014;12(9):794-801). On the other hand, early results in a small German audit demonstrate that an adjustable Velcro compression wrap may provide a simple, clinically effective, and patient-acceptable solution for self-care with compression. Use of this type of device could potentially reduce overall health care burden by reducing necessary skilled treatment visits and/or cost while still achieving good clinical outcomes. Noppeney concluded that a multicenter trial is required to test the hypothesis that inelastic fabrics are superior to short-stretch bandages and stockings and to provide additional data after varicose vein ablation procedures for treating great saphenous vein reflux. Patients treated with open surgery, radiofrequency ablation, and endovenous laser treatment could be included. Measurement hematoma extension, pain scores, side effects, venous clinical severity score, and quality of life 7 days before and 7 and 30 days after the procedure should be assessed.
Patient-oriented concepts in the treatment of chronic venous insufficien
Compression hosiery comes in a multitude of shapes, sizes, and classification testing standards, such as British standard, German Institute for Quality Assurance and Certification, and French national standard organization. When prescribing compression hosiery, health care providers should take into consideration the amount of compression they wish to achieve for the patient, regardless of classification, making the right choice for every patient and avoiding potential prescribing errors. However, recommendations regarding the class of compression are lacking in most clinical guidelines. The Mediven observational study demonstrated that outpatient prescription of medical compression stockings (MCS) is not sufficiently guided by the medical needs of venous patients. In a follow-up analysis, the authors therefore evaluated the frequency of prescriptions of MCS and donning aids. Moreover, they asked whether MCS are differentially prescribed according to the patients’ clinical, etiological, anatomical, pathophysiological (CEAP) classification and body mass index (BMI). Approximately one-third of patients did not receive a prescription for a second pair of MCS at the beginning of the study and approximately one-third of patients were not given a 6-month repeat prescription. Moreover, donning aids were only rarely prescribed. These factors had an impact on compliance, since high MCS wearing frequencies were associated with both frequent MCS represcriptions and, at least for patients aged 61 years or above, prescription of donning aids. Prescribed MCS were mostly of light quality, irrespective of the patient’s CEAP classification and BMI. Importantly, improvements in the CEAP classification of patients in category C3 occurred more frequently with medium and firm MCS qualities (BMI >25: 30.9%; BMI <25: 41.7%) than with light MCS qualities (BMI >25: 22.4%; BMI <25: 13.3%). In obese patients, constriction furrows occurred less frequently when medium or firm MCS qualities were used. Thus, concerning the number and type of MCS prescriptions, there is still significant need for improvement. If required by the patients’ medical needs, medium, and firm MCS qualities should be considered to a much greater extent.
Leg Ulcers
Leg ulcers and wound care: basics
Gogia defined edema as excessive tissue fluid with dynamic egress of fluid from blood and ingress into the lymphatic system. Return of fluid occurs up to 90% through the venous system and up to 10% through the lymphatic system; 80% of lymphatic system is in a subcutaneous plane. The lymphatic system takes out the dead cells, protein, bacteria, and helps with disposal. Lymphedema is a vicious cycle, with an imbalance between demand and flow. However, lymphedema is also continuing inflammation. Chronic ulcers have a venous as well as a lymphatic component. Gogia pointed out that edema and ulcers feed each other. He presented results from Sanwari Bai Surgical Centre Lymphedema clinic on the treatment of 668 patients with lymphedema. The basic principles of wound and ulcer care are, in the opinion of the speaker, reduction in the edema, removal of the debris, and epithelization. In conclusion, Gogia emphasized that it is important to treat edema as part of the treatment for an ulcer. Although pathophysiological interpretations and indications of ulcer management is still under dispute, positive clinical effects of compression are indisputable. Patients report improvements in pain, mobility, and general quality of life, in addition to ulcer healing.
Advancements in local therapy: ulcer debridement
Mosti introduced ulcer debridement as an essential step to promote the wound bed preparation of a nonhealing ulcer during the chronic, inflammatory stage. The aim of debridement is to convert the molecular and cellular environment of a chronic wound to that of an acute healing wound. The guidelines recommend that venous leg ulcers receive a thorough debridement at their initial evaluation to remove obvious necrotic tissue, excessive bacterial burden, and cellular burden of dead and senescent cells (grade 1B). The speaker pointed out that debridement is one of the key steps in wound bed preparation that is based on the principles of TIME: T (tissue) means that infected or necrotic tissue must be removed to promote a healthy granulation tissue; I (infection) means that reduction in the bacterial burden is crucial; M (moisture) means that moisture needs to be controlled; and E (epidermal migration) means that it must be favored for a successful outcome. Then, the speaker presented all debridement modalities. For example, an autolytic debridement is performed using a moist wound dressing. Mechanical debridement can be performed using a wet-to-dry method, negative pressure wound therapy, ultrasounds, wound irrigation, and wound vacuum cleaning. Enzymatic debridement uses enzymatic ointment, biological debridement uses larvae and sharp surgical debridement uses scalpels, scissors, curette, shaver, and hydrosurgery. The choise of debridement depends on the wound appearance, the health care professional’s ability/license, the patient’s general condition, the available technology, and the setting for inpatients or outpatients. Mosti stressed that no method of debridement is superior to surgical methods. In conclusion, the speaker emphasized that debridement is a mandatory step in ulcer treatment and can be performed with different methods. Surgical/hydrosurgical debridement is the best treatment modality in case of large and infected ulcers, particularly before surgical repair. Autolytic and mechanical debridement are optimal options for smaller ulcers to be treated in an outpatient setting. Well-educated health care personnel are necessary to select the best option and to perform the chosen solution.
How to increase patient compliance?
