IV – INVESTIGATIONS AND HEMODYNAMICS
VENOUS DISORDERS
Venous and lymphatic disorders: noninvasive investigations
Chairperson: Z. Rybak (Poland)
Knee perforating veins as a source of varicosities: prevalence and clinical relevance
M. V. L. BARROS (Brazil)
The authors studied the incidence of anterior knee perforating veins (PV) in 752 patients using Duplex scanning.
They found out that almost 5% of patients with varicose veins had such incompetent perforators that provoked reflux in the leg in anteromedial and anterolateral collateral veins or a great saphenous vein local insufficiency in the calf.
These perforating veins were usually small in diameter and not associated with severe disease.
Duplex investigation of the lesser saphenous vein
R. MORETTI (Italy)
The author described his experience studying the small saphenous vein with Duplex Scanner, and reported high incidence of asymmetric origin.
Most veins originated from the popliteal vein or the lower third of the thigh, and one out of five patients had multiple connections.
Noninvasive venous pressure measurement by controlled compression sonography
C. THALHAMMER (Switzerland)
Information about increased venous pressure is useful in many clinical situations, but is rarely used because it is invasive, requiring venous puncture. Using a manometer that is transparent to ultrasound, the compression is exerted by the probe on the tissue and the underlying veins until they collapse could be measured. Applying such a manometer to the probe of their duplex scanner, the authors were able to accurately measure, noninvasively, venous pressure in the arm, where for experimental purposes, the pressure was artificially increased.
Venous and lymphatic disorders – conventional and nonconventional ultrasound
Chairpersons: G. Botta (Italy), A. Lechter (Colombia)
Hyperflow conditions new concept in venous diseases
N. A. NAZARE CASTRO, S. SALLES CUNHA, T. PINHO NAVARRO (Brazil)
This observational study describes the presence of a spontaneous cephalad flow (hyperflow or overflow) without compressing the calf in the Giacomini vein due to an insufficiency in the saphenopopliteal junction. In these cases, the incompetence of deep venous system is transmitted to the superficial system throughout the Giacomini vein, causing some cases of recurrent varicose veins.
Ultrasonography diagnosis of recent venous thrombus: experimental study in dogs
M. G. GIANNINI, H. A. R. ROLLO, F. H. A. M. MAFFEI (Brazil)
In the authors’ opinion the ultrasound study by power Doppler, B flow, and harmonic tissue imaging of a recent thrombus created surgically in the inferior vena cava of dogs in this experimental study offers greater sensitivity, specificity, and accuracy than phlebography studies. Currently in the medical literature, the majority of comparative studies between ultrasound and phlebograpy for the diagnosis of acute deep venous thrombosis suggests that phlebography is the more accurate.
3D CT venography to investigate the venous system: value and results for assessment of congenital malformations and varicose veins
J. F. UHL, C. GILLOT, V. DELMAS, O. PLAISANT, O. AMI (France)
The authors presented a most impressive reconstruction of three-dimensional CT venous studies of patients with complex venous disorders. The possibility of rotating the images and suppressing muscles and other structures offers a very clear and understandable image of the venous system. These anatomic studies should be combined with hemodynamic information for a better understanding of venous disease.
On-table varicography is still a useful investigation in the treatment of varicose veins
J. T. HOBBS (UK)
The ultrasonic study is the gold standard in the study of varicose veins disorders, but the equipment is expensive and not universally available. In inexpert hands ultrasonic studies cannot recognize significant reflux. In complex venous disorders (vulvar veins, recurrences, and a complex pattern of veins of the poplitea fossa) on-table varicography is a very helpful. On-table varicography investigation demonstrates correctly complex venous anatomy disorders with the injection of a nonionic contrast directly and taking a simple X ray with basic equipment, which is available everywhere.
