Is it essential to treat the AASV during thermal ablation of the GSV?
Jean-Luc GERARD, MD;
Clinique du Mont-Louis, Paris
Clinique Geoffroy Saint-Hilaire, Paris
Abstract
Recent decades have experienced the substantial development of endovenous techniques to treat varicose veins. Such techniques are guided by ultrasound through use of increasingly efficient equipment, and operators have become better trained. This, in parallel with the study of cadaver dissections, has led to a marked improvement in the knowledge of vein anatomy in the lower limbs. The treatment of varicose veins has always been known for its risk of recurrence, which can have several origins. The most widely accepted cause right now is recurrence attributed to the anterior accessory saphenous vein. But the anatomy of this vein, when it’s present, varies greatly from one patient to another, even from one limb to another. Apart from open surgery, phlebologists and vascular surgeons use different treatments for varicose veins. These mainly include endovenous thermal ablation (EVTA, by laser or radiofrequency), sclerotherapy (liquid or foam), and cyanoacrylate closure. All those procedures are ultrasound guided. The goal of this article is to discuss the pertinence of a preventive treatment for an accessory anterior vein when that vein is competent and when it’s practically feasible.
Introduction
The role of the anterior accessory saphenous vein (AASV) in recurrence of varicose veins after treatment of the great saphenous vein (GSV) seems to persist, even if recurrence is decreasing with mostly using minimally invasive endovenous ablation techniques—endovenous laser ablation (EVLA) or radiofrequency ablation—instead of surgical treatment (recurrence rates reported vary, eg, 43%1 to 8%-35%2-4).
Formerly, surgical ligations of the saphenofemoral junction (SFJ) were often used to treat the AASV even when it was competent. Nowadays, preoperative duplex scanning allows better visualization of the SFJ, and the minimally invasive endovenous ablation techniques are precise and done under ultrasonographic control. Phlebologists and vascular surgeons are often keen to protect the functional portions of the SFJ when possible.
In 2019, Marianne De Maeseneer, in an article in Phlebolymphology entitled “What a phlebologist should know about the anterior accessory saphenous vein,”5 concluded that the AASV is “the eternal culprit” in varicose veins after surgery and endovenous ablation.
The cause of those recurrences might be the persisting incompetence of the SFJ after EVTA.5
In 2020, Baccellieri and colleagues, in International Angiology,6 reported on the variable AASV anatomy at the SFJ as a possible risk factor for recurrent varicose veins after GSV radiofrequency thermal ablation. Their results showed that direct confluence of the AASV at the SFJ was a negative predictor of a recurrent varicose vein after 1 year and suggested that SFJ morphology could influence their formation; in particular, the authors suggested that concomitant incompetence of the AASV or direct confluence of the AASV at the SFJ could be an indication for simultaneous treatment by nonsurgical techniques (FTA or laser), while avoiding surgical ligation.
According to Garcia-Gimeno and colleagues,7 the SFJ of the GSV is involved in 65% of all varicose vein disease and the isolated AASV is responsible for 10.9%.
Whiteley and colleagues, in 2008,8 described in a retrospective review of a 2-year period including 1686 local anesthesia procedures that 29% of those undergoing thermoablation of the GSV also required treatment of the AASV, suspected to be due to an incompetence of the AASV (incompetence defined as a reflux greater than 0.5 seconds on an erect patient after manual calf compression, with the AASV inducing a “sump effect” [siphon effect] when enlarged with no reflux found).
In December 2021, an article published in Phlebology entitled “A systematic review and meta-analysis of treatment modalities for [AASV]” reported on an analysis of 860 articles. The authors concluded that it is “safe and effective” to treat AASV incompetence and suggested use of thermal ablation or cyanoacrylate, and maybe phlebectomy when the SJF is competent.9
Everyone seems to agree that treatment of the AASV is pertinent when incompetent. It causes similar disease severity and morbidity to that caused by the incompetence of the GSV.10
Following a promising case series published in 2021 entitled “Feasibility and potential significance of prophylactic ablation of the major ascending tributaries in EVLA of the great saphenous vein: a case series,”11 there is a multicentered, prospective, controlled German study12 including 1150 patients currently comparing the benefit on varicose recurrency afforded by preventive ablation of a competent AASV at the same time as the ablation of the incompetent GSV. For a 5-year follow-up, 2 groups—with and without AASV preventive ablation—will be compared with regard to rate of varicose recurrence and main complications.