Morisson listed the indications for compression: prevention of deep vein thrombosis, prevention of progression or exacerbation of venous conditions, prevention of postthrombotic syndrome, varicose veins, and chronic venous insufficiency, including venous ulceration, edema, postsclerotherapy, and postsurgery. We have level A recommendations with clear benefit for compression therapy in active venous ulceration, prevention of postthrombotic syndrome after deep vein thrombosis, prevention of thromboembolic events after surgery when combined with anticoagulant prophylaxis, reduction in edema and inflammation, and a better cosmetic outcome. Morrison provided suggestions for increasing patient compliance in hot environments: compression hose choices, lighter weight and color, open-toe, calf or thigh-high stockings rather than panty hose. The speaker discussed the conservative treatment of chronic venous disease, such as weight loss, leg elevation, increased exercise/ ambulation, herbal medications, the graduated compression stockings. Compression therapy helps prevent thromboembolisms in nonambulatory hospitalized patients by improving venous return from the lower extremities with venous stasis. Compression counters the effects of ambulatory venous hypertension, helps control the progression of venous and lymphatic diseases, and reduces and controls edema and inflammation. Next, Morrison explained the compression levels and the long-stretch and short stretch garments. Choosing the compression modality depends on the age of the patient. She pointed out that the stiffness of compression products plays a major role for their hemodynamic efficacy. Stockings with a higher stiffness have a higher antiedematous efficacy. The speaker summarized that compliance can be improved with competence. Techniques of donning and doffing the stocking and different compression modalities can enhance patient compliance and treatment outcomes.
Preventing recurrence of venous leg ulcers
Up to 70% of venous leg ulcers recur after healing, with the highest rates being within 3 months. Many live with recurring ulcers for decades. Health care services available after healing are few and fragmented. Evidence shows that compression is better than no compression and high-level compression is better than moderate level compression, even though adherence is an issue. On the contrary, the level of evidence on preventive treatments is low concerning calf muscle exercise, leg elevation, and regular follow-up care. To prevent recurrence, research should concentrate on identifying target areas, early detection of risk, treatments, and models of care. Many studies identified factors associated with recurrence, namely past deep vein thrombosis, multiple previous ulcers, and longer ulcer duration. Early detection can be promoted by the development of risk assessment tools, reliability testing, validation studies, and Apps. Currently, 8-item risk assessment tools are available with a web-based app. Finlayson presented results from the VIP study (Venous Insufficiency Program of Leg exercise and/or elevation), where patients were randomized to three groups: (i) calf muscle exercise program + 1 hour/day leg elevation + compression; (ii) 1 hour/day leg elevation + compression; and (iii) routine care. The mean time to recurrence was 44 weeks in the first group, 38 weeks in the second, and 33 weeks in the third. The speaker proposed three models of care: Best Food Forward Program, Champions for Skin Integrity, and Leg Club Model.
Improving adherence to clinical practice guidelines: learning from the venous leg ulcer example
Worldwide, 1.5 to 3.0 people out of 1000 have active leg ulcers. The prevalence is increasing with age: 20 in 1000 people >80 years old have active leg ulcers. Aging populations, health care demands, and the cost burden continue to grow. Best practice showed that compression increases ulcer healing vs no compression. A multicomponent bandage is more effective than a single-component bandage, and a multicomponent system with elastic bandages is more effective than with inelastic bandages. There is no agreement or clarity on the optimal level of compression. The speaker emphasized that there is a failure to translate research findings into clinical practice, meaning that 30% to 40% of patients do not get treatments that have a proven effectiveness and 20% to 25% of patients get care that is not needed or potentially harmful. Identified barriers are structural, organizational, health care professional, patient-related, and professional-patient interactions. Barriers to guideline implementation are lack of reimbursement (84%), lack of time (51%), and contradictory recommendations published by different societies (54%). Another trial showed knowledge gaps, communication, time management, and individual case problems as barriers to guideline adherence. Weller highlighted that healing was 2 times more likely if the clinical practice guidelines are followed. Guideline implementation lowered costs and improved assessment, diagnosis, and the time to healing. The speaker emphasized that, to improve adherence to clinical practice guidelines, they must be implemented in context, be incorporated into the training of health care professionals, be used in a collaborative environment, and involve the patient. In Weller’s opinion, further research needs to identify which interventions overcome barriers to enhance enablers and how clinical behavior can be changed measured, and understood better. At present, there is no individual approach for translating evidence to practice that is superior in all situations.
10 years of experience in venous ulcer treatment: the view from a surgeon
The prevalence of venous ulcers is 1% to 2%, the cost is 0.5% to 1% of the national health care budget, and the recurrence is 30% to 60% within 1 year. The pathophysiology is the result of venous hypertension and pressure-related damage to the skin microcirculation. Wittens recommended treating both superficial incompetence and incompetent perforating veins due to the low rate of recurrence rate after treatment. He reported the results of the 10-year Dutch SEPS trial (Subfascial Endoscopic Perforator Surgery) that showed 12% of patients were ulcer free after adequate perforating vein treatment vs 71% without treatment. Deep venous obstruction should also be treated because of the improved rates of healing and the reduced rates of recurrence. The results of treating deep venous incompetence are poor in the long term, but, if valve reconstruction is successful, it will improve healing and decrease recurrence. In conclusion, venous ulcers that do not heal within 4 weeks need to be referred to a dedicated center, and the underlying causes need to be treated promptly.
New therapy concept in the treatment of leg ulcers
In recent years, various acronyms relating to the topical treatment of chronic wounds have been introduced. In 2003, the TIME concept gained the widest acceptance internationally. However, over the past years, a number of new aspects and therapeutic options have emerged. On behalf of “Wund-D.A.CH.,” the umbrella organization of the various wound care societies in German-speaking countries, an interdisciplinary and interprofessional expert panel suggested refining the TIME concept for the classification of topical chronic wound treatment to include novel therapeutic options. The factors of the TIME concept designated by “T” (tissue), “I” (infection), and “M” (moisture) still apply and remain important; therefore, they were included with slight modificaitons in the new MOIST concept. The letter “E” of the TIME concept originally stood for epidermis and subsequently for edge (wound margins), comprising very different concepts aimed at wound bed preparation and promotion of reepithelialization, such as debridement, skin grafts, and biological wound therapies. In the MOIST concept, “E” has now been replaced by the letters “O” for oxygen balance and “S” for support as this allows for the inclusion of new treatment options for targeted therapy in a much more differentiated approach. “M” means moisture balance, as it is essential to achieve equilibrium between too little and too much moisture in wounds. Accordingly, dry wounds require the addition of moisture, for example, hydrogels. Usually, however, there is an excess of moisture, thus requiring the use of wound products, such as super-absorbers. “O” indicates oxygen balance because hypoxia plays a key role in the pathophysiology of chronic wounds. Regarding topical treatments, there are therapeutic options available to restore oxygen balance. These adjuvant treatments include wound dressings or sprays as well as normobaric or hyperbaric oxygen therapy. “I” describes infection control. To prevent infections, eradicate multiresistant pathogens, or treat local infections, antiseptics, such as polyhexanide and octenidine or wound dressings with antimicrobial effects, containing silver, honey, or dialkyl carbamoylchloride, are commonly used for the topical treatment of chronic wounds. “S” means support. In the case of recalcitrant wounds, despite apparently adequate treatment, specific wound therapies may be used that actively affect the impaired wound healing process. Wound healing is achieved, for example, through a decrease in metalloproteinases, by lowering the pH, or by applying growth factors. Finally, “T” indicates tissue management. Tissue management describes all measures aimed at wound bed preparation, and primarily includes the various methods of debridement and wound cleansing, for example, with preserved solutions, such as hypochlorous acid. Subsequent wound preparation may also comprise drug-free wound dressings or physical measures, such as negative pressure, electricity, or ultrasound. Adjuvant use of these therapies has beneficial effects on debridement, wound cleansing, granulation, and reepithelialization. Thus, the MOIST concept is meant to assist physicians in systematically planning topical treatment of chronic wounds using the most recent scientific advances.
