Prevalence of patients with chronic venous disease-related symptoms but without visible signs (described as C0s in the CEAP classification): the Italian experience
University Hospital of Padua, Italy
SUMMARY
The [C[0S]] item of the CEAP classification is one of the emerging topics in venous disease epidemiology. It has been referred to by several studies, but until today it has not been clearly assessed by any specific study. In Italy, the topic has interested several groups of researchers since the 1980s. The author carried out several pilot studies with infrared photoplethysmography (PPG), strain-gauge plethysmography, laser-Doppler and echo-duplex. The results suggested that one of the pathophysiological causes of venous disease-related subjective symptoms without varicose veins could be caused by the reduction of the venous wall tone, and the term hypotonic phlebopathy (HP) to describe these patients with chronic venous-disease related symptoms without varicose veins has been proposed. The diagnosis criteria are focused on symptoms (heavy legs in upright position, restless leg syndrome, subedema and/or evening edema) and signs detected by photoplethysmography (PPG), strain-gauge plethysmography and duplex scanning (reduction of the muscle- venous calf pump and increase of the venous wall compliance).
The prevalence of HP has been assessed between 1989 and 1992 by the Acireale Project, and it showed a 15.90% morbidity, with higher prevalence in females. The most important risk factors for HP are family history and pregnancy. However HP is not rare in males; the principal risk factor for this gender is long periods in a standing position at work.
These observations have been independently confirmed by two studies carried out in France in 1992, which showed a 15% prevalence in a similar group of subjects with functional venous insufficiency.
The author suggests the introduction of the functional phlebopathy term into clinical practice; the diseases characterised by subjective symptoms without anatomic damage, and in their context identify several different frameworks such as the constitutional phlebostasis, HP, and probably many more.
INTRODUCTION
The C0S class of the clinical CEAP classification1 indicates a particular kind of subject with venous disease-related symptoms, such as heavy legs in the upright position, restless leg, subedema, and/or evening swelling, but without visible signs of venous diseases.
All these subjective symptoms immediately evoke the picture of chronic venous insufficiency, at least when they are associated with clear signs of varicose veins or previous venous disease. Despite the condition is often encountered in daily practice, the so-called phlebopathic symptoms have never been specified in any of the published literature, not even when this aspect was among the main objectives of the study.2,3 Conversely, it is harder to interpret the meaning of these symptoms when the clinical picture is not clearly defined, and when there are no objective signs of reference of venous disease.
In the past, different definitions have been proposed, such as phlebopathic diathesis, prevaricose syndrome, and functional phlebopathy. The last one, proposed by Bassi in the 1970s,4 is the most correct, in our opinion, because it stresses the presence of an incorrect functioning in the absence of anatomic alterations.
In 1982, our group indicated that the prevalence of these subjects with varicose symptoms without varicose veins was about the 20% of all people who visited our vascular lab because of suspected venous disease.5
In 1986, we investigated 35 symptomatic subjects, using reflection light photoplethysmography (PPG) and we found a ÄR of 200±30 mV, significantly (P<0.005) lower than normal values for our laboratory.6,7 The ÄR indicates the difference between the reflexion light of subcutaneous venous plexus measured after 10 flexion-extension movements of the foot and the same measurement at rest. The measurement’s unit of the PPG investigation utilised in the 1980 was the milli volt (mV). This reduction in muscle-venous calf pump effectiveness, according to the pathophysiological behaviors of the varicose syndrome, suggested that the varicose symptoms without varices could be caused by a reduction of the venous wall tone. In fact, by artificially increasing the venous tone with elastic bandages, we observed a normalization of ÄR of PPG.8
Believing that these subjects have a reduction of the venous tone without any organic damage, we proposed the term of hypotonic phlebopathy, and we set up an epidemiological study to confirm our hypothesis and to assess the morbidity of this venous dysfunction.
METHODS FOR THE “ACIREALE PROJECT”
One thousand five hundred people were enrolled from the electoral list of Acireale, small town of western Sicily with 50 000 inhabitants, stratifying subjects for age, sex, social level, and residency (sample groups of farmers, fishermen, service industry workers, and students). One thousand thirty-one people replied positively to the invitation by mail to join the study. All participants received a detailed questionnaire on venous disease history, and underwent an angiological clinical examination to assess the evidence of subcutaneous veins, and several vascular investigations, such as continuous wave (CW) Doppler, strain-gauge (SG) plethysmography, PPG, Echo- Duplex scanning, and laser-Doppler.