However, the AASV is present in only 41% of people and responsible for varicose vein disease in less than 11%.7 Is this culpability in varicose vein recurrence a good enough reason to treat every AASV, even when competent?
Anatomy of the saphenofemoral junction
The anatomical nomenclature published by Caggiati and colleagues in the Journal of Vascular Surgery in 2005 stated that the AASV “at the upper thigh courses deeply (superficial to the muscular fascia, like the GSV) to a hyperechoic fascia that resembles the GSV covering. However, the [AASV] can be easily identified, because it courses more anteriorly with respect to the GSV, with a path corresponding to that of the underlying femoral artery and veins.”13
There are a lot of different possibilities for connection of the AASV to the femoral vein, passing by the SJF or not, which can explain the recurrence after endovenous ablation procedure (Figures 1 and 2).14
Below the femoral triangle, the “AASV is not only a tributary of the [SFJ], but it is one of the saphenous trunks, situated in its own saphenous compartment in the thigh, lateral to the [GSV]” says Marianne De Maeseneer,5 at least the uppermost centimeters of the thigh. Under that, when incompetent, there is often a subcutaneous segment, visible to the naked eye, corresponding to varicose vein.
Muhlberger15 carried out a study on the cadaver dissection of the last 25 cm of the GSV in 217 legs. It considers as major tributaries flowing into the last centimeters of the GSV the following (Figure 315): i) the lateral pudendal vein, present in 90% of cases; ii) the superficial circumflex iliac vein, found in 83% of cases; iii) the superficial epigastric vein, present in 78% of cases; and iv) anterior and posterior accessory saphenous vein of the GSV (less frequently observed) in 51% and 68% of cases, respectively.16
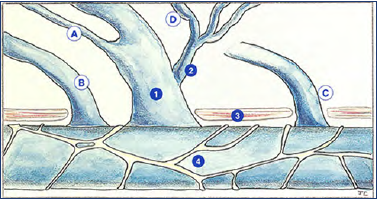
Figure 1. Schematic representation of connections for accessory saphenous vein. 1, saphenofemoral junction; 2, first tributary; 3, aponeurosis; 4, common femoral vein; A, anterior accessory saphenous vein draining in the saphenofemoral junction; B, anterior accessory saphenous vein draining directly into the common femoral vein below the saphenofemoral junction; C, anterior accessory saphenous vein draining directly into the common femoral vein above the saphenofemoral junction; D, anterior accessory saphenous vein draining into a tributary of the saphenofemoral junction. Reproduced from reference 14: Saphènes accessoires. Phlebologia. https://www.phlebologia.com/fr/la-jonctionsapheno-femorale/saphenes-accessoires/ © 2022, Les Laboratoires Servier.
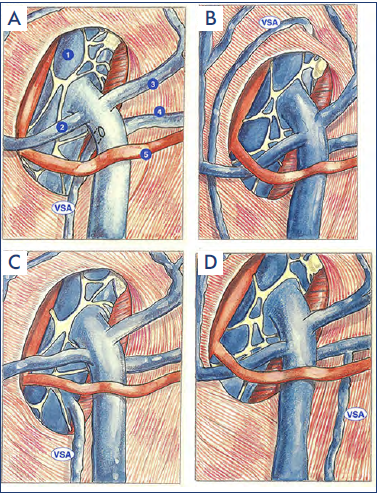
Figure 2. Schematic representation of different types of accessory saphenous vein junctions. A) Abutment in the internal saphenous arch. 1, common femoral vein; 2, PEV, superficial external pudendal vein; 3, EpiV, superficial epigastric vein; 4, circumflex iliac vein; 5, inferior pudendal artery. B) Abutment in the common femoral vein below the saphenous arch. C) Abutment in the common femoral vein at a distance from the saphenous arch. D) Confluence in a collateral vein of the internal saphenous arch. Abbreviation: VSA, anterior accessory saphenous vein. Reproduced from reference 14: Saphènes accessoires. Phlebologia. https://www.phlebologia.com/fr/la-jonctionsapheno-femorale/saphenes-accessoires/ © 2022, Les Laboratoires Servier.