Two biomarkers that assess healing status of venous leg ulcers
Stacey presented the results of a study that examined a panel of biomarkers in healing and nonhealing chronic venous leg ulcers to determine whether a biomarker can accurately predict healing in these wounds. Wound area and wound fluid were collected in 42 patients weekly for 14 weeks. Wounds were classified as healing or nonhealing by using three consecutive weekly measurements; the middle time point of the three was classified as healing with decreasing wound sizes and as nonhealing with increasing sizes. Wound fluid from each week was then analyzed for a variety of biomarkers using multiplex enzyme-linked immune-absorbent assays. A total of 32 healing time points and 27 nonhealing time points in which wound fluid was available were included in the analysis. An independent t-test of biomarkers in healing and nonhealing wounds showed that 13 biomarkers were significantly different between healing and nonhealing wounds (P<0.1). These markers were then included in a multivariable regression model, in which two biomarkers (GM-CSF and MMP-13) were significantly different between healing and nonhealing wounds (P<0.01). Receiver operating curves and optimal cut-off points using the Youden J statistic were then used to determine the accuracy, sensitivity, and specificity of these biomarkers. GM-CSF demonstrated a 92% accuracy in discriminating between healing and nonhealing wounds, and its optimal cut-off value had a sensitivity of 96% and a specificity of 81%. MMP-13 held a 78% accuracy in discriminating between healing and nonhealing wounds, and the optimal cut-off demonstrated a sensitivity of 92% and a specificity of 61%. In the author’s opinion, future studies involving different centers and different wound types should be conducted and a point of care test for assessing the wound healing status should be developed.
Skin grafts
The quality of skin is only one part of successful ulcer treatment. The preparation of the wound bed is even more important. The first step should be the extensive removal of necrosis and fibrosis with a lot of capillary bleeding. There are several options for wound bed preparations. They can include growing of noninfected granulation tissue (dressing), additional preparation with negative pressure wound therapy (NPWT), layered shaving (suprafascial necrosectomy and fibrosectomy), crural fasciotomy, or ulcer excision (Homan procedure) or wound debridement with surgery, ultrasound, or water jet. The ulcer healing rate seems superior with ulcer shaving therapy and skin grafting than with granulation tissue or crural fasciotomy (80% vs 40% to 50%). In clinical practice, split-thickness skin graft (STSG) transplantation remains the gold standard for covering large skin defects. In a prospective, randomized clinical trial (Guogienė I et al. J Wound Care. 2018;27(1):5-13) including 84 patients who underwent STSG transplantation surgery for postburn, posttraumatic, or postoperative skin defects, patients were randomized to receive a skin graft of either 0.2 mm, 0.3 mm, or 0.4 mm thickness. The greatest mean epithelialization scores and highest rate of complete wound epithelialization were identified in the recipient and donor wounds of the 0.2 mm transplant group at all times points. When the recipient wound pain scores were evaluated, the greatest visual analog scale (VAS) values were found in the 0.2 mm transplant group. The opposite result was found for the donor wound, where the highest VAS scores were identified in the 0.4 mm transplant group. A thicker skin graft included a higher risk of transplantation failure, although it could be more stressing in daily life. In Hemanns’ opinion, a thickness of 0.3 mm should be preferred (Obermayer 0.2 mm).
A single-center, nonblinded, randomized controlled trial (Kazanavičius M et al. J Wound Care. 2017;26(6):281-291) aimed at identifying the most appropriate, most suitable, and most efficient dressing for STSG donor sites, comparing the wound healing rate, pain severity, and duration, as well as the dressing change frequency in four randomized patient groups. All patients were randomly allocated to four different donor site treatment groups: polyurethane (Mepilex), polyurethane with silicone membrane (Mepilex border), transparent, breathable film (Mepitel film), and cotton gauze dressings. The fastest healing time was demonstrated in patients in the transparent, breathable film group. In the modern dressing study groups, the pain was not as severe and the dressings were used for a shorter period. However, the pain was lightest and felt shortest in the transparent, breathable film dressing group. The modern dressing’s polyurethane and polyurethane with silicone membrane had to be changed more frequently than transparent, breathable film.
A Cochrane systematic review (Santema TB et al. Wound Repair Regen. 2016;24(4):737-744) that included 17 trials (1655 randomized participants) showed that skin substitutes can, in addition to standard care, increase the likelihood of achieving complete ulcer closure compared with standard care alone after 6 to 16 weeks (risk ratio, 1.55; 95% CI, 1.30-1.85) in the treatment of diabetic foot ulcers. However, effectiveness in the long term, including lower limb salvage and recurrence, is currently lacking and cost-effectiveness is unclear. In conclusion, to cover a defect of skin and damaged tissue after preparing the wound for transplantation is the main cornerstone in modern ulcer treatment. Skin grafting, especially performed as a Meshgraft, is the most frequent option. The procedure is simple without additional costs. The effectiveness is high and the long-term results are very good. The skin is the best protection for ulcer recurrence in daily life. To get a perfect result and safe skin transplantation, hospitalization is mandatory, since an ulcer history of 40 years cannot heal in 1 week.
