Relationship between the small saphenous vein and nerves: implications for the management of chronic venous disease
Claude GILLOT,2
Philippe LEMASLE3
Biomédicale des Saint Pères –
Université Paris 5 – France
2 Centre de Chirurgie des Varices –
Neuilly sur Seine – France
3 Le Chesnay – 78150 – France
SUMMARY
The aim of this study was to describe the anatomical relations of the short saphenous vein in the lower limb as an aid in locating important anatomical landmarks in the surgical treatment of chronic venous disease. The small saphenous vein (SSV) runs in a compartment demarcated by muscular fascia and a membranous layer of subcutaneous tissue. Muscular contraction can affect the diameter and hemodynamics of the SSV. In light of the close proximity to associated nerves, the clinician should be well aware of the anatomical pitfalls in order to avoid injury to adjacent structures. Providing complete anatomical information facilitates surgical intervention involving SSV procedures for treatment of venous disease.
INTRODUCTION
The saphenous venous compartments
The venous system of the lower limb consists of two major sets of veins. The deep venous system is comprised mainly of the femoral vein and its tributaries which lie beneath the muscles of the leg and carry most of the blood from the leg. The second set of veins is the superficial venous system, ie, the great saphenous vein and the small saphenous vein. The small saphenous vein arises from the outer aspect of the ankle, passes up the posterior aspect of the calf and leg and empties into the popliteal vein. The great saphenous vein starts anterior to the medial malleolus, ascends vertically along the inner aspect of the thigh and leg and empties into the femoral vein.1 These superficial veins are commonly subject to chronic abnormal dilation and development of varicose veins.
OBJECTIVE
To identify potentially hazardous areas in the treatment of venous disease with surgery and other methods based on anatomical, venographic and ultrasound imaging studies of the saphenous venous compartment.
METHODS
The subcutaneous tissues of the lower limb are arranged in two connective fasciae in the thigh and the leg: superficially below the skin in a membranous layer (formerly called the fascia superficialis), and a deeper layer, the muscular fascia, covering the muscles. These two layers are in close relation with the saphenous venous system. The superficial layer covers the saphenous trunks, while the tributaries are located subcutaneously.
Bailly2 and then, Lesmasle et al3, described the great saphenous vein (LSV) as forming the “Egyptian eye” describing the configuration of the LSV between the muscular fascia and saphenous fascia. With duplex scanning, these fasciae appear as two white lines surrounding a black dot; thus, forming an “eye.” The other more superficial veins are tributaries.
Ultrasonographic imaging shows that the saphenous veins are interfascial veins, demarcated by two connective fasciae, the saphenous fascia and the muscular fascia, and thus are contained in a “saphenous compartment” (Figure 1).4,5
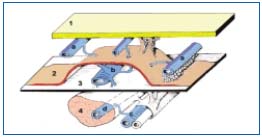
Figure 1. (Adapted from A. Caggiati) The three compartments of
the venous system of the lower limb:
1. the skin
2. the saphenous fascia
3. the muscular fascia
The deep venous system is located in the deep layer, beneath the
muscular fascia: deep trunks (c) and muscular veins (d) inside the
muscles (4). The saphenous trunks (b) are located between the two
layers of fascia in the saphenous compartment (saphenous “eye”).
Tributaries (a) of the saphenous trunks are found under the skin.
Caggiati and Ricci6 have proposed the term “saphenous fascia.” For this reason, the saphenous veins do not fit the classical description of “superficial” veins. This is easily recognized by ultrasound, forming the socalled “Egyptian eye” sign (Figure 2). This concept was validated at a consensus meeting organized at the UIP congress in Rome.7
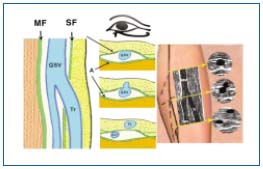
Figure 2. The “Egyptian eye.”
MF = muscular fascia / SF = saphenous fascia / GSV = great
saphenous vein / Tr = Tributary of GSV.
Functional anatomy
The fascial relations of the saphenous trunks suggest that muscular contraction affects their diameter and hemodynamics. In addition, the saphenous fascia acts as a type of mechanical barrier that can counteract pathologic vasodilatation in varicose veins.
The saphenous tributaries and collateral vessels emerge from this space and are devoid of any fascial sheath. In fact, they are unprotected and thus subject to varicose dilatation before the large saphenous trunks are affected.6
Particularities of the small saphenous system
The small saphenous vein (SSV) starts at the lateral malleolus. Running up the calf and back of the leg (Figure 3), shown in orange), the SSV and the great saphenous vein (LSV) (shown in yellow) are located in the “saphenous compartment.”8 But in these areas, the membranous layer (saphenous fascia) is different. It is thick and resistant, appearing more like an aponeurosis (Figure 4). Therefore, the SSV is an interfascial vein.