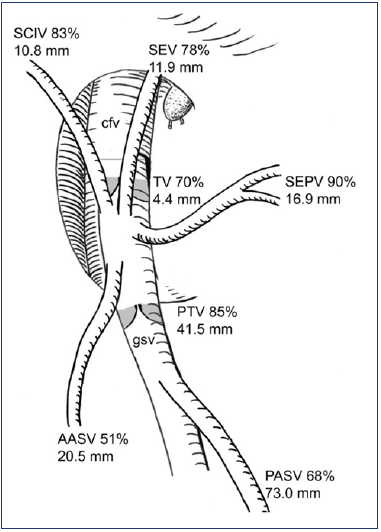
Figure 3. Saphenofemoral junction. Abbreviations: AASV, anterior accessory saphenous vein; cfv, common femoral vein; PASV, posterior accessory saphenous vein; PTV, preterminal valve of the great saphenous vein; SCIV, superficial circumflex iliac vein; SEPV, superficial external pudendal vein; SEV, superficial epigastric vein; TV, terminal valve. Reproduced from reference 15: Mühlberger et al. J Vasc Surg. 2009;49(6):1562-1569. © 2009, Society for Vascular Surgery. Published by Mosby, Inc. all rights reserved.
Those examinations revealed that the terminal valve (TV) was “present between SFJ and first tributary in 70% of cases.”17
Anwar and colleagues describe that reflux at the SFJ would be transmitted “into GSV and its major tributaries causing them to be incompetent in 23% of cases and develop into varicosities. Furthermore, major tributaries enter into GSV within the first few millimeters and may not be treated during endovenous ablation and can cause recurrent varicose veins in the future.”17
There is another important anatomical variability: the femoral valve, which is located in the common femoral vein, above the SFJ. For Capelli,18 when this femoral valve is not present (20% to 24% of cases) or is incompetent, with terminal and preterminal valves also incompetent, the indication for a surgical ligation is obvious. But this assertion is not confirmed in practice: there is no more recurrence after chemical or thermal ablation, no matter the status of these 3 valves.
We note that the anatomy of the veins in the lymph node at the groin has been described by Uhl et al,19 with no history of surgery. Those veins are described as connecting to the femoral vein via direct perforators and joining the GSV and/ or AASV.19
Thermal ablation procedure
Improvement in knowledge of the venous anatomy was made possible by the substantial development of EVTA over the 20 last years.
Indeed, these treatments make it possible to occlude a single incompetent vein, often a single saphenous axis (mainly great or small saphenous vein). One of the advantages of ultrasound-guided thermal occlusion is its precision: the tip of the fiber is perfectly visualized, and we know how to perform a treatment over a precise length, with no overflow. It is therefore possible to treat the entire junction (thermal ligation of the SFJ) or part of it, leaving the competent tributaries free.
The tip of the fiber should be positioned precisely between the termination of the GSV into the femoral vein, including the termination of the AASV when present. This is feasible without technical difficulty via ultrasound-guided endothermal procedures, as the tip is quite echogenic (Figure 4). The occlusion takes place precisely where the tip of the fiber has been positioned (Figure 5).
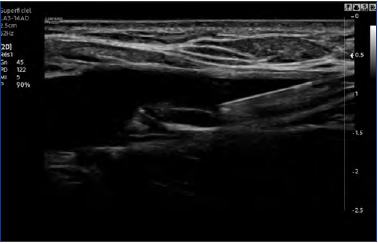
Figure 4. Ultrasound-guided endothermal procedure. The tip of the fiber (shown by arrow) is echogenic. Image provided courtesy of Anne-Sophie Lensel.
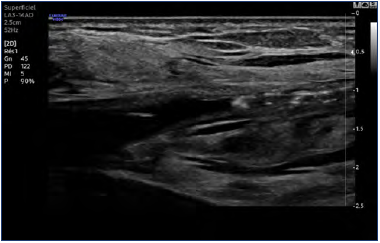
Figure 5. Ultrasound-guided endothermal procedure. Occlusion occurs where the fiber tip is positioned (see also Figure 4). Image provided courtesy of Anne-Sophie Lensel.
What kind of treatment can we perform on a competent (and small) vein?
Endovenous thermal ablation?
Whereas an introduction by Seldinger technique20 is easy to perform in an incompetent and large vein, it seems much more difficult to carry out in a thin, tiny one, especially when that vein is sinuous, with its intrafascial and straight portion not very long: the positioning of a tourniquet at the groin can be difficult, as would be the puncture.
A direct puncture with a 16-gauge Venflon cannula could then be proposed; the success of such step is to be studied. Some companies propose 400-μm laser fibers that can enter by a smaller Venflon cannula. The puncture of a small and competent vein in the superior third of the thigh can still be a practical issue.