Skin substitutes
Leg ulcers usually heal when properly treated with adequate dressing, compression therapy, and correct life style (physical activities, resting in supine position, avoiding prolonged standing or sitting positions). Autologous skin grafting is indicated in case of superficial ulcers without deep skin layer defects, size ≤200 cm2. Skin substitutes are preferred in the case of deep ulcers where deep skin layers must be reconstructed, size >200 cm2. Skin substitutes must be sterile, biocompatible, and biodegradable. They should persist for 3 to 4 weeks on the ulcer beds. Indeed, shorter contact would not allow for tissue integration, whereas longer contact could interfere with new host tissue formation. A short hospitalization, including surgical debridement and reconstructive ulcer surgery may aid the healing process. A tissue bank is generally required as only tissue banks can explant, treat, and store donor skin. Skin can be stored in cryopreservation at -80°C, by lyophilization, or in a highly concentrated glycerol solution. In case of inadequate treatment, nonconcordant patients, or complex ulcers (mixed, arterial, autoimmune diseases, etc), healing may not occur and leg ulcers may become long lasting, large, and deep. Skin substitutes are necessary since derma tissue, like many other tissues, is not able to regenerate and dermis deficiency encourages scar formation. Tissue engineering materials are easier to handle, can be stored for a longer period of time (up to 18 months), but are usually more expensive than donor skin. In a case series of 414 difficult-to-heal leg ulcers (with ulcers surface >100 cm2 and duration >1 year, involving dermal and subcutaneous layers and not showing healing tendency), selected from a larger series of more than 2000 patients, after sharp debridement, skin substitutes resulted in a very effective promotion of ulcer healing both directly or by a subsequent autograft. No significant unwanted effects were reported.
Tissue and mesenchymal stem cells
Regenerative medicine is the reconstitution of damaged tissue activating resident cells, or with cell transplantation. Mesenchymal stem cells (MSCs) are a promising source of adult progenitor cells for cellular therapy and have been demonstrated to differentiate into various mesenchymal cell lineages. They have a crucial and integral role in native wound healing by regulating immune response and inflammation. Increasing evidence has pointed out that MSCs may enhance wound healing and serve as a cell source for many tissue engineering applications, including bone regeneration, cartilage regeneration, myocardial regeneration, neurogenesis, inflammatory bowel diseases, diabetic foot ulcers, and venous leg ulcers. MSCs exist in many tissues, for example, bone marrow, umbilical cord, placenta, adipose tissue, oral mucosa, etc. Brambilla showed a liposuction technique used in his center for cell sampling, stating that they obtained good results with this technique at 4 weeks regardless of the etiology of the ulcer.
Abolishment of venous reflux
The skin region surrounding the medial malleolus usually drains into the great saphenous vein (GSV), while the area around the outer ankle drains into the small saphenous vein (SSV). Therefore, medial ulcers are mainly associated with an incompetent GSV and lateral ulcers with an incompetent SSV. Therapeutic intervention should be adjusted to the complex variations of venous anatomy, their functional pathology, and the exact origin of venous reflux localized by duplex ultrasound investigation. The author presented the results of duplex investigations performed in consecutive leg ulcer patients, all with venous reflux, in a 2-year period. A total of 169 patients (183 legs), with chronic venous leg ulcers (clinical, etiological, anatomical, pathophysiological [CEAP]: C6) were examined. Venous function was assessed with duplex ultrasound, and the cases were described using the advanced CEAP classification. Additionally, a “sourcing” technique was performed with duplex ultrasound investigation of the ulcer bed and the venous system under manual compression and release of the ulcer. The principle of “sourcing” is to follow venous reflux from the ulcer area to its proximal origin. The detected reflux routes were classified either as “axial” or “crossover”. A total of 20% of the patients with ulcers showed no clinically visible varicose veins; 103 patients had medial ulcers, 54 lateral ulcers, 21 medial and lateral, and 5 had gaiter ulcers. Of the medially located ulcers, 64 (35%) had reflux in the great saphenous vein (GSV), 28 (15%) showed reflux in the medial perforating veins (axial types), and 11 (6%) had reflux in the small saphenous vein (SSV; crossover type). Of the 54 patients presenting with lateral ulcers, 25 (14%) showed GSV incompetence (crossover type) and only 13 (7%) showed SSV incompetence (axial type). Sixteen patients showed refluxes penetrating from deep into lateral perforating veins. Crossover reflux routes were detected in 25 of 54 (46%) legs with lateral and in 11 of 103 (11%) legs with medial ulceration (χ2, 44.34; P<0.001). Therefore, in patients with venous ulcers, an extended examination (CEAP classification) and a special duplex technique (“sourcing”) are useful in identifying the specific route responsible for the venous reflux, which seems essential for planning a rational treatment of venous reflux ulcers.
Velcro devices in leg ulcers
Venous hypertension is the first pathophysiologic factor in venous ulcers. Consequently, the most effective compression modality will be the most effective in reducing venous hypertension. Only inelastic compression can counteract ambulatory venous hypertension. Inelastic material, exerting higher working pressure and working peaks to close the vein, is significantly more effective in decreasing venous reflux, in increasing venous pumping function, and in reducing ambulatory venous hypertension when compared with elastic material. Mosti presented the preliminary results of an ongoing MIRACLE trial (Multicenter Italian Randomized Clinical Experience). The main aims of this randomized controlled trial are to prove the feasibility of self-management and assess the cost-effectiveness of the Adjustable Velcro Compression Devices (Circaid, Juxta Cure) in leg ulcer treatment. The primary outcomes are the evaluation of costs in terms of material and dressing time, self-management of compression devices, and ulcer area change. The secondary outcomes are healing rate after 16 weeks and healing time. The trial should enroll 60 patients (10 per center): 30 patients will be treated with CircAid Juxta Cure and 30 patients with Cobain 2. Patients of both sexes (age 20-85) suffering from venous ulcers with a wound size from 5 to 100 cm2 persisting for at least 3 months and with minimal arterial impairment (ABI ≥0.8) can be enrolled. For both groups, dressing consists of ulcer debridement, hydrofiber dressing, and Cadexomer powder in case of critically colonized or infected wounds. Up to now, 138 dressing changes in 19 patients treated with CircAid vs 144 dressing changes in 17 patients treated with Coban 2L have been needed. CircAid Juxta Cure has a distinct advantage over Cobain 2, with an average cost per patient of 150€ vs 255€. In conclusion, inelastic material exerting strong pressure, pressure peaks, and the so-called massaging effect provides a significant improvement in the impaired venous hemodynamics. Currently, inelastic compression (bandages, AVCD exerting strong/very strong pressure and high-pressure peaks) is the most effective compression modality in ulcer treatment. Inelastic bandages are very effective, despite significant pressure loss, but they need expert personnel to apply them. AVCD (CircAid) can be safely used in ulcer treatment. Compared with inelastic bandages, it seems to increase the healing rate and shorten the healing time, ensuring cost savings with negligible side effects. AVCD (CircAid) does not require expert personnel to apply them. After a short instruction, it may be self-applied and readjusted to maintain a consistent hemodynamic effectiveness (maintenance of pressure range), which provides further cost savings due to the reduction in professional health care support, since material is just one part of the total cost of treatment and is probably the least expensive one when compared with costs for nurses and doctors.