Figure 3. The saphenous
compartments for the GSV
and the SSV.

Figure 4. Photograph by
C. Gillot: the thick membranous
layer (open) of the SSV (1)
at the upper calf level, showing
the sural nerve (2) and
a medial gastrocnemius
perforating vein (3).
Embryology: theory of “angio-guiding” nerves (Figure 5)
Angiogenesis and neurogenesis are closely interrelated during prenatal development and continue to play a physiological part in postnatal life.9 Evidence indicates that nerves and blood vessels exert reciprocal control over their own growth. For example, “guidance factors,” including vascular endothelial growth factor A (VEGFA), should play a pivotal part in the three-dimensional growth patterns of arteries and nerves.
Three “angio-guiding” nerves in the embryo induce angiogenesis of lower limb veins9,10 along the limb axis:
1. The axial nerve or sciatic nerve (No 1, in yellow). One of its branches, the sural nerve directs development of the SSV.
2. The preaxial nerve becomes the femoral nerve (No 2, in pink).
3. The postaxial nerve (No 3, in white) becomes the posterior femoral cutaneous nerve.
The axial venous plexus (shown in red) participates in formation of the saphenous system. Ventrally, the preaxial venous plexus (shown in blue) becomes the femoral vein and the great saphenous vein. Dorsally, the postaxial venous plexus (shown in purple) becomes the postaxial or dorsal extension of the small saphenous vein.
Thus, capillary blood vessels differentiate along vascularguided nerves and produce several anastomoses, determining the final configuration of the venous system.
The axio-preaxial anastomosis in the thigh forms the emergence pathway for the deep femoral vein. It connects the axial plexus and its popliteal anastomosis dorsally with the postaxial venous plexus. This is the small saphenous vein arch. Ventrally, it connects with the preaxial venous plexus. It is the origin of the popliteal vein. Lastly, Giacomini’s vein represents the posterior anastomosis of the SSV at the root of the thigh.
The SSV and related nerves
The sural nerve (Figure 6) is formed by sensory branches of the tibial and peroneal nerves. It is an axial nerve located below the muscular fascia. It is distant from the SSV in the upper part of the calf, joining the SSV at the apex of the calf.
The sural accessory nerve emerges from the fibular nerve, oblique and anterior to the lateral head of the gastrocnemius muscle, below the muscular fascia.
At the apex of the calf, the sural nerve and its accessory branch join in a common trunk . This nerve can be called the “SSV nerve” because it accompanies the vein down to the ankle.

Figure 6. Photograph by C. Gillot: the SSV arch and the nerves.
(PA: dorsal or postaxial extension of SSV).

Figure 7. Photograph by
C. Gillot: the sural nerve (1)
with its companion vein (2,
in blue), and artery (3, in
orange). The SSV (4, in light
purple) joins the sural nerve
to form a common trunk in the
medial aspect of the popliteal
vein (5). Laterally, note the
accessory nerve (6) joining the
sural nerve at the lower part of
the diagram (apex of the calf).
RELEVANCE OF THESE ANATOMICAL FEATURES
The close proximity of these nerves to the SSV accounts for possible injury to the nerve during certain surgical procedures (invagination, phlebectomies, and endovenous procedures), particularly at the popliteal level and the apex of the calf.
Anatomy of the SSV10
Origin: (Figure 8)
– The SSV arises posterior to the lateral malleolus as a continuation of the lateral marginal vein of the foot, close to its companion (sural) nerve. It rises along the lateral border of the tendocalcaneus and then, crosses to reach the middle of the posterior aspect of the leg. Running upwards, it perforates the deep fascia in the lower part of the popliteal fossa between the heads of the gastrocnemius muscle. It ends in the popliteal vein. The lateral malleolar plexus: the origin of the SSV is often a plexus.
The junction at the apex of the calf provides an exchange for blood flow.
– With its inferior leg tributaries (medial and lateral)
– The distribution pathways of the SSV are:
• The great saphenous trunk or a posterior tributary
• The medial gastrocnemius vein: this is the “vein of the sural nerve”
• The muscular perforator veins in the calf:
■Posterior and superior perforating veins (Gillot) of the medial head of the gastrocnemius
■Apical perforating vein of the lateral head of the gastrocnemius
■Trans-gastrocnemius: soleus perforating veins (lateral)
■Lateral perforating veins of the soleus muscle

Figure 8. Photograph by
C. Gillot: the SSV and the sural
nerve (yellow dot) at the ankle.