For veins smaller than 4 mm, “thermal ablation by a seasoned operator, using suitable equipment, is tricky but technically feasible.”21
Despite that misgiving, a case report22 reviewing treatment of primary varicosis via EVLA of the GSV, including 278 procedures in 213 patients between May and December 2019, showed a 92.8% technical success rate early on. Occlusion of the GSV was achieved in 99.6%, and of the highest ascending SFJ tributary, if present, in 92.4%. The authors concluded that “a co-treatment of the tributaries is feasible and could improve the technical success of EVLA if a prophylactic closure of these veins is desired, especially if their distance to the SFJ is short.” Its effect on the recurrence rate needs further research.
A current German study is underway aiming to evaluate prevention of varicose vein recurrence via synchronous EVLA treatment of sufficient AASV in patients undergoing EVLA of an insufficient GSV.12
Cyanoacrylate closure?
Cyanoacrylate glue ablation is a nontumescent, nonthermal ablation technique for treatment of varicose veins and is safe and effective,23 at least in the short term; long-term studies are lacking as it was first used in 2013.24
Side effects have been described; for example, in 2020, Langridge and colleagues reported that rarely, cyanoacrylate glue embolization leads to extravasation and a chronic foreign body reaction requiring surgery. They concluded that “the relative novelty of cyanoacrylate glue embolization in the treatment of varicose veins requires clinicians to monitor for rare complications during its use in clinical practice. Patients should be aware of the rare risk of glue extravasation and foreign body reaction for fully informed consent prior to treatment.”25
Furthermore, endovenous glue-induced thrombosis (EGIT) is not that rare, and a diameter of <5 mm for saphenous veins is a risk factor for its development.26
Studies with that technique were also based on incompetent veins that are mostly big (diameter of 7 mm [range 5.6– 8 mm]).23 The feasibility on thinner veins is also to be determined.
Sclerotherapy?
The direct puncture of the vein, which is the most common technique in Europe, is feasible, with no difficulty, whatever the size of the vein. A phlebologist usually performs injections with ultrasound guidance in veins smaller than 2 or 3 mm, using 22- or 23-gauge needles. This can be done just after EVTA of the GSV for varicose veins in the tributaries (that are incompetent). The technical feasibility is good, being careful about vein-spasm risk.
Side effects of liquid or foam sclerotherapy are acceptable for the treatment of varicose veins, but they should raise questions if for the treatment of a competent vein.
Conclusion
In a 2019 review article entitled the “Fate of the tributaries of saphenofemoral junction following EVTA of incompetent axial vein,” Anwar and colleagues17 noted that a systematic review and meta-analysis by O’Donnell et al27 found that causes of recurrence are different after EVTA (mostly recanalization [32%] and development of incompetent AASV [19%]) than after surgical ligation (18% of neovascularization).
The European Society for Vascular Surgery reminds us in 2022 that “recurrent [varicose veins] often display recanalization of a saphenous trunk, previously treated by endovenous ablation, neovascularization at the location of previous surgery (in particular at the SFJ), or reflux in other veins such as the AASV, the SSV, or [perforating vein], which may have been healthy previously. The aim of investigation is to identify the nature and source of the recurrence.”28,29
Anwar and colleagues in their review17 found 3 main causes for AASV reflux (or any para-axial reflux) after EVTA of an incompetent GSV. These are as follows: i) true development of para-neoreflux (developing from incompetent SFJ into the AASV); ii) an AASV reflux missed in the initial scan; and iii) occult AASV reflux caused by “steal” effect of gross reflux in the untreated GSV in the initial scan. They note that “the true incidence of neoreflux into para-axial veins causing clinical significant recurrence is not known.” With this knowledge, should it be mandatory to do preventive treatment of competent AASV of the thigh (when it is present and drains directly into the SFJ)?
The feasibility and benefits do not seem to justify the risks, even if they are often reversible. The cost is also an important issue, especially for cyanoacrylate closure (in France for example, a dose costs €1000 with no possibility of reimbursement through insurance).
It is not always easy for the patient to accept side effects like deep venous thrombosis or skin pigmentation, even after well informed consent. It would be much more difficult to explain that those troubles are caused by treatment of a competent vein, solely as a preventive measure against risk of recurrence, which is in a range between 8% and 35%.