Vascular Anomalies
Development of knowledge on vascular anomalies through history: main contributors in the last decades
During his talk, Raul Mattassi reviewed some important historical milestones in vascular malformations. In the past, as far back as ancient times, vascular malformations were observed, but poorly understood. This changed in the 1500’s when Guido Guidi, a Florentine doctor and the personal physician of King Francis I of France, described the case of a fellow Florentine by the name of Alessandro Boscollo. The man was afflicted with, as Guidi described, “scalp arteries and veins as dilated as enormous varices; furthermore, those vessels were vigorously pulsating.” He referred the case to the famous surgeon Gabriele Falloppio who refused to operate on such a difficult case, mainly because not much was known about the circulation. The Galen theory of the vascular system was the only one accepted so blood circulation was ignored. A revolution in knowledge came in 1628 when William Harvey discovered blood circulation, providing the basis for the understanding of abnormal circulation and arteriovenous fistulas. Following Harvey, the description of vascular malformation was as follows.
In the 17th century, anatomists began to describe the arteriovenous fistulas. Leali Lealis first described a fistula between an artery and the spermatic vein, and JB Winslow (1669–1770), a Dutch anatomist, described fistulas between the esophageal artery and left pulmonary vein, the left bronchial artery and vein, and the left bronchial artery and azygos vein. In 1757, the Scottish anatomist William Hunter described typical signs of arteriovenous communications, such as the noise that disappeared when compressed. The 19th century brought us descriptions and drawings of several cases of arteriovenous fistulas as well as some attempts made in the treatment of such cases. In addition, there were more descriptions of venous anomalies and discussions about their classification. In 1817, Jean Louis Alibert, a French dermatologist, referred to vascular anomalies as “angioses’ and made the distinction between “hematoncus’ (vascular tumors) and “ecchymoma congeniale.” It was the Scottish surgeon John Bell (1763-1820) who coined the term “aneurysm by anastomosis,” to differentiate them from “nevi materni.” It was not until 1863 that an anatomopathological classification was created when Virchow referred to all vascular anomalies as “angioma” and divided them into the following types: simple angioma as a capillary form, cavernous angioma as vascular lakes, and racemous angioma, dilated, communicating vessels. In this same period, Franz von Pitha, an Austrian surgeon and professor of surgery in Vienna, wrote a famous book about surgery together with Theodore Billroth in which he described dysplastic dilated veins in the upper limbs.
In the second half of the 19th century, Carl Nicoladoni, who was born in Vienna and was a professor of surgery in Innsbruck and Graz, became famous for his innovative surgery, the first thumb transplant, was also the first to describe diffuse infiltrative arteriovenous malformations of the upper limbs. In 1869, he described the typical sign by compression of arteriovenous fistulas, the “Nicoladani – Branham sign.” Twenty years later, there was still quite a bit of controversy regarding whether or not arteriovenous malformations were congenital or not; for example, in 1889, Halsted reviewed 447 cases in the literature and reported that only 4 were congenital. On the other hand, his resident Rein off collected other cases and instead concluded that many were congenital.
At the turn of the century Maurice Klippel and Paul Trenaunay described cases with varicose veins, limb hypertrophy, and cutaneous nevi leading to the “triade” – Klippel-Trenaunay syndrome. There were no signs of arterial involvement (no arteriovenous defects), so they also looked at incomplete cases where only two of the signs were described. In the first two decades of the 20th century, Frederick Parkes Weber described cases of “hemangiectatic hypertrophy of limbs.” These cases were similar to Klippel-Trenaunay (with the “triade”), but with arteriovenous fistulae and were called “Parkes-Weber syndrome,”.
Born in Budapest, Geza de Takats moved to Chicago where he developed vascular surgery, where he made a clear distinction between arteriovenous malformations and other defects, such as venous malformations and venous “angiomas.” Soon after, Marceau Servelle and Fernando Martorell first described a venous infiltrating disease of the limbs with phleboliths and limb hypotrophy. It was roughly from this point on that rapid advances were made in the field. For example, Edmondo Malan, a professor of surgery in Milan carried out extensive studies on vascular malformations, 451 personal cases to be exact and then introduced a worldwide-accepted classification. Emerick Szilagyi, born in Hungary and who also moved to the United States and became the director of the surgical department of the Henry Ford Hospital of Detroit, was a famous vascular surgeon with research and innovative procedures in vascular surgery. In 1976, he published a case study about arteriovenous malformations treated surgically, but yielding poor results and concluded that “the large majority of patients do well on a carefully supervised conservative regimen.” More recently, Stefan Belov, a brilliant Bulgarian surgeon, worked alone on vascular malformations in his country and wrote a monograph based on 605 cases. Inspired by Malan, he thought about the possibility of improving classifications and proposed the “Hamburg Classification.” Belov was active in teaching in foreign situations, such as Hungary, Czechoslovakia, Germany, Italy, South Korea, and even Cuba; it was for this reason that he outlined the necessity to create multidisciplinary working groups.