Epidemiology
The questionnaire enquired about subjective symptoms, family history, obesity, number of pregnancies, and use of oral contraceptives. The prevalence of hypotonic phlebopathy was assessed according with the following criteria based on subjective symptoms and objective signs assessed by the clinical examination.
The questionnaire enquired about subjective symptoms, family history, obesity, number of pregnancies, and use of oral contraceptives. The prevalence of hypotonic phlebopathy was assessed according with the following criteria based on subjective symptoms and objective signs assessed by the clinical examination.
Hypotonic phlebopathy
– Subjective symptoms always present;
– Continuous wave Doppler or echo-duplex scanning showing venous patency and absence of valve dysfunction or reflux;
– PPG with ÄR < 250 mV;
– Strain-gauge plethysmography: MVIV >3.0 mL %, with DV <1.7 mL %.
The maximal venous incremental volume (MVIV) is the maximal volume reached by the calf during the venous occlusion at the rest, in supine position with the strain gauge placed around the maximal circumference of the calf.
The ÄV indicates the difference between the calf volume measured after 10 flexion-extension movements of the foot and the same measurement at rest. In this dynamic measurement the subject was in the seating position with the strain gauge placed around the maximal circumference of the calf.
Latent hypotonic phlebopathy
– Subjective symptoms referred to in intermittent fashion (spring, summer, pregnancy, standing work, etc);
– Continuous wave Doppler or echo-duplex scanning showing venous patency and absence of valve dysfunction or reflux;
– PPG with ÄR <250 mV;
– Strain-gauge plethysmography: MVIV >3.0 mL %, with ÄV <1.7 mL %.
Enhanced hypotonic phlebopathy
– Subjective symptoms referred to as continuously present during the examination period, but occasionally in the past, and related to an identifiable cause (ie, people with occasional subjective symptoms in the past and stable symptoms in the last 4 years, after pregnancy).
– Continuous wave Doppler or echo-duplex scanning showing venous patency and absence of valve dysfunction or reflux;
– PPG with ÄR <250 mV;
– Strain-gauge plethysmography: MVIV >3.0 mL %, with ÄV <1.7 mL %.
Senile hypotonic phlebopathy
– Subjective symptoms referred to by aged people as continuously present since the 6th decade, and never or occasionally in the past;
– Continuous wave Doppler or echo-duplex scanning showing venous patency and absence of valve dysfunction or reflux;
– PPG with ÄR < 250 mV;
– Strain-gauge plethysmography: MVIV >3.0 mL %, with ÄV <1.7 mL %.
Varicose disease
– Evidence of subcutaneous dilated veins with reflux, with or without subjective symptoms.
Venous valve incompetence without varicose veins
– People showing a small reflux (less than 0,5 sec) in one or more parts of some superficial veins, without dilatation.
This last unusual diagnosis was needed because more people showed small anatomical and functioning alterations, so small that it was impossible to assign to the varicose vein a diagnosis, but nevertheless it was impossible to consider it normal from an anatomical point of view because of the reflux.
Continuous-wave Doppler was performed in the standing position, focusing on the most important veins of the lower limb (femoral vein, saphenous cross, great saphenous vein above and below the knee, popliteal vein, small saphenous vein, tibial veins) assessing the venous patency and the reflux.
Echo-Duplex scanning was used in people who showed any evidence or suspicion of venous reflux at continuous-wave Doppler, and in a small group of thirty subjects to assess the venous compliance. This parameter was reported by measuring the difference between the venous diameters in the supine position and in the upright position.
PPG (reflection light photoplethysmography) was performed the standardized way, that is, in the sitting position, to assess the ÄR between the baseline and top values of the curve after 10 flexion-extension movements of the foot; the refilling time was also measured in the ankle.
Strain-gauge plethysmography was performed to assess the venous wall compliance during venous occlusion, measuring in the supine position the maximum incremental venous volume at the calf level (MVIV). In the sitting position the drop of volume (ÄV) was measured after 10 flexion-extension movements.