Note the thickness of the
fascia layer covering the
structures peeled back
(on the left).
Termination of the SSV
In the popliteal fossa, the small saphenous vein runs a few cm above the popliteal fold to form an anterior arch before terminating in the posterior or posterolateral surface of the popliteal vein.
However, many variations exist, and several types of termination of the small saphenous vein have been proposed based on surgical and echographic findings.
According to a practical and surgical point of view, we described 5 termination types of the SSV11 (Figure 9) according to the presence (A and B) or the absence (C, D, and E) of SPJ:
Type A: Normal SPJ located less than 5 cm above the crease (83%)
• Type A1: without a common trunk with the medial gastrocnemial veins (62%)
• Type A2: with a common trunk with the medial gastrocnemial veins (21%)
Type B: High SPJ, egal or more than 5 cm above the crease (6%)
Type C: No SPJ SSV prolongated by Giacomini vein (5%)
Type D: No SPJ Plexiform deep termination in the thigh muscles (5%)
Type E: No SPJ Short termination at the leg level (1%)
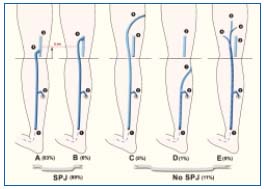
Figure 9. The 5 different types of SSV termination. A, B with SPJ;
C, D, and E with no SPJ.
SSV (1); Calf gastrocnemial perforator (2); Popliteal vein (3);
Normal SSV termination with a low arch (4); High termination
(5); Giacomini vein (6); Short type of SSV ending with
a communicating vein into the GSV (7); Muscular perforators
of the thigh (8); Dorsal or cranial extension of SSV (9).
Venous arch
The existence of a venous arch (french “crosse”) is not a constant finding in normal subjects (70%). It is more common in patients with varicose veins because it is often responsible for a pathological reflux in this area.12 Such a reflux from higher points, the popliteal or deep femoral vein, feeds the superficial network little.
1/ ARCH of the SSV
The SSV terminates in the popliteal vein; the arch of the SSV usually crosses the lateral aspect of the tibial nerve, close to the nerve (Figure 10). The saphenopopliteal junction is located just above the femoral condyle.
The arch of the SSV must be differentiated from the saphenopopliteal junction, the only site of implantation of the SSV in the popliteal vein.
Sometimes (30% of cases) the SSV terminates at a lower level in the popliteal vein, near the femoral condyle. In this case:
– The arch crosses the medial aspect of the tibial nerve.
– The SSV often shares a common trunk with the gastrocnemius veins.
However, the SSV scarcely has a common course with the sural nerve (Figure 7).

Figure 10. Photograph by
C. Gillot: the arch of the SSV
(purple dot) crossing the
medial aspect of the tibial
nerve. The nerve of the medial
head of the gastrocnemius muscle
(yellow dot) crosses
over the termination of the
SSV in the medial aspect of
the popliteal vein. The
gastrocnemius trunk (blue dot).
2/ “DEEP” EXTENSION of the SSV10,13
It is known as an axial extension because it is located dorsally, near the tibial nerve (axial nerve in the embryo). It can join an axial arch (or sciatic nerve arch) which is located ventrally to the sciatic nerve (Figure 11).
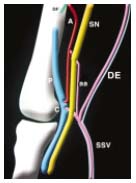
Figure 11. Drawing by
C. Gillot: the dorsal or postaxial
extension of the SSV (PA). A
preaxial vein (A) along the
sciatic nerve (SN), axial nerve
of the embryo and the axial
arch (aa) joining the deep
femoral vein (DF).
P = popliteal vein; SSV = small
saphenous vein; C = arch of
SSV.
3/ “DORSAL” EXTENSION of the SSV
Known as the postaxial or cranial extension of the SSV14,15 (postaxial nerve of the embryo), it is located more superficially, but below the muscular fascia. It accompanies the femoral posterior cutaneous nerve (Figure 11).
It perforates the fascia at various levels, and with Giacomini’s vein16,17 (intersaphenous anastomosis) joins the LSV.
CONCLUSION
The clinician needs to be aware of potentially hazardous areas in treatment of venous disease with SSV approach and procedures. These findings emphasize the usefulness of ultrasonographic mapping prior to an invasive procedure for treatment of chronic venous disease.18,19
1/ At the ankle, the origin of the SSV is often plexiform, located deep below the fascia. The nerve is located very close to the vein, surrounded by fat tissue, often dense and associated with sclerosis, which makes approach to it rather difficult.