Hemodynamics of the saphenofemoral junction, patterns of reflux, and their clinical implications Relationship between the caliber of the greater saphenous vein and the competence or absence/incompetence of the femoral valve in subjects with incompetence of the saphenofemoral junction
M. CAPPELLI, R. MOLINO LOVA, S. ERMINI, P. ZAMBONI (Italy)
The disconnection of the saphenofemoral junction in cases of femoral vein insufficiency has a high percentage of recurrences. To correctly study venous reflux in the saphenofemoral junction it is necessary to record venous flow on the side of the femoral vein using power Doppler. The study of venous flow at this level can offer prognostic information regarding crossectomy.
In the second presentation the author demonstrated the relationship between great saphenous vein diameters and femoral vein competence/incompetence studied by ultrasound in patients with saphenofemoral junction insufficiency. In cases of femoral vein incompetence the great saphenous vein will increase its diameter.
The sub diaphragmatic IAP: physiologic classification and instrumental test
Chairpersons: E. Brizzo, (Argentina), C. Belczak (Brazil)
Propellent-suction pumps phlebographic assessment: plantar, gemelar, gluteal and pelvic
S. ZUBICOA EZPELETA (Spain)
One hundred and twenty-one patients were studied in order to evaluate the plantar and gemellar pumps by means of dynamic ascending phlebography. The examinations of the gluteal and pelvic pumps were performed with selective phlebography with catheterization from a vein at the elbow, canalizing the gluteal veins and other pelvic tributary branches. The authors also registered measurements of ambulatory venous pressure.
They concluded:
Plantar and gastrocnemial pump
1. In the case of the plantar pump activation (loaded foot) the emptying of the plantar arch which drains by the posterior tibial veins, is almost complete.
2. In patients with malformation (flat feet) the emptying in the plantar arch is scarcely noticeable.
3. The hallux flexo-extension movement also shows the unloading of the internal plantar vein, although slower and less complete than with the heel step.
Gluteal pumps
1. Although the interconnected abdomino-pelvic venous system makes up a functional unit, gluteal pumps actively participate in the return circulation, experiencing with the gluteal muscle contraction a slight increase in the emptying velocity and reduction in the vein caliber.
Functional unit
J. LEAL MONEDERO (Spain)
1. The veins of the abdomen, pelvis, and lower limbs make up the subdiaphragmatic functional unit.
2. The pelvic venous system works in a way related to that of the lower limbs, but they present a different pumping hemodynamic and valvulating system.
3. The impulse-aspirative pumps need to perform their role in the valvular system which acts as a compartment.
4. These valvular systems can be internal and external.
5. For the diagnosis and treatment of the venous pathology in the pelvis , the knowledge of the type of the pathology which has created this alteration in the centripetal-centrifugal flow is vital.
6. The infra-diaphragmatic vascular rehabilitation should not only be performed in the lower limbs (plantar, sural, popliteal-gastrocnemial), but also in the pelvic floor, as well for as the abdominal wall and breathing.
Compression and its efficacy on the venous pump
H. PARTSCH (Austria)
In the presented paper measurements of interface pressure and stiffness of compression stockings and bandages, using mainly the MST tester and the Kikuhime transducer, were performed. The authors described the effects of stockings and bandages on venous diameter (n=26), venous reflux (n=21), expelled volume and on ambulatory venous hypertension by means of duplex, air plethysmography, foot volumetry, and phlebodynamometry. Although the interface pressure on the distal lower leg in the supine position may go as high as 40 mm Hg with a class III-stocking and also with a short-stretch bandage, so during standing and walking a material with high stiffness (stretch bandages, zinc-plaster) will produce pressure peaks of 70 mm Hg or more. This allows the occlusion of the veins intermittently during walking. The authors concluded that, although the use of compression stockings is the method of choice in patients with chronic venous disease, multilayer compression bandages have a superior effect on the disturbed venous hemodynamics to stockings, because the latter compress the leg veins in the upright position only to a minor extent.