Laser Doppler parameters (resting and standing flux and venous-arteriolar reflex VAR) were used in a small group of twenty subjects to assess the microcirculatory features. Fifty healthy subjects, without symptoms and/or signs of venous disease were utilized as a normal control group.
RESULTS
The results shown in this paper come from those published in the original paper in 2000,9 and have been revised and classified following the CEAP criteria,1 including the recent revisions and refinements.10-18 The most important suggestion of these recent revisions was to add the letter N in the items E, A, and P of the CEAP classification. The item AN indicates the condition of patients without any anatomical alteration of the venous system; this suggestion is very appropriate for Hypotonic Phlebopathy [HP] patients and we used it in our results. The item PN indicates the absence of reflux, obstruction, and reflux plus obstruction (frequently observed in several veins of patients with chronic venous disease). We agree also with this suggestion. Nevertheless, because we hypothesized and identified the reduction of venous tone as pathophysiological alteration in HP patients presenting without reflux and without obstruction, and because the reduction of venous tone is not a physiological status, instead of PN we prefer to indicate HP as P//(N).
Concerning the item EN, which would indicate an unidentified aetiology, we disagree with this suggestion because in the universal semiology of medical definition, until today, a disease with unidentified aetiology is defined as PRIMARY DISEASE. Because HP cannot be defined as CONGENITAL DISEASE, and it is not SECONDARY to other pathophysiological conditions, we considered HP as a primary disease. For these reasons in the following pages the Hypotonic Phlebopathy (HP), is indicated as C(0S) E(P) A(N) P(//N).
Prevalence of the different conditions:
The 1031 participants of the survey were divided up as follows:
– 330 (32.00%) were healthy;
– 140 (13.57%) were affected by “other vascular diseases”;
– 234 (22.69%) had varicose veins (VV [C[2-3-4]S – EP – AS – P
– 163 (15.80%) were symptomatic and had small reflux (valve incompetence) without varicose vein dilatation (reflux without varicose veins (RWVV [C[0S] – EP – AN – PR]);
– 164 (15.90%) were symptomatic but did not present varicose veins (hypotonic phlebopathy, HP [C0S – EP – AN
– P//[N]]). Among the 164 HP patients one can distinguish:
• 44 (26.83%) with hypotonic phlebopathy (HP)
• 45 (27.43%) with latent HP
• 49 (29.89%) with enhanced HP
• 26 (15.85%) senile HP
The prevalence of HP in females was twice as many this in males whatever the age group.
Latent, enhanced, and senile HP showed a uniform distribution for sex.
Males showed a higher prevalence in latent HP than females in the groups aged 30 to 39, and 40 to 49; in the 40-to-49 year age group, males had a higher prevalence in the enhanced HP too.
These findings are probably due to the greater attention paid to health problems in the 4th and 5th decades of age, with a greater response to the invitation to participate.
Prevalence of venous symptoms in hypotonic phlebopathy
About the most characteristic symptoms of these 164 patients with HP, we found:
– heavy legs: 122 (74.39%: 26.21% males, and 48.17% females);
– evening edema: 58 (35.36% : 10.36% males, and 25.0% females); edema, never reached the clinical characteristics of C3 classification;
– night resting cramps and restless leg syndrome: 48 (29.26%: 9.14% males, and 20.12% females).
Leg heaviness is the most frequent symptom. Women, especially, report it (48.17%), in agreement with usual clinical observations.
Men report it less (26.21%). Evening edema and restless leg syndrome have a lower prevalence than heavy legs.
Prevalence of risk factors in hypotonic phlebopathy
The risk factors considered by our questionnaire were family history for venous disease, obesity, constipation, pregnancy, and use of oral contraceptives. The prevalence of the risk factors in the different sub-groups of HP is summarized in Table I.
Out of the 89 women identified as HP (all categories), 45 had one or more pregnancies, and 11 used oral contraceptives, either at time of examination or in the past. The prevalence of risk factors in the women of our study is summarized in Table II.
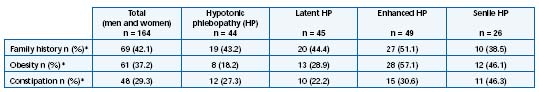
*The percentage (%) is related to the number of patients n in each sub-group of HP.