The aim in prevention of recurrent varicose veins today seems mainly to improve success of EVTA. “Neoreflux into tributaries of GSV including AASV is the most common (8–31%) pattern of recurrence following endovenous ablation of GSV. Successful GSV ablation depends on many factors including the mode and amount of thermal energy delivered, laser wavelength and pullback rate, use of perivenous tumescent infiltration, manual compression over the vein during the procedure and a fiber tip position below the SFJ.”17,30 However, the main factors determining successful abolition of reflux from GSV tributaries depend on how far the successful GSV ablation extends toward the SFJ and the distance of tributaries from the SFJ. It is reasonable to assume that any technique that ablates incompetent GSV far from the SFJ is unlikely to control the reflux into its tributaries. This may explain such variation in recurrence results (8%–31%).17
Therefore, today, I would not (yet) propose that my patients undergo concomitant treatment of a competent AASV during the procedure of thermoablation of the GSV, whether by sclerotherapy, cyanoacrylate closure, or thermoablation.
However, when more results from the German study12 become available in 5 years, they may change our practice relative to contemporary thought. We’ll need to wait and see!
REFERENCES
1. Garner J, Heppell P, Leopold P. The lateral accessory saphenous vein – a common cause of recurrent varicose veins. Ann R Coll Surg Engl. 2003;85:389-392.
2. Proebstle TM, Möhler T. A longitudinal single-center cohort study on the prevalence and risk of accessory saphenous vein reflux after radiofrequency segmental thermal ablation of great saphenous veins. J Vasc Surg Venous Lymphat Disord. 2015;3:265-269.
3. Winokur RS, Khilnani NM, Min RJ. Recurrence patterns after endovenous laser treatment of saphenous vein reflux. Phlebology. 2016;31:496-500.
4. Anwar MA, Idrees M, Aswini M, Theivacumar NS. Fate of the tributaries of saphenofemoral junction following endovenous thermal ablation of incompetent axial vein – a review article. Phlebology. 2019;34:151-155.
5. De Maeseneer M. What a phlebologist should know about the anterior accessory saphenous vein? Phlebolymphology. 2019;26(2):66-72.
6. Baccellieri D, Ardita V, Carta N, Melissano G, Chiesa R. Anterior accessory saphenous vein confluence anatomy at the sapheno-femoral junction as risk factor for varicose veins recurrence after great saphenous vein radiofrequency thermal ablation. Int Angiol. 2020;39(2):105-111. doi:10.23736/S0392-9590.20.04271-6.
7. Garcia-Gimeno M, Rodriguez-Camarero S, Tagarro-Villalba S, et al. Duplex mapping of 2036 primary varicose veins. J Vasc Surg. 2009;49:681-689.
8. Whiteley MS, Chen X, Chase LE, Holdstock JM, Harrison CC, Price BA. Treatment of the great saphenous vein by catheter based thermoablation is associated with anterior accessory saphenous vein treatment in almost a third of cases. Br J Surg. 2008;95(S3):191-192.
9. Alozai T, Huizing E, Schreve MA, et al. A systematic review and meta-analysis of treatment modalities for anterior accessory saphenous vein insufficiency. Phlebology. 2022;37(3):165-179. doi:10.1177/02683555211060998.
10. Schul MW, Schloerke B, Gomes GM. The refluxing anterior accessory saphenous vein demonstrates similar clinical severity when compared to the refluxing great saphenous vein. Phlebology. 2016;31(9):654-659. doi:10.1177/0268355515604532.
11. Muller L, Alm J. Feasibility and potential significance of prophylactic ablation of the major ascending tributaries in endovenous laser ablation (EVLA) of the great saphenous vein: a case series. PLoS One. 2021;16(1):e0245275. doi:10.1371/ journal.pone.0245275.
12. Fink C, Hartmann K, Mattausch T, et al. Impact of a synchronous prophylactic treatment of the anterior accessory saphenous vein on the recurrent varicose vein rate in patients undergoing thermal ablation of an insufficient great saphenous vein (SYNCHRONOUS-Study): study protocol for a prospective, multicentre, controlled observational study. BMJ Open. 2022;12(6):e061530. doi:10.1136/ bmjopen-2022-061530.
13. Caggiati A, Bergan JJ, Gloviczki P, Eklof B, Allegra C, Partsch H; International Interdisciplinary Consensus Committee on Venous Anatomical Terminology. Nomenclature of the veins of the lower limb: extensions, refinements, and clinical application. J Vasc Surg. 2005;41(4):719- 724.
