Management of small saphenous vein varices with perspectives from a recent meta-analysis and recommendations
31076 Toulouse, France
Abstract
The methods of treating varicose veins have been constantly evolving over the past 20 years, leaving a prominent place today for endovenous techniques, with conventional surgery being gradually abandoned. The modern treatment of varicose veins of the lower-limbs is performed either by tumescent endovenous thermal techniques (laser, radiofrequency, steam) or by nonthermal nontumescent techniques (ultrasound-guided foam sclerotherapy, glue cyanoacrylate, mechanochemical endovenous ablation). The introduction of minimally invasive endovenous ablation techniques (thermal and nonthermal techniques) are associated with several advantages, including minimally invasive, immediate discharge and ambulation, faster recovery, and less periprocedural morbidity. Based on the literature and recommendations, endovenous thermal ablation should be preferred to surgery and foam sclerotherapy in the treatment of small saphenous vein incompetence. The potential benefits, particularly the reduced risk of nerve damage, might be of considerable clinical importance and may lead to a preference for nonthermal techniques in the future. Extensive data about nonthermal techniques are necessary to improve outcomes and achieve robust evidence.
Introduction
Isolated saphenopopliteal reflux may occur in up to 15% of patients with primary varicose veins.1 This reflux can be associated with equally significant chronic venous disease (CVD) signs and symptoms compared with great saphenous vein incompetence. Untreated varicose veins may sometimes lead to leg ulcerations, which are difficult to manage. Traditionally, treatment was restricted to surgery or compression therapy. Small saphenous vein surgery is considered more challenging than great saphenous vein surgery and is associated with higher recurrence and postoperative complication rates. Treating the small saphenous vein must be carried out very carefully because the ending is variable, and it is in close proximity to the nerves.
Over the past two decades, the treatment of varicose veins has been revolutionized by the introduction of minimally invasive endovenous ablation techniques (thermal and nonthermal techniques). These procedures are associated with several advantages, including a minimally invasive nature, immediate discharge and ambulation, faster recovery, and less periprocedural morbidity. They seem to have superior anatomical success rates compared with traditional surgical stripping.2-5
Surgical anatomy
Many complications of surgical stripping of the small saphenous vein have been described, such as damage to the sural nerve, the tibial nerve, and the fibular nerve. The small saphenous vein drains blood from the external part of the foot and the posterior internal part of the leg. It is a continuation of the external marginal vein that runs along the dorsal side of the foot. At its origin, the main trunk passes below, then behind the external malleolus in the external retromalleolar groove. It then rises vertically and in a median supra-aponeurotic position along the rear of the calf, and is then attached to the sural (sensory) nerve, which must not be damaged during thermal ablation. The sural nerve is an axial nerve formed by sensory branches of the tibial and fibular nerves. The sural accessory nerve emerges from the fibular nerve. At the apex of the calf, the sural nerve and its accessory branch join in a common trunk and accompanies the small saphenous vein down to the ankle.
At the mid-leg point, the small saphenous vein enters the subaponeurotic tunnel of the sural triceps. It then bends slightly, which tends to send it deeper, and the vein continues along its path to the top of the knee joint line. At the knee joint, it bends and forms an anterior concave arch to join the popliteal vein at a level that can vary, or it may even be attached to a subordinate popliteal trunk in the great saphenous vein or the tributaries thereof, in the deep femoral vein, or it may even form a joint trunk with the gastrocnemius veins.
The sciatic nerve, which is located posterior to the thigh, is divided at variable levels, but mostly at the summit of the popliteal fossa. This division is slightly displaced from the longitudinal axis of the limb on the lateral aspect. It is divided into 2 nerves: the tibial nerve and the fibular nerve; it is advisable to stay below this area (by about 15 mm to 20 mm in general) to avoid damaging the nerve during endovenous thermal ablations.
In 15% to 20% of cases, the saphenopopliteal junction is nonexistent. The external saphenous trunk extends to the rear side of the thigh. It then bends inward to join the internal saphenous trunk, or it may run down toward the deep femoral vein.3,6,7
Thermal techniques (laser and radiofrequency ablation) have emerged as an effective alternative to open surgery with stripping and high ligation. These methods are nevertheless accompanied by risks and side effects. Compared with open surgical therapy, the risk of damage to peripheral and motor nerves is reduced; however, it still exists as a result of heat exposure and tumescent anesthesia. Nonthermal methods that can be applied without tumescent anesthesia have been introduced as they pose a considerably lower risk of nerve lesions while proving to be effective.8
Recommendations for treating the small saphenous vein
International recommendations for endovenous saphenous ablation are heterogeneous, particularly for small saphenous vein treatment (Table I).9-15 Concerning surgery, the 2011 American Venous Forum guidelines did not mention thermal treatments, but rather surgery, with level 1B evidence. For thermal treatments, the 2011 American Venous Forum guidelines recommend high ligation with invagination stripping with a grade of 1B, the 2012 International Union of Phlebology recommends thermal treatment with a grade of 1A, the 2013 NICE guidelines considered all of the saphenous axes together, without making a specific analysis of the small vs the great saphenous vein, the 2015 ESVS guidelines gave thermal treatments a grade 2B recommendation, and the 2016 AVLS and the 2016 LATAM guidelines gave grade 1B recommendations. In a recent publication, the European College of Phlebology guidelines for truncal ablation reports that, for the treatment of short saphenous reflux, endovenous laser ablation or radiofrequency ablation techniques are recommended in preference to surgery or foam sclerotherapy, assigning a 2A level of evidence.16 The 2014 Europe and LATAM 2016 guidelines gave sclerotherapy a grade 1A. The other guidelines indicated sclerotherapy treatment, but without a grade of evidence. The guidelines on nonthermal nontumescent techniques consider all of the saphenous axes together, without making a specific analysis of the small vs the great saphenous vein. Since 2016, the AVLS has recommended mechanochemical endovenous ablation with a grade 2B and the NICE accepted the procedure as standard.