Table I. Prevalence of risk factors in male and female patients with hypotonic phlebopathies (Acireale study).
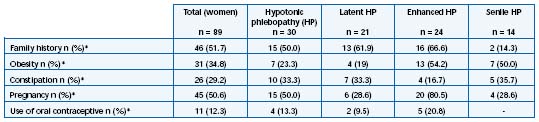
*The percentage (%) is related to the number of patients n in each sub-group of HP.
Table II. Prevalence of risk factors in the women with hypotonic phlebopathies (Acireale study).
Vascular Investigations
PPG – The average of ÄR was 275±40 mV in healthy people, and 200±15 mV in HP [C0S – EP – AN – P//[N]] (P<0.005), showing a small yet significant reduction of the effectiveness of muscle-venous calf pump. In VV [C[2-3-4]S – EP – AS – PR] ÄR showed the lowest values, with very high (P<0.0005) statistical significance versus HP and healthy people (Figure 1). The refilling time of PPG showed similar behavior, with a small reduction in the HP and very important reduction in VV (Figure 2).
Strain-gauge plethysmography – The average of MVIV was 4.5±0.4 mL % in HP and 2.9±0.3 mL % in healthy people (P<0.005). ÄV was 2.7±0.5 mL % in HP and 1.5±0.4 mL % in the controls.
Echo-Duplex-scanning – We did not find reflux or obstruction in subjects with HP. Out of 20 subjects with HP and 10 healthy subjects, received an Echo-Duplex scanning examination, to assess the venous wall compliance, measuring the difference between the vein diameter in supine and upright position. The diameter was measured at the popliteal vein, tibio-peroneal trunk, and gastrocnemial veins. The venous diameter was always higher in the upright position. The difference between diameters in the two positions was:
- HP [C0S – EP – AN – P//[N]]: popliteal v. 3.40±1.10 mm; tibio-peroneal trunk 2.70±0.80 mm, gastrocnemial v. 3.50±1.30;
– healthy people: popliteal v. 1.50±0.53 mm, tibio-peroneal trunk 1.10±0.57 mm, gastrocnemial v. 1.30±0.48 mm.
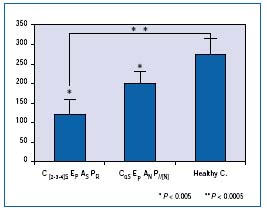
Figure 1. Photoplethysmography (PPG) investigation of the
Acireale patients. Values on the Y-axis represent the difference
between the reflexion light (ΔR) of subcutaneous venous plexus
measured after 10 flexion-extension movements of the foot and
the same measurement at rest. ΔR is expressed in mill volts (mV).
Comparison of ΔR between healthy subjects and patients with
varicose veins, and hypotonic phlebopathy is shown on this graph.
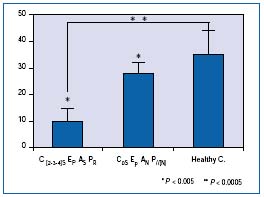
Figure 2. Photoplethysmography (PPG) investigation of the Acireale
patients. Values on the Y-axis represent the refilling time in seconds
(sec). Comparison of refilling time between healthy subjects and
patients with varicose veins, and hypotonic phlebopathy is shown
on this graph.
The statistical analysis showed that the difference was relevant (P<0.0001)19 (Figure 3). People with RWVV [C[0S] – EP – AN – PR] mostly showed a localized valve dysfunction, with flaps or prolapse.
Laser-Doppler – 10 HP [C0S – EP – AN – P//[N]] subjects and 10 healthy people received a laser-Doppler examination (with the probe placed 10 cm above the internal malleo- lus) to complete the functional venous assessment. This study showed a significant (P<0.0001) increase of resting and standing flux in HP (RF 10.4±1.9 perfusion unit, SF 7.28±1.2) than in healthy people (RF 8.0±0.9, SF 3.6±0.6). The venous-arteriolar reflex was reduced (30% in HP, 55% in controls).20
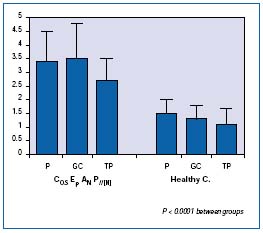
Figure 3. Echo-Duplex scanner examination of the Acireale
patients. Values on the Y-axis represent the difference in venous
diameter (in mm) in the measurement between the upright
and the supine position. Abbreviations: P = popliteal vein,
GC = gastrocnemial vein and TP = peroneal tibial vein.