Wayne Yakes, an interventional radiologist in Denver, CO, USA, introduced alcohol occlusion of vascular malformations and arteriovenous malformations by catheter and percutaneous puncture. He would later have a hand in founding the ISSVA. In 1992, he organized a workshop in Denver and it was there that the International Society for the Study of Vascular Anomalies was founded. Today, the ISSVA continues to grow and organizes workshops every 2 years. One of the first women to make an early contribution to vascular physiology and surgery was Emilie Holman, a professor of surgery at Sanford University. She is credited with the concise and brilliant unraveling of the mysteries of the arteriovenous fistula. John Mulliken organized a small meeting in Boston about vascular anomalies in 1976. These workshops continue today.
Back in 2008, Cristine Léaute-Labréze, a dermatologist in Bordeaux, France, discovered the positive effect of propranolol on hemangiomas, a revolutionary treatment. Another revolutionary figure is Mikka Vikkula, a Belgian Geneticist in Brussels, who did outstanding research in the genetics of vascular malformations and, along with his team, discovered several gene mutations. Judah Volkmann, a researcher in Boston whose main research was in angiogenetics, identified antiangiogentic factors against tumors that may be effective in vascular malformations. Korean born Bjung Boog Lee, a vascular surgeon in Washington D.C., has spent countless hours studying vascular malformations. He organized a vascular malformations clinic in Seoul, as well as the first international consensus on venous malformations for the International Union of Phlebology in 2009, later updated in 2013, and finally organized the first international consensus on arteriovenous malformations in 2012 for the International Union of Angiology.
Management of complex vascular anomalies
The updated classification of vascular anomalies made a distinction between vascular tumors and vascular malformations. Boon presented an example of a patient with PHACES syndrome, in which posterior fossa anomalies, plaque-like hemifacial hemangioma, aortic arch anomalies, cardiac anomalies, eye anomalies, and sternal cleft are presented. The patient was treated with a β-blocker, pulsed-dye laser, and rhinoplasty. As a second example, the speaker showed pictures of a patient with a complex venous malformation that required the involvement of a management radiologist, hematologist, gastroenterologist, pediatrician, psychologist, physiotherapist, and plastic and vascular surgeon. The third example given was the management of a patient with CLOVES syndrome (Congenital, Lipomatous, Overgrowth, Vascular malformations, Epidermal nevi, and Scoliosis). Boon described the management of a complex combined lymphatic venous malformation (CVLM) consisting of medical elastic compression, low-molecular-weight heparin, and antibiotics. He ended his presentation with the management of the embryonic vein of Servelle by surgical resection, endovascular radiofrequency ablation, and sclerotherapy with coils.
Management of complex vascular anomalies: the view from the International Society for the Study of Vascular Anomalies
Accurate diagnosis of vascular anomalies is crucial for appropriate evaluation and management, often requiring multidisciplinary specialists. Classification schemes provide a consistent terminology and serve as a guide for pathologists, clinicians, and researchers. One of the goals of the International Society for the Study of Vascular Anomalies (ISSVA) is to achieve a uniform classification. The last classification (1997) stratified vascular lesions into vascular malformations and proliferative vascular lesions (tumors). However, additional disease entities have since been identified that are complex and less easily classified by generic headings, such as capillary malformations, venous malformations, lymphatic malformations, etc. The ISSVA Classification of Vascular Anomalies was recently updated by the Society’s Scientific Committee and Board to incorporate these changes. It was adopted at the last workshop in Melbourne, Australia (April 2014). In the last edition, the section on tumors was expanded to list the main recognized vascular tumors, classified as benign, locally aggressive or borderline, and malignant. A list of well-defined diseases was included under each generic heading in the simple vascular malformations section. A short definition was added for eponyms. Two new sections were created: one dealing with the malformations of individually named vessels (previously referred to as “truncular” malformations); the second groups together lesions with an uncertain or debated nature (tumor vs malformation).
Vascular anomalies: from Hamburg to Boston
Congenital vascular malformations (CVM) remain an enigma among the vascular disorders as it is a difficult and confusing diagnostic and therapeutic clinical entity with a wide range of clinical presentations. The old classification did not take into account the etiology, anatomy, and pathophysiology, which often led to misguided and mistaken terminology. To achieve a consensus regarding the nomenclature and management of CVM, a new classification was proposed in the workshop held in Hamburg, Germany in 1988. The new classification, so called Hamburg classification differentiates between arterial defects/malformations, venous malformations, arteriovenous malformations, lymphatic malformations, capillary malformations, and combined vascular defects, ie, hemolymphatic malformations. A subclassification distinguishes between extratruncular and truncular forms, depending on the stage of angiogenesis. Extratruncular forms can be diffuse, infiltrating or limited, or localized. Truncular forms can be obstruction or dilatated. This new definition, based on the embryological characteristics of the CVMs, later became known as the “modified” Hamburg classification. The Boston group proposed another classification system in which all vascular anomalies were divided into two categories: vascular malformations and vascular tumors, which was subsequently adopted as the ISSVA classification. Lee concluded that the “modified Hamburg classification” is a more clinician-friendly version and has been considered as a guideline for treatment selection and prognosis of treatment outcome.
Update on genetics of vascular anomalies
Vikkula reported that, in the angiopoietin receptor gene TEK, somatic mutations cause solitary and multiple sporadic venous malformations (Nat Genet. 2009). Another report in 2015 showed that somatic activating PIK3CA mutations also cause venous malformations. For example, the blue rubber bleb nevus syndrome is caused by somatic TEK mutations (TIE2). In a recent trial, rapamycin improved TIE2-mutated venous malformations in murine models and human subjects. A multicenter European phase 3 clinical trial is ongoing that is investigating sirolimus in vascular anomalies. The speaker introduced VASCern as the European network on rare multisystem vascular diseases and the VASCular Anomaly Patient Association (VASCAPA).
New advances in the treatment of Klippel-Trenaunay syndrome
The Klippel-Trenaunay syndrome is a hemolymphatic malformation, its clinical presentation includes atypical varicose veins, diffuse angiomas, arteriovenous fistula, pigmentary nevus, different measure and length of the legs. There are three periods in the surgical management of Klippel-Trenaunay syndrome, where the first period involves vein resection and bloom techniques, the second period involves vein resection, regional segmentary skeletonization, and the third period involves endoluminal laser ablation, vein resection, and a foam technique. Simkin concluded that the regional segmentary skeletonization is a good technique and the recurrence of varicose veins increases up to 30%. He stated that the endoluminal laser ablation is a good technology for treating recurrent varicose veins and superficial microarteriovenous fistulas.