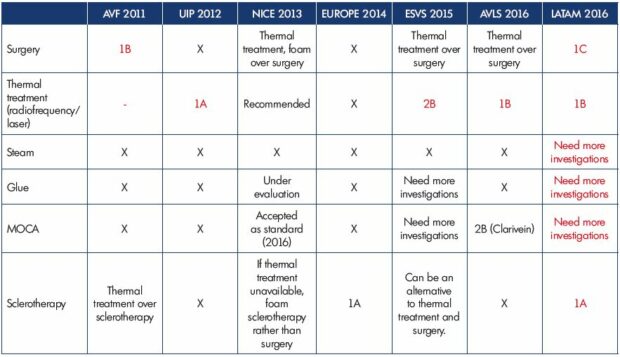
Table I. Guideline recommendations.
The text in red indicated the guidelines are considering just the small saphenous vein. The rest are considering all of
the saphenous axis together, without making a specific analysis of the small vs the great saphenous vein. X, no specific
recommendation.
Literature
Before the past two decades, conventional saphenopopliteal junction ligation with or without stripping of the small saphenous vein has been the standard treatment for varicose veins associated with saphenopopliteal reflux. Small saphenous vein surgery is considered more challenging than great saphenous vein surgery and is associated with higher recurrence and postoperative complication rates. With a conventional surgical procedure, an incision is made in the popliteal fossa, and the small saphenous vein and saphenopopliteal junction are identified. The saphenopopliteal junction is then disconnected and a short segment of the small saphenous vein is either resected or stripped. Treating the small saphenous vein must be carried out very carefully because the ending is variable, and it is in close proximity to the nerves. Generally, a class II stocking is worn for a month.
In their meta-analysis, Boersma et al2 reported the results of nine articles (surgical treatment of 798 small saphenous veins).17-25 The surgical procedures were heterogeneous, included ligation and/or disconnection of the saphenopopliteal junction, with or without stripping, and there were anatomical success rates of 24% to 94% over a mean follow-up of 17.3 months. Two studies that randomized patients to either surgery or endovenous laser ablation showed inferior anatomical success rates for surgery.17,19 Brittenden et al18 reported data from a study that randomized patients to surgery, endovenous laser ablation, or foam, showing inferior anatomical success rates compared with endovenous laser ablation, but comparable results with foam. Allegra reported long-term anatomical success in 70% of 132 small saphenous veins after 5 years of follow-up.22 Paresthesia occurred in up to 31% (mean 19.6%) and deep venous thrombosis in 0.7%. In their study, van Groenendael et al26 compared the treatment of recurrences of 42 small saphenous veins (laser vs surgery) and showed that the incidence of recurrences was not statically significant between the groups. There was a faster recovery following laser ablation (1 day vs 7 days), and endovenous laser ablation reduced the incidence of sural nerve injury (9% vs 20%).
In the treatment of small saphenous veins, thermal ablation or surgery are well-established methods. Nevertheless, treatment of saphenous veins by ultrasound-guided foam sclerotherapy could also be an effective and cost-effective treatment option. Sclerotherapy is the targeted chemical ablation of varicose veins by an intravenous injection of a foamed sclerosing drug. The irritant nature of the sclerosant causes inflammation of the endothelium and sub-endothelium layers of the vein wall, resulting in fibrosis and occlusion of the vein. Traditional foam has been prepared by mixing liquid sclerosant with room air or gas, using the Tessari method or the double syringe method.27
Postsclerotherapy compression is not clearly defined, but Hamel Desnos et al28 found, in a randomized controlled trial, no differences between the compression group and the control group when comparing efficacy, side effects, satisfaction scores, symptoms, and QOL.
In their meta-analysis, Boersma et al2 reported the results from 6 articles, including 1 randomized controlled trial (foam sclerotherapy treatment of 494 small saphenous veins).18,29-33 The Tessari method was mostly used to produce foam (liquid-to-air ratio of 1:4 or 1:3); studies were heterogeneous and used polidocanol (1% or 3%) and sodium tetradecyl sulfate (1% or 3%), with a mean anatomical success rate that ranged from 20% to 96%. Only 2 studies described postprocedural complications and deep venous thrombosis was noted in just 1 patient. In a prospective and controlled study, Gillet et al34 demonstrated a low rate of deep venous thrombosis after foam sclerotherapy of 331 small saphenous veins. Only two (0.6%) deep venous thromboses were observed, both of which were confined to the medial gastrocnemius veins and were reported in symptomatic patients.
Endothermal modalities (ie, endovenous laser ablation and radiofrequency ablation) use heat transfer to ablate incompetent venous trunks, with local infiltration of tumescent anesthesia used to protect surrounding structures from heating injury, to induce venous compression, and to limit procedural pain. The small saphenous vein is punctured at mid-calf to reduce the risk of sural nerve injury. When treating the small saphenous vein, the tip is positioned at the point where the small saphenous vein leaves the subfascial space to join the popliteal vein.16 Despite this, thermal injury may increase the rates of periprocedural pain, skin burns, and nerve injury. Postintervention compression for 1 week is often recommended, but the value and duration of compression is not clearly defined.35 However, a recent meta-analysis did not reveal any advantage of compression therapy.36
Endovenous laser ablation
In endovenous laser ablation, under ultrasound guidance, a bare-tipped or jacketed laser optical fiber is inserted into the vein from a distal point toward the junction, followed by laser activation. The fiber is then slowly withdrawn, and the vein becomes occluded. Boersma et al2 reported the results of 28 articles