Duplex color ultrasound venous assessment in pelvic chronic venous insufficiency
A. SÁNCHEZ GUERRERO (Spain)
To prove the usefulness of pelvic venous ultrasound (transparietal and transvaginal) in subdiaphragmatic chronic venous insufficiency the authors compared angiographic findings (iliocavography with pressure measurements) with the data obtained with the echographic assessment with color duplex. The authors studied patients with ultrasound investigations suggesting a picture of pelvic venous insufficiency during the last 3 years. The authors emphasized the ability of duplex ultrasound to differentiate normal subjects from pathological ones, and among these to distinguish centripetal hemodynamic pictures (venous obstruction, May Thurner, nutcracker) from centrifugal (gonadal and/or hypogastric insufficiency).
Development of reflux in the perforator veins
N. LABROPOULOS, A. BHATTI, L. LEON, A. K. TASSIOPOULOS (USA)
The aim was to describe the mechanisms by which perforator vein (PV) reflux develops in patients with primary chronic venous disease (CVD), patients with CVD who had had at least two duplex ultrasound (DU) examinations prior to any treatment were included in the study. All affected limbs were classified by the CEAP system. Reflux was induced by distal limb compression followed by sudden release using rapid-inflation pneumatic cuffs, and by dorsiplantar flexion. The perforator vein reflux was divided into ascending and des-cending types (re-entry flow) and those developed in new locations, which did not have reflux in any system. There were 29 limbs in 26 patients with reflux development in the PV. In total 38 new incompetent PVs were identified. The median time of the examination was 25 months (range 9 to 52).
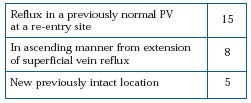
Anatomic location of the new incompetent perforators:
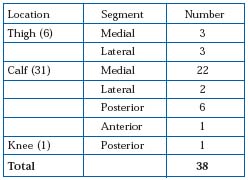
Worsening of clinical class was observed in 11 limbs:
– 7 from Class 2 to 3 or 4
– 2 from Class 3 to 4
– 2 from Class 4 to 6
The authors concluded:
1. Reflux in perforating veins develops in ascending manner through the superficial veins
2. Worsening of CVD is observed with new PV reflux but many other factors play a major role. A causative association is difficult to prove.
LYMPHATIC DISORDERS
Venous and lymphatic disorders: noninvasive investigations
Chairperson: Z. Rybak (Poland)
Accuracy of continuous wave Doppler in lower limb venous examination
J. FARRAH (UK)
Continuous-wave Doppler (CWD) is still used in many practices to assess patients with varicose veins.
To assess its validity, the authors studied 101 varicose patients with CWD and with Duplex Scanning, on the same day with different “blind” operators. They showed that CWD is reliable in studying the saphenofemoral junction, but it is of little value in studying recurrent varices and other parts of the venous system, so a Duplex Scanner examination is recommended before surgery.
EDEMA
The swollen leg
In the framework of the JOBST symposium.
Chairpersons: H. Partsch (Austria), M. Goldman (USA)
Clinical differential diagnosis of the swollen leg
H. PARTSCH (Austria)
Edema is the main symptom of various diseases. It is the symptom of underlying pathology but not of a particular diagnosis. Edema is a visible and palpable swelling caused by an increased fluid content of the interstitium. Depending on the underlying pathology it can be unilateral or bilateral (Table I).
It is very important to exclude malignant lymphedema of the limbs. For example, unilateral lowerlimb edema may be a sequel of compression of the iliac vein by a tumor. Edema of the left leg can be provoked by the pelvic spur due to compression of the left iliac vein by the right iliac artery. There are some rare causes of leg edema. For example, edema due to depression immobility or pretibial myxedema (EMO syndrome: exophtnalmus, myxedema, osteoarthropathy). Arm edema is often due to mastectomy with lymph node resection.
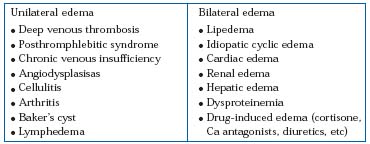
Table I. Differential diagnoses of swollen limbs.