COMMENTS
In our opinion, the increased MVIV and the decreased ÄV of strain-gauge plethysmography, and the decrease in PPG ÄR without reflux or venous obstruction, demonstrate that the symptoms in HP [C0S – EP – AN – P//[N]] could be sustained by the increase of the venous wall compliance.
The reduction of PPG refilling time without valve dysfunction could be explained as a faster refilling caused by a decrease of filling resistance sustained by the reduction of the venous and venular tone, showed also by the changes of the parameters of the laser Doppler.
On the other hand, the reduction of venous tone in these symptomatic subjects is confirmed by the behavior of venous diameter difference in the supine and upright positions.
These results confirm our hypothesis of the reduction of venous tone with the increase of venous wall compliance are the pathophysiological substrate of the varicose symptoms without varicose veins HP [C0S – EP – AN – P//[N]].
Our findings, collected since 1982, have been independently confirmed by two French studies. One was carried out on military recruits,21 the second on a vast survey in the Paris region.22 The authors found a 15% prevalence of functional venous insufficiency in the 20-to 30-year age group. They remark that the clinical disturbances are only functional (heavy legs, paresthesia, nocturnal cramps in the calves, restless legs) without clinical and anatomical abnormalities of the veins. The disturbances often reflect a hyperdistensibility of venous wall, which can be detected by venous occlusion plethysmography, but it is fairly common to see varicosities and telangiectasias.23
This occasional concurrency of experimental data and the similar conclusions reached by two different groups in different times are a very good unexpected confirmation that our hypothesis was true.
The venous wall hypotonia could be sustained by the structural alterations of connective,24,25 cellular,26,27 matrix, and smooth muscle cells dysfunction28 of the venous wall, like those recently described in the varicose veins. Leg heaviness is the most frequent symptom, especially referred to by women in agreement with usual clinical observations. Men report this symptom fewer times (26.21%). Evening edema and restless leg phenomena have a lower prevalence than heavy legs, as underlined also by the Edinburgh study.
The family history of venous disease is the risk factor with the highest prevalence (42.07%). It seems to be important in determining the appearance of all types of HP and it occurs especially in the female gender, except in senile HP.
Obesity is the second risk factor of HP (37.19%); nevertheless its importance is modest in constitutional HP, and only for women (15.90%). In latent HP its role remains low, though more important for males (20.00%). In senile HP it is important for both sexes, appearing in 46.15% of senile population. But its highest importance is as an enhancing factor in enhanced HP (57.14%), especially for men (30.61%).
Constipation has a general prevalence of 29.26%. It is an important risk factor especially for women, and in senile HP for both gender. Like obesity, it plays a very important role as an enhancing factor for males.
Pregnancy is a very high risk factor for HP. In our study we found 89 women with HP and 45 of them (50.56%) had had one or more pregnancies. It has a very important role as an enhancing factor; 80.53% of the women with enhanced HP had had one or more pregnancies. However, we think that in senile HP the enhancing role of previous pregnancy is less important than obesity and constipation.
Conversely, the use of oral contraceptives is not a risk factor for HP; its general prevalence is below 20%, reaching this prevalence value only as an enhancing factor, but the significance is very low.
About the 163 patients of the study population (15.80%) with valve incompetence and reflux in different levels of the superficial venous system, without varicose veins (RWVV [C[0S] – EP – AN – PR]), we underline the relevance of this anatomic and functional condition in males, being related to stress caused by work in a prolonged standing position. From the pathophysiological point of view, it is never a healthy state. Its clinical evidence could be modest or absent for a long time but its progression in varicose veins is always possible.
CONCLUDING REMARKS
The C0s CEAP patients’ condition as described in the CEAP classification is a true problem in the clinical practice. Few papers have been published about this topic but recently the interest of the researchers has been growing. Beyond our opinion, we remind the constitutional phlebostasis with endocrine peculiarities described by Allegra,29,30 the papers by the group of Cloarec, and the recent report by Jawien. In his epidemiological study,31 the majority of the people classified as C0 (20% of general population) was symptomatic32 (C0-S).