Genetics
Genetics of vascular anomalies
Vikkula explained that inherited disorders are often autosomal dominant, but with variable expressivity and penetrance. In contrast, the sporadically occurring congenital disorders have no family history and are the most common form of most vascular anomalies. Another factor is the heterogeneity. For example, there are currently mutations in 28 known lymphedema-associated genes. The common effects of these different genes are also known. There is variable expressivity of the same mutation. In venous malformations, more than 60% are due to somatic mutations. Different genes could cause the same phenotype and single genes could cause multiple phenotypes. The speaker presented a recommended classification of the vascular anomalies from the International Society for the study of vascular anomalies to make the diagnosis more precise for a better stratification. Different signaling pathways can be activated in vascular anomalies. Vikkula pointed out that there is no transformation for oncogenic driver mutations. At the end of the talk, the speaker presented a vascular panel for diagnostics and carrier screen used at the Centre for Human Genetics in Brussels, Belgium.
Genetics of platelet disorders
Watson presented the risk factors for platelet function disorders, namely age, antiplatelet drugs, surgery, gene mutations, thrombocytopenia. He then discussed the variability in hemostatic parameters using three clinical examples from patients with Glanzmann’s thrombasthenia. Subsequently, he introduced Hermansky-Pudlak syndrome, which consists of albinism, visual defects, bleeding, and other symptoms, and it is a recessive disorder. The speaker pointed out the significant variability in symptoms, even within a specific genetic disease. It can be difficult to differentiate patients with platelet bleeding disorders from normal patients. Watson presented guidelines for analyzing causality of single nucleotide variants in human disease (Nature 2014). Many single nucleotide variants have no apparent phenotype. A large, international, multicenter study was performed to identify the genetic basis of unresolved bleeding and platelet disorders by exome sequencing. In summary, next generation sequencing is here, and it is cost-effective in identifying gene defects in families where there is a clear pattern of inheritance. In patients with no clear pattern of inheritance, several gene defects are likely to contribute to bleeding. Most gene defects should be considered as risk factors for bleeding.
Genetics of venous disease
Venous disease comprises varicose veins, venous ulcer, malformations, venous thrombosis, reticular vein flares, and recurrent varicose veins. The underlying DNA sequence and gene polymorphisms are modified by many factors, such as protein activity control, transcriptional control, environment, hormones, RNA processing and transport control, and translation control before resulting in a phenotype/gene expression. Van Rij asked the question whether there is a gene that determines the likelihood of developing varicose veins. In patients with lymphedema distichiasis, 100% have venous reflux, where 50% of the patients develop varicose veins. This syndrome was first related to the FOXC2 gene mutation. The speaker report
ed that the first link to varicose veins was made after an analysis of the phenotypic abnormalities in lymphedema-distichiasis syndrome in 74 patients with a FOXC2 mutation. A monogenic FOXC2 mutation regulates gene expression in angiogenesis; this mutation is highly expressed on valve leaflets. It is implicated in both lymphatic and vascular development, but its exact role is unknown. Linkage studies in twins have shown that varicose veins are heritable and FOXC2 is strongly implicated. A genome-wide association study was performed to investigate whether the patients with varicose veins commonly have FOXC2 mutations; the results could not confirm an association with FOXC2. Obviously, varicose veins are a complex genetic disorder. At present, many genes are candidates for venous insufficiency, such as FOXC2, estrogen receptor β, tumor necrosis factor, homocysteine, etc. Recently, a systematic review on genetic polymorphism of vein wall remodeling in chronic venous disease was published in Blood. van Rij reported on a genome-wide association analysis for chronic venous disease that identified EFEMP1 and KCNH8 as susceptibility loci. He stressed again that one condition may be influenced by many genes and conversely one gene may cause many conditions. At the end of his presentation, the speaker reported the results of many studies showing that varicose veins and venous thromboembolism share familial susceptibility and possibly genetic factors.
Debates
SOX trial: rubbish outcome or rubbish design?
A number of criticisms of the trial were pointed out by Shalboub, such as end points (Villalta, Ginsberg) not fitting the purpose and a poor or overestimated compliance (55.6%). Furthermore, the SOX trial can be criticized for the timing and inadequacy of applying the stockings. Graduated compression stockings (GCS) and placebo stockings were mailed to study participants without a face-to-face consultation to demonstrate their correct application. This lack of face-to-face contact may have had an effect on compliance in the trial. The results of a meta-analysis that evaluated the effectiveness of GCS in preventing postthrombotic syndrome showed uncertainty because of sampling variability and heterogeneity among three randomized controlled trials that is too high to conclude in favor or against an effect of wearing compression stockings in preventing postthrombotic syndrome. An effect may be present for higher values of baseline risk. Furthermore, the authors of another meta-analysis (Lancet Haematol. 2016;3(6):e293-e300) showed that the use of GCS does not significantly reduce the development of postthrombotic syndrome, concluding that, at this time, the body of evidence is limited. Since there is presently equipoise, further conclusive studies are needed to establish the role of this therapy. Furthermore, in the IDEAL deep vein thrombosis trial (Lancet Haematol. 2018;5(1):e25-e33), individualized therapy with elastic compression stockings for the prevention of postthrombotic syndrome was noninferior to the standard 24-month duration of therapy. Using the same scoring system (Villalta scale), a large discrepancy in postthrombotic syndrome can be observed in the two trials, despite that there was a low baseline postthrombotic syndrome risk in the SOX trial. Even Susan Kahn affirmed that she has not changed her practice following the SOX trial and continued to prescribe GCS to all patients with deep vein thrombosis with early deep vein thrombosis–related swelling. In conclusion, the clinical and scientific community does not have confidence in SOX. This trial will not be the “last word” on this important clinical question.