Dermatologic manifestations of the swollen leg
M. GOLDMAN (USA)
The main dermatological manifestations of the swollen leg are:
1. Edema
2. Hair loss
3. Stasis dermatitis
4. Hyperpigmentation
5. Lymphostasis verrucosa cutis
6. Lipodermatosclerosis
7. Ulceration.
The leg edema is characterized by pitting and erythema, and is susceptible to infection. The basic treatment of this condition must include:
1. Treatment of the underlying cause
2. Exercise/physical therapy
3. Lymphatic massage and endermology
4. Intermittent pneumatic compression
5. Graduated compression stockings
6. Diuretics (special indications).
Localized alopecia is due to decreased oxygenation of the tissue, venous hypertension, and dermatosclerosis.
Stasis dermatitis is often associated with swollen legs and is remarkable due to pruritus and lichenification. The basic treatment of stasis dermatitis must include correction of the venous hypertension, compression, bland ointment, and lowpotency topical corticosteroids.
Pigmentation is caused by extravasation of the RBC, perivenulitis and inflammation. Hyperpigmentation can be treated with graduated compression, retinoic acid, deferoxamine, and laser. Characteristic features of lipodermatosclerosis are:
• Chronic inflammation
• Calcium deposits
• Fibrous, indurated skin.
Lymphostasis verrucosa cutis is one of the more severe complications of the swollen leg. This syndrome is caused by chronic edema, chronic stasis changes, and recurrent infection. The treatment of the lymphostasis verrucosa cutis must include:
1. Exercise/physical therapy
2. Lymphatic massage
3. Intermittent pneumatic compression
4. Graduated compression stocking
5. Whirlpool debridment
6. Prevention of infection.
Ulceration is the final stage of CVI and swollen limb. Adequate and prompt treatment is necessary. Sometimes it can progress to malignancy.
Classification and investigation of the swollen limb
K. G. BURNAND (UK)
Lymphedema is edematous swelling of a region of the body as a result of defective lymphatic drainage. There are two forms of lymphedema:
Primary (75% female, 25% male)
• Congenital (11%)
• Praecox (precocious) (75%)
• Tarda (late) (14%).
Secondary
The main causes of secondary lymphedema are trauma, iatrogenic (block dissection), infection (filiariasis, cellulitis), inflammation (rheumatoid, eczema), malignancy, and irradiation. Investigation of patients with lymphedema usually includes clinical examination, venous tests (duplex), isotope lymphography, contrast lymphography, ECG, echocardiography, genetic analysis and some laboratory tests (albumin, urea, creatinine). Isotope lymphography is a gold standard for outpatient investigation of lymphedema. Differential diagnoses of lymphedema are necessary for dealing with cardiac, renal, and hepatic failure, hypoproteinemia, fluid retention syndromes, venous edema, hysterical edema, factitious edema, eythrocyanosis frigida, lipoidosis or lipodystrophy, postarterial reconstruction, gigantism, and arteriovenous fistulas. In conclusion, the author has underlined the necessity of a new classification of the lymphedema.
THROMBOSIS
Thromboembolic pathology
Chairpersons: R. Gesto (Spain), J. Chunga-Chunga (Peru)
Nutcracker syndrome: echographic diagnosis with color duplex ultrasound
A. SÁNCHEZ GUERRERO (Spain)
Significant left renal vein compression in the aorto-mesenteric entrapment, or Nutcracker syndrome (NS), is less well-known than other compressive syndromes as the subclavian steal syndrome or May-Thurner syndrome, also related to anatomical narrowing. More frequently it is described in the literature by its urological manifestations secondary to renal venous hypertension, which is a common cause of pelvic and scrotal varicocele and even of lower-limbs varicose veins, although not usually diagnosed. It is also a cause of failure and recurrence of the previously treated varicocele.