2/ In the apex of the calf: this is an area of very high risk and the most hazardous:
– It is the junction of several veins, with risk of perforations or of entering the wrong vein during catheterization.
– Possible existence of a “short saphenous artery” which poses a high risk for injection of a sclerosing agent, due to a highly variable surrounding disposition of this artery. For this reason, ultrasonographically-guided procedures in this area are mandatory.20,21
– The confluence of nerves which perforate the aponeurosis.
– The perforating veins join the gastrocnemius muscles.
3/ In the popliteal fossa, the veins are very close to the nerves:
– The short saphenous arch is close to the tibial nerve, or sometimes the nerve of the medial head of the gastrocnemius muscle.
– The existence of a common SSV trunk with the gastrocnemius veins is always associated with a medial arch of the tibial nerve.
– The axial extension of the SSV is along the tibial nerve and the sciatic nerve.
– The postaxial or dorsal extension is along the posterior cutaneous femoral nerve.
REFERENCES
2. Bailly M. Cartographie CHIVA. In: Editions Techniques Encyclopédie Médico-chirurgicale. Paris. 1995;43-161-B:1-4.
3. Lemasle P, Uhl JF, Lefebvre-Vilardebo M, Baud JM. Proposition d’une définition échographique de la grande saphène et des saphènes accessoires à l’étage crural. Phlébologie. 1996;49:279-286.
4. Caggiati A, Ricci S. The long saphenous vein compartment. Phlebology. 1997;12:107-111.
5. Caggiati A. The saphenous venous compartments. Surg Radiol Anat. 1999;21:29-34.
6. Caggiati, A. Fascial relations and structure of the tributaries of the saphenous veins. Surg Radiol Anat. 2000;22:191-196.
7. Caggiati A, Bergan JJ, Gloviczki P, et al. International Interdisciplinary Consensus Committee on Venous Anatomical Terminology. Nomenclature of the veins of the lower limbs: an international interdisciplinary consensus statement. J Vasc Surg. 2002;36:416-422.
8. Caggiati A. Fascial relationships of the shortsaphenous vein. J Vasc Surg. 2001;34:241-246.
9. Gillot C. Popliteal venous arrangements: hypotheses and certainties. Phlébologie. 1998;51:65-74.
10. Gillot C. Atlas of the Superficial Venous System of the Lower Limb. Editions Phlébologiques Françaises in French and English (CD-ROM multimedia version. Gillot C, Uhl JF in French, English and Spanish, available from the Ganzoni company).
11. Lemasle P, Uhl J-F, Lefebvre-Villardebo M, et al. Confrontation écho-chirurgicale de la terminaison de la saphène externe dans le cadre de la chirurgie d’exérèse: résultats préliminaires. Phlébologie. 1995;48,3:321- 325.
12. Creton D, Kohler F. Is the insufficiency of the short saphenous vein in relation with the level of its anastomosis in the deep vein? Phlébologie. 2000;1:7-12.
13. Gillot C, Uhl JF. Multimedia Atlas of the Superficial Venous System of the Lower Limb (CD-ROM in French, English and Spanish. Ganzoni; In press).
14. Georgiev M. The thigh extension of the lesser saphenous vein: from Giacomini’s observations to ultrasound scan imaging. J Vasc Surg. 2002;37:558-563.
15. Gillot C. Postaxial extension of the short saphenous vein anatomical study, functional considerations, pathological significance. Phlébologie. 2000;3:296-325.
16. Gillot C. The vein described by Giacomini: attempt at systematisation and definition of the terminology of the veins based on embryology and function. Phlébologie. 2001;54:425-429.
17. Delis KT, Knaggs AL. Prevalence, anatomic patterns, valvular competence, and clinical significance of the Giacomini vein. J Vasc Surg. 2004;40:1174-1183.
18. Lemasle P, Baud JM. Value of echomarking in the surgical treatment of varicose veins. Phlébologie. 1992;45:349- 355.
19. Uhl JF, Lefebvre-Villardebo M, Lemasle P. L’écho-marquage pré-opératoire des varices des membres inférieurs: une exploration essentielle pour l’efficacité de la chirurgie d’exérèse. Phlébologie. 1995;48:359-365.
20. Schadeck M. Sclérose de la petite veine saphène: comment éviter les mauvais résultats? Phlébologie. 2004;57:165-169.
21. Creton D. Saphenopopliteal junctions are significantly lower when incompetent. Embryological hypothesis and surgical implications. Phlebolymphology. 2005;48:347-354.
