The white book of venous disease in Spain
Marc CAIROLS1
Josep MARINEL.LO I ROURA2
1. Department of Angiology and Vascular Surgery, Bellvitge Hospital L´Hospitalet de Llobregat, Spain
2. Department of Angiology and Vascular Surgery, Mataró Hospital Mataró, Spain
Chronic venous disease (CVD) is extremely important in Western countries because of its high prevalence, chronic nature, repercussions on quality of life, and complications.1-3 In Spain, there is a high incidence of CVD both in primary care and in vascular surgical departments. Consequently, CVD consumes a high percentage of available resources4 and a large part of the public health budget.
A first step towards improving care for patients with CVD will be to improve our knowledge of different aspects of the management of CVD and to outline foreseeable developments between now and 2010. With this aim in mind, the Spanish Society of Angiology and Vascular Surgery (SEACV) and the Spanish Chapter of Phlebology (CEF) of the Spanish Society have produced the ‘White Book of Venous Disease in Spain’.5
AIMS
The aim of this initiative is to provide human and logistic resources for health care, as well as managers and experts with sufficient, reliable, and rigorous information concerning the health care problems associated with CVD in Spain. Therefore, the aim was not just to describe and explain the current status of the problem, but also to outline foreseeable trends over the next three years.
The analysis covered risk factors and populations at risk, main consultation complaints, diagnostic methods, guidelines for prevention, therapeutic strategy and its compliance, cost/benefit of treatments, predictable trends in terms of care and repercussions on quality of life, and lost working time.
MATERIALS AND METHODS
The prospective Delphi study “Chronic Venous Disease: impact on the Spanish Health Care System. Perspectives for 2010. A prospective macro study using the Delphi method” was performed from the beginning of October 2003 until the end of May 2004. It involved the following steps:
1. Creation of a scientific evaluation committee. The committee included 18 specialists from the SEACV and the CEF, and its task was to draft the essentials of the Delphi questionnaire.
2. Desk research. During this phase, documentation was collected and analyzed, together with available studies on the same topic, in order to define the study framework.
3. Preliminary study comprising:
• Qualitative study involving 30 in-depth interviews with various experts from the health care sector
• Three opinion polls conducted among 100 specialists in angiology and vascular surgery, 150 primary care doctors, and 50 patients in whom CVD was diagnosed
4. Prospective Delphi study. The study was based on the Delphi method,6-8 which involved collection of quantitative (numerical) information to use in modeling trends in various aspects of CVD up to the year 2010: epidemiology, disease development, health care and health care policy and, in particular, treatments, based upon assessments made by a group of highly qualified experts.
The prospective Delphi study was carried out in both public and private community services (17 autonomous communities).
RESULTS
1. EPIDEMIOLOGICAL ASPECTS
The prevalence of CVD is high in the Spanish population. The increase in its incidence in recent years reflects two trends. One rather unfavorable trend is related to population aging, increases in obesity and sedentary lifestyles, work involving prolonged periods of standing or sitting, and so forth, all factors known to increase the incidence of CVD. The other trend is more favorable and is seen in increasing awareness of the need to adopt healthy lifestyles, greater attention to diet and the body, and more exercise.
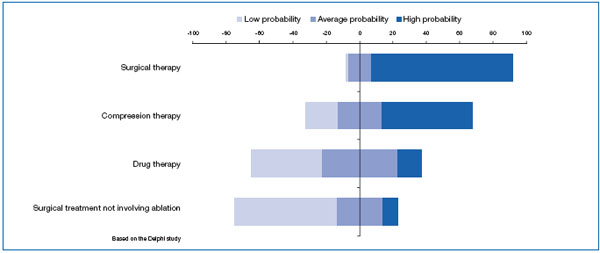
Despite this ambivalent situation, the Delphi study experts consider that the rate of prevalence of CVD will tend to increase as we approach 2010. This increase will affect both sexes, although it will be greater among women. In younger people (under 25 years), the prevalence of CVD will remain stable, but will tend to increase among the rest of the population, particularly in those aged over 45 years (Figure 1).
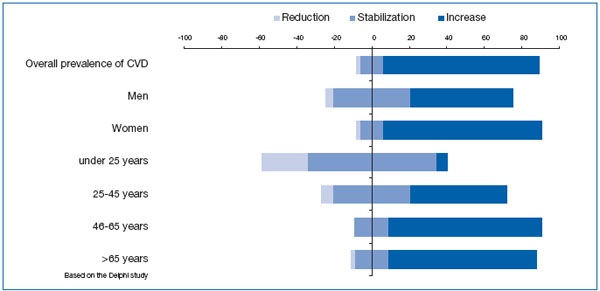
Figure 1. Trends in the prevalence of CVD between now and 2010 according to the Delphi study experts.
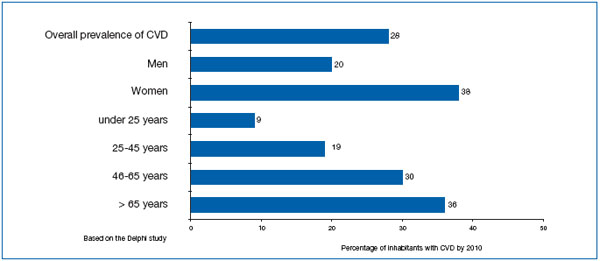
Figure 2. Estimated prevalence of CVD per 100 inhabitants by the year 2010.