According to Bassi, we suggest including in the classification of venous diseases the functional phlebopathies characterised by subjective symptoms without anatomic damage, and in their context identify several frameworks such as the constitutional phlebostasis, hypotonic phlebopathy, and probably many more.
The identification of these clinical pictures is important not only from the nosographic and academic point of view, but also in clinical practice. In fact, especially severe symptoms of HP are improved by regular use of phlebotonic drugs, (spring and summer times).
The hypothesis that the functional phlebopathies, and particularly hypotonic phlebopathy, could be a prodromic phase of varicose disease (prevaricose syndrome) is rather improbable. Our uncontrolled follow-up carried out for over 10 years has shown varicose evolution only in the group RWVV in which a structural anatomic damage in the form of the valve dysfunction is still present.
The diagnosis of HP must be supported by the assessment of venous wall hypotonia by instrumental examination; the [C0S – EP – AN – P//[N]] alone, until today does not authorize the conclusive diagnosis of HP. As remarked by H. Partsch in his kind comment to the Acireale Project,9 our paper is probably the first attempt to correlate the subjective venous disease-related symptoms with the functional parameters from vascular lab.
The strength of the relationship does not emerge because this goal was not included in the study design. The relationship between subjective symptoms and functional parameters from vascular lab is one of the main goals of another study recently approved by the Ethic Committee of Padua, and that we hope it will start as soon as possible.
From the epidemiological point of view, we confirm the importance of family history and pregnancy as the main risk factors of dilative phlebopathies. Conversely, the often-suggested role of oral contraceptives as a risk factor for venous wall dysfunction (varicose veins and HP) has not been confirmed.
Therefore, concerning these kinds of phlebopathies, the use of oral contraceptives is not harmful; on the contrary, since they reduce the number of pregnancies, which are directly related to varicose veins, they could be paradoxically considered preventive. Nevertheless, we need to remember that using oral contraceptives enhance the risk of venous thrombosis because they interfere with the coagulative system.
REFERENCES
2. Bradbury AW, Evans CJ, Allan PL, et al. Vascular Surgical Society of Great Britain and Ireland: Symptoms of Varicose Veins. Br J Surg. 1999;5:700.
3. Fowkes FGR. Prevalence and risk factors for chronic venous insufficiency. Acta Phlebol. 2000;1:69-78.
4. Bassi G. La patologia venosa funzionale. In Bassi G: Compendio di Terapia Flebologica. Torino: Minerva Medica eds; 1985.
5. Tamburino G, Andreozzi GM. The initial stage of venous insufficiency. In Tesi M, Dormandy J, eds: Superficial and Deep Venous Diseases. Turin: Minerva Medica; 1982;87-90.
6. Monaco S, Ferrara M, Minardo G, Minacapelli C, Signorelli S, Andreozzi GM. La reografia a luce riflessa (RLR) nella valutazione della Flebopatia Ipotonica Costituzionale. Acta Cardiol Medit. 1986;4:3;155-160.
7. Ferrara M, Minardo G, Monaco S, Lo Duca S, Oddo MG, Signorelli S, Andreozzi GM. La reografia a luce riflessa (RLR) nella semeiotica strumentale Flebologica. Acta Cardiol Medit. 1986;4:195-199.
8. Ferrara M, Monaco S, Cacciaguerra G, Amico-Roxas MT, Di Pino L, Signorelli S, Andreozzi GM. Pressioni venose e tono parietale venoso. Acta Cardiol Medit. 1986;4:177-183.
9. Eklof B, Rutherford RB, Bergan JJ, et al. Revision of the CEAP classification for chronic venous disorders: consensus statement. J Vasc Surg. 2004;40:1248-1252.
10. Andreozzi GM, Signorelli S, Di Pino L, et al. Varicose symptoms without varicose veins: the hypotonic phlebopathy, epidemiology and pathophysiology. Min Cardioang. 2000;48:277-285.
11. Perrin MR, Guex JJ, Ruckley CV, et al. Recurrent varices after surgery (REVAS), a consensus document. Cardiovasc Surg. 2000;8:233-245.