Sixteen patients (15 female and 1 male) diagnosed with NS by color duplex ultrasound and confirmed by hemodynamic studies were compared with a control group of four patients (all female). In all patients – from both groups – the pressure gradient was estimated after additional phlebography. The results obtained were surprising. The average velocity ratio between the aorto-mesenteric entrapment area and the pre-entrapment area was 11.20 (13.89-5.6) in the group with NS compared with 2.25 (1.29-3.24) of the control group.
The diameter ratio between the renal vein in the aorto-mesenteric entrapment area and the preentrapment area was 6.45 (4.46-8.13) in the NS group compared with 1.96 (1.33-2.67) in the control group. In the 62% with NS, continuous flow inversion in the left gonadal vein was observed, opposed to none in the control group. The patients with NS presented pelvic varicocele with average diameter of venous lakes of 7.6 mm (14-5) with velocity of high spontaneous flow average 9.6 cm/seg opposed to none in the control group (diameter of the venous lakes 4 mm) with spontaneous average velocity of 0.75 cm/seg. About 94% of patients (n=15) with NS presented a hypogastric vein with centripetal flow, except one patient, due to the presence of an associated May-Thurner syndrome. The left average cavo-renal pressure gradient was 4.37 mm Hg in the NS group as opposed to 0.75 in the control group.
It seems that CDU could be an excellent method of choice in the diagnosis of NS. The diagnostic criteria are simple:
– the presence of a ratio of velocity or diameter >5
– continuous flow inversion in the left gonadal vein or pelvic varicocele (venous lakes >5 mm) with high velocity of spontaneous flow (>4 cm/ seg) with a hypogastric vein with flow in a centripetal direction.
PELVIC SYNDROME
Venous pathology in the female pelvis
Chairpersons: J. Leal Monedero (Spain), C. L. S. Figueiroa (Brazil)
Pelvic venous insufficiency pathophysiology: centrifugal and centripetal syndromes
J. L. MONEDERO (Spain)
One cannot diagnose a disease if one does not know that it exists, and Dr Monedero suggests that for pelvic chronic venous insufficiency (PCVI), this is often the case.
At the pelvic level, venous syndromes can be due to two causes: one is an increase in centripetal pressure, when there is an obstruction to blood flowing toward the heart, like in nutcracker syndrome (left renal vein entrapment by aorta and mesenteric artery), May-Thurner syndrome (left iliac vein compression by right iliac artery), malformations such as double cava vein, or compression due to tumors or other causes. The other is an increase in centripetal pressure, for general causes like heart failure, or local venous insufficiency, mainly in gonadal, hypogastric, and gluteal veins.
Knowing that PCVI exists can help clinicians to correctly diagnose many atypical varices.
PCVI etiological and triggering factors
C. L. S. FIGUEIROA (Brazil)
The author suggests that pain in PCVI can be caused by a neurological insult due to venulo-capillary hypertension.
Treatment by embolization of the pelvic vein insufficiency in women presenting with nonsaphenous perineal veins – anatomic and clinical correlation: 2-year follow-up
D. CRETON (France)
Pelvic vein syndrome includes pelvic heaviness, bladder irritability and urgency, constipation, vulvar varices, and haemorrhoids. It provokes three precise clinical signs: pelvic and varicose pain just before or during the menstrual period, and dyspareunia just after intercourse. Associated varicose veins are often perineal veins, perforators on the buttock, and more rarely the sciatic vein.
Using an analog visual scale for the three signs, with a cumulative maximum score of 30, the author found that in women of reproductive age suffering from PCVI the mean score was almost 14, and that after treatment with embolization, 67% of the patients improved more than 80%, with results stable for up to 2 years, but to obtain these results it was necessary to perform wide embolizations, that involved both ovarian and hypogastric veins. Such good results are not confirmed in menopausal women, whose symptoms usually do not improve with treatment.
The main message of this section is that if you are confronted with atypical varices, especially in patients with pelvic pain and dyspareunia, you must look for pelvic venous insufficiency and that if such a situation is detected, it can be corrected with effective and non-aggressive treatments.