In absolute numbers, the experts predicted that the prevalence of CVD per 100 inhabitants in Spain will be 28% by the year 2010. Prevalence will increase considerably more among women (38%) than among men (20%), and it will also be higher in subjects aged over 65 years (36%) whereas in those aged between 46 and 65 years it will be higher (30%) than among 25- to 45- year-olds (19%) (Figure 2).
Ninety-three percent of Delphi study experts considered that CVD is currently undiagnosed in a large percentage of the population. No change is expected in this percentage.
Among the various risk factors for CVD, the most important in the years ahead are overweight, old age, and jobs involving risk (ie, long periods of standing or sitting or exposure to heat). Of less importance are sedentary lifestyle, female gender, prolonged standing, and prolonged sitting. Other important risk factors (although less frequently evaluated than those given above) are heat, oral contraceptives, and genetic predisposition.
Knowledge of the risk factors that will be important in the future is essential if we are to draw up prevention policies and thereby reduce the incidence and prevalence of CVD.
2. PREVENTION OF CVD
Some CVD risk factors cannot be modified, such as age, gender, and genetic predisposition, but most can, particularly those related to lifestyle. A wide range of corrective actions and policies may be implemented:
• prevention campaigns in primary care
• training programs for general practitioners
• early diagnosis campaigns in primary care
• mass media information campaigns for the general population
• promotion of lifestyle changes among the population (eg, increased physical exercise, avoidance of obesity), and
• promotion of the prevention of risk factors at work
The Delphi study experts consider that all of these preventive actions and policies will have been introduced to a certain degree by the year 2010. However, it is difficult to evaluate the efficacy of such
Primary care plays a key role in prevention, as general practitioners are the main source of information for the population at large about the control of CVD risk factors. In addition, the experts also feel that the presence of angiologists and vascular surgeons in primary care centers will greatly improve prevention of CVD. As we know, the specialties dealing specifically with treatment of CVD are currently only available in hospital settings.
3. DIAGNOSIS OF VENOUS DISEASE
During the initial stages of CVD, the symptoms do not affect quality of life, and so patients tend to avoid consulting a doctor. Delays in diagnosis and initiation of treatment ensue, with all the consequences that this entails. It is therefore advisable to recommend early diagnosis of CVD to allow early initiation of treatment so as to improve patients’ quality of life.
The preliminary study clearly shows that the diagnostic methods most widely used today are clinical and physical examination, together with Doppler ultrasound investigation. According to the Delphi study’ experts, these will continue to be the most important tests for detection of CVD in the coming years. In addition, continuous-wave Doppler ultrasound or hand-held Doppler devices will continue to be used much as they are today, while plethysmography, leg volumetry, and phlebography will become less important.
4. TREATMENT OF CVD
The Delphi study experts estimate that around 57% of patients diagnosed with CVD will be on some form of treatment by the year 2010. This percentage is low compared with the results of the preliminary study in which vascular surgeons estimated that 76% of patients with CVD are currently receiving treatment. This discrepancy is probably due to undertreatment of such patients by primary care physicians, who underestimate the importance of the disease.
Compression therapies will become more widespread as 2010 approaches, as will hygienic and postural measures, and changes in lifestyle. Although less marked than for the above measures, increases are also anticipated in surgical procedures, drug treatment and sclerotherapy. Use of surgical procedures not involving ablation is not expected to change, but topical treatment will tend to decline.
In terms of the period of treatment, 85% of experts consider drug therapy should be given in the summer (when symptoms are more acutely felt and patients are less tolerant of compression hosiery), 75% when symptoms appear, 61% intermittently in periods of two to three months, and 25% continuously. In addition, 85% of experts stated that compression therapy should be used continuously, while 74% feel it should be used only when symptoms become apparent (Figure 3).
One aspect of drug treatment for CVD that will tend to affect the future of therapy is the education of patients regarding their treatment.
As we approach the year 2010, improvement in symptoms (pain, heavy legs, swelling, cramp, etc.) and signs of venous disease, together with patients’ quality of life, will be the most important criteria affecting choice of venotonic drugs in the treatment of CVD. Much importance will also be attached to the following criteria: funding by the Spanish social security system, drug safety, patient convenience (facilitating compliance), acceleration of healing of venous ulcers and dosage (once a day preferred).
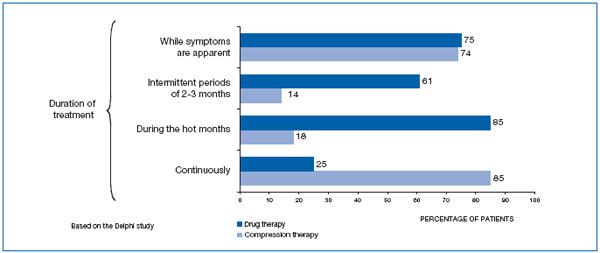
Figure 3. Most accurate periods for drug and compression therapy, according to the experts.
So far, compression therapy, drug treatment, surgery, and surgical procedures not involving ablation, such as radiofrequency, are financed by the Spanish National Health System. In the view of the experts, it is highly likely that surgical treatment will continue to be funded in this way in the year 2010, and they also feel that compression therapy may possibly be financed. In contrast, there are doubts about continued funding for drug treatments and, above all, it is unlikely that funding will continue for surgical methods not involving ablation (Figure 4).