14. Saphenes accessoires. Phlebologia. https://www.phlebologia.com/fr/lajonction- sapheno-femorale/saphenesaccessoires/
15. Muhlberger D, Morandini L, Brenner E. Venous valves and major superficial tributary veins near the saphenofemoral junction. J Vasc Surg. 2009;49(6):1562- 1569. doi:10.1016/j.jvs.2009.02.241.
16. Gerard JL. The duplex ultrasonography investigation of varicose veins, the therapeutic strategy. Phlebologie. 2020;73(2):59-85. [English version of chapter in: Guex JJ, Hamel-Desnos C, eds. Ultrasons et Phlébologie. Editions phlebologiques Francaises-Paris; 2016:123-132.]
17. Anwar MA, Idrees M, Aswini M, Theivacumar NS. Fate of the tributaries of sapheno femoral junction following endovenous thermal ablation of incompetent axial vein – a review article. Phlebology. 2019;34(3):151-155. doi:10.1177/0268355518783635.
18. Cappelli M, Molino Lova R, Ermini S, Giangrandi I, Giannelli F, Zamboni P. Hemodynamics of the sapheno-femoral complex: an operational diagnosis of proximal femoral valve function. Int Angiol. 2006;25(4):356-360.
19. Uhl JF, Lo Vuolo M, Labropoulos N. Anatomy of the lymph node venous networks of the groin and their investigation by ultrasonography. Phlebology. 2016;31:334-343.
20. Science Direct. Seldinger technique. Accessed July 2022. https://www. sciencedirect.com/topics/medicine-anddentistry/ seldinger-technique
21. Hamel-Desnos C, Miserey G. Mise au point/Focus “Choosing wisely.” Varices saphenes et recidives. Traitements d’occlusion chimique ou thermique dans l’insuffisance des veines saphenes et des recidives. Phlébologie. 2018:71(3):10-17.
22. Muller L, Alm J. Feasibility and potential significance of prophylactic ablation of the major ascending tributaries in endovenous laser ablation (EVLA) of the great saphenous vein: a case series. PLoS One. 2021;16(1):e0245275. doi:10.1371/ journal.pone.0245275.
23. Dimech AP, Cassar K. Efficacy of cyanoacrylate glue ablation of primary truncal varicose veins compared to existing endovenous techniques: a systematic review of the literature. Surg J (N Y). 2020;6(2):e77-e86. doi:10.1055/s-0040-1708866.
24. National Institute for Health and Care Excellence. Cyanoacrylate glue occlusion for varicose veins (Interventional procedures guidance 526) [Internet]. Published June 26, 2015. Accessed November 25, 2018. https://www.nice.org. uk/guidance/ipg526.
25. Langridge BJ, Onida S, Weir J, Moore H, Lane TR, Davies AH. Cyanoacrylate glue embolisation for varicose veins – a novel complication. Phlebology. 2020;35(7):520- 523. doi:10.1177/0268355520901662.
26. Cho S, Gibson K, Lee SH, Kim SY, Joh JH. Incidence, classification, and risk factors of endovenous glue-induced thrombosis after cyanoacrylate closure of the incompetent saphenous vein. J Vasc Surg Venous Lymphat Disord. 2020;8(6):991-998. doi:10.1016/j.jvsv.2020.01.009.
27. O’Donnell TF, Balk EM, Dermody M, Tangney E, Iafrati MD. Recurrence of varicose veins after endovenous ablation of the great saphenous vein in randomized trials. J Vasc Surg Venous Lymphat Disord. 2016;4(1):97-105. doi:10.1016/j.jvsv.2014.11.004.
28. De Maeseneer MG, Kakkos SK, Aherne T, et al. European Society for Vascular Surgery (ESVS) 2022 Clinical practice guidelines on the management of chronic venous disease of the lower limbs. Eur J Vasc Endovasc Surg. 2022;63(2):184-267. https://doi.org/10.1016/j.ejvs.2021.12.024.
29. De Maeseneer M, Pichot O, Cavezzi A, et al. Duplex ultrasound investigation of the veins of the lower limbs after treatment for varicose veins—UIP consensus document. Eur J Vasc Endovasc Surg. 2011;42:89- 102.
30. Disselhoff BC, der Kinderen DJ, Kelder JC, Moll FL. Five-year results of a randomised clinical trial of endovenous laser ablation of the great saphenous vein with and without ligation of the saphenofemoral junction. Eur J Vasc Endovasc Surg. 2011;41(5):685-690. doi:10.1016/j. ejvs.2010.12.014.