12. Rutherford RB, Padberg FT, Comerota AJ, et al. Venous severity scoring: an adjunct to venous outcome assessment. J Vasc Surg. 2000;31:1307-1312.
13. Meissner MH, Natiello C, Nicholls SC. Performance characteristics of the venous clinical severity score. J Vasc Surg. 2002;36:89-95.
14. Kakkos SK, Rivera MA, Matsagas MI, et al. Validation of the new venous severity scoring system in varicose vein surgery. J Vasc Surg. 2003;38:224-228.
15. Perrin M, Dedieu F, Jessent V, et al. Evaluation of the new severity scoring in chronic venous disease of the lower limbs. An observational survey conducted by French angiologists. Phlebologie. 2003;56:127-136.
16. Uhl JF, Cornu-Thenard A, et al. Reproducibility of the “C” classes of the CEAP classification. J Phlebology. 2001;1:39-48.
17. Allegra C, Antignani PL, Bergan JJ, et al. The “C” of CEAP: suggested definitions and refinements: An International Union of Phlebology conference of experts. J Vasc Surg. 2003;37:129-131.
18. Moneta GL. Regarding “the C of the CEAP”: suggested definitions and references: an International Union of Phlebology conference of experts (abstract). J Vasc Surg. 2003;37:224-225.
19. Andreozzi GM, Cacciaguerra G, Garozzo S, et al. Echo-Doppler chez les sujets avec phlébopatie hypotonique (abstract). J Mal Vasc. 1995;20(sA):47.
20. Martini R, Bandieramonte G, Blanco G, Garagozzo G, Failla G, Signorelli S, Andreozzi GM. Modificazioni della emodinamica microcircolatoria osservata con tecnica laser Doppler in soggetti con Flebopatia Ipotonica. Acta Cardiol Medit. 1992;10:35-37.
21. Clement R, Blin E, Chaundet X, et al. Prévalence du stade pré-variqueux et de la maladie variqueuse chez l’adulte jeune. 11ème Congrès UIP Montréal; 1992. Phlebology. 1992;1:238-241.
22. Cloarec M, Estryn-Behar M, Griton P, et al. Etude épidémiologique de l’insuffisance veineuse dans une population de l’Ile-de- France. 11ème Congrès UIP Montréal; 1992. Phlebology. 1992;1:242-246.
23. Cloarec M, Barbe B, Griton P, Vanet F. Update on functional venous insufficiency. Phlebolymphology. 1997;3:3-9.
24. Chello M, Mastroroberto P, Zoffrea S, Marchese AR. Analysis of collagen and elastin content in primary varicose veins. J Vasc Surg. 1994;20:490.
25. Maurel E, Azema C, Deloy J, Bouissou H. Collagen of the normal and the varicose human saphenous vein: a biochemical study. Clin Chim Acta. 1990;193:27-37.
26. Lowell LC, Gloviczki P, Miller VM. In vitro evaluation of endothelial and smooth muscle function of primary varicose veins. J Vasc Surg. 1992;16:679-686.
27. Scappaticci S, Capra E, Cortinovis M, et al. Cytogenetic studies in venous tissue from patients with varicose veins. Cancer Genet Cytogenet. 1994;75:26-30.
28. Renaudin JM, Fiscel C, Mercier F, et al. Smooth muscle differentiation in human vein wall at valvular level: comparison with non valvular wall and correlation with venous function. Angiology. 1999;50:21-23.
29. Allegra C, Bonifacio M, Criscuolo A. Les phlébostases constitutionnelles. 10ème Congrès Mondial UIP Strasbourg; 1989. John Libby Eurotet London Paris; 1989.
30. Allegra C. Le flebostasi costituzionali. In: Bilancini S, Lucchi M, eds. Le Varici Nella Pratica Quotidiana. Torino: Minerva Medica eds; 1991:395-401.
31. Jawien A. The influence of environmental factors in chronic venous insufficiency. Angiology. 2003;53:245-256.
32. Jawien A, Grzela T, Ochwat A. Prevalence of chronic venous insufficiency (CVI) in men and women in Poland: multicenter cross-sectional study in 40 095 patients. Phlebology. 2003;18:110-122.