Before the SOX trial, previous studies assessing the efficacy of GCS in the prevention of deep vein thrombosis were small (<200 patients), single center, and not blinded. This has a great design, and we should believe the results, because it was a blinded, large, multicenter trial providing generalizable results and less bias. Furthermore, all subgroups of patients were analyzed. Kearon stated that we are blaming this trial only because we do not like its results. As an example, regarding the criticisms affirming that GCS were not worn enough, he replied that around 70% of patients used GCS during the study follow-up period. Therefore, stockings were worn a lot. However, frequent use did not mean better outcomes (HR, 0.96). Furthermore, men wore more GCS and did worse (HR, 1.6). In addition, it should be taken into account that a lower use might reduce treatment effectiveness, but not eliminate it. Thus, he concluded that the SOX trial is a great study with dependable (valid) results.
TED stockings are a WASTE of time
The Octavia study demonstrated that stopping the use of elastic compression stockings (36 to 46 mm Hg) after 1 year in compliant patients with proximal deep vein thrombosis seemed to be noninferior to continuing elastic compression stockings therapy for 2 years. The use of elastic compression stockings for 2 years had slightly more benefit than use for 1 year for patients with a postthrombotic syndrome. In the group who continued elastic compression stockings, there was a 6.9% reduction (though not much in severe postthrombotic syndrome). Furthermore, in the SOX trial, elastic compression stockings (30 to 40 mm Hg) did not prevent postthrombotic syndrome after a first proximal deep vein thrombosis, though poor compliance was reported among the participants. Nandurkar stated that we are probably relying excessively on stockings despite the lack of evidence, especially concerning the 18 mm Hg thromboembolic deterrent stockings. Regarding the prevention of deep vein thrombosis, thromboembolic deterrent stockings are probably useful in surgical patients, but not useful in medical patients. Moreover, the problem of compliance or a bad fit causing other constrictions outside of their cost should always be taken into account. Last, but not least, thromboembolic deterrent stockings can distract from effective pharmacological prophylaxis.
Graduated compression stockings can be differentiated from thromboprophylactic stockings, as they are designed to work in bed with low compression strength (15 to 18 mm Hg) and from medical compression stockings (MCS), as they are designed to work in a sitting position with higher compression strength (18 to 32 mm Hg). Thromboembolic deterrent stockings (8 to 18 mm Hg) can be placed in the former group. They act by decreasing the venous diameter in the horizontal position and increasing bloody velocity (therapy reducing stasis). They also show a massaging effect that relies on muscle movements reacting with the stocking, on the pressure gradient (graduated compression), and they include superficial veins external to the muscle pumps.
In an evidence-based consensus statement published in Phlebology in 2017, the authors concluded that the role of stockings in addition to anticoagulation is limited (evidence grade 2C). However, Kalodiki stated that, just because the evidence is not there, it does not mean that thromboembolic deterrent stockings do not work. During her talk, she reviewed a paper (Smith and Pell. BMJ. 2003;327:1459-1461). The authors of this review were unable to identify any randomized controlled trials on parachute intervention. They concluded that, as with many interventions intended to prevent ill health, the effectiveness of parachutes has not been subjected to rigorous evaluation by using randomized controlled trials. Advocates of evidencebased medicine have criticized the adoption of interventions evaluated by using only observational data. They think that everyone might benefit if the most radical protagonists of evidence-based medicine organized and participated in a doubleblind, randomized, placebo-controlled, cross-over trial of the parachute. As discussed by Kalodiki, compression stockings for thromboprophylaxis can be useful for surgical interventions, long-haul flights, acute medical in-patients, and stroke patients other than in other conditions, such as postthrombotic syndrome, cancer, thrombophilia, chronically immobilized, bariatric, chemotherapy, trauma, neurosurgery, pregnancy, critically ill. The authors of the CLOTS trial collaboration (Clots in Legs Or sTockings after Stroke) were able to demonstrate that proximal deep vein thrombosis occurs more often in patients with stroke who wear below-knee stockings than in those who wear thigh-high stockings (Ann Intern Med. 2010;153(9):553-562). The AT9 edition of ACCP guidelines (Chest. 2012;141(suppl 2):e195S-e226S) suggest using graduated elastic compression (2C) or intermittent pneumatic compression (2C) for acutely ill medical in-patients with a major bleeding risk. Finally, results of a Cochrane systematic review (Cochrane Database Syst Rev. 2014;(12):CD001484) showed that graduated elastic compression is effective in diminishing the risk of deep vein thrombosis in hospitalized patients, with strong evidence favoring their use in general and orthopedic surgery.
Stripping is archaic and unsuited to modern day superficial vein reflux management
Treatment of superficial vein reflux involves open surgery (high ligation and stripping), saphenous preservation (ASVAL, CHIVA), and endovenous ablations (radiofrequency, laser, ultrasound-guided foam sclerotherapy, mechanochemical endovenous ablation [MOCA], cyanoacrylate ablation). Modern high ligation and stripping is an invasive technique, requiring anesthesia and sedation. It is a painful procedure that may cause bruising, hematoma, nerve and lymphatic injury, and a delayed return to work. Deep vein thrombosis can develop in up to 5.3% of cases, and the recurrence rate is between 6% and 66%. The early benefits of endovenous treatments over stripping in randomized controlled trials include less pain and bruising, fewer wound complications, earlier return to work, higher patient satisfaction, and an improvement in quality of life. The SVS/AVF, European, the UK NICE, and AVF guidelines recommend endovenous thermal ablation (radiofrequency or laser) or ultrasound-guided foam sclerotherapy over high ligation and stripping (grade of recommendation: 1 [strong], level of evidence: B [moderate quality]). In conclusion, if expertise and endovenous technology is available and affordable for the patient, then the proven early benefits justify using endovenous procedures over stripping for ablation of the superficial reflux.
Open surgery vs endovenous treatments: what factors would make you consider open surgery? Anatomical factors: short proximal sections, very superficial trunk, excessive tributaries; health system factors: rules, regulations; cost factors: to patients, overall cost, remuneration; treating doctor factors: training facilities, money, instrumentation, facility, access; desired end point and number of visits; and patient wishes. In conclusion, stripping is not archaic and remains a very relevant option for saphenous vein reflux in some cases and, when all factors are considered, it is a viable option in the current guidelines, such as the NICE and SVS/AVF guidelines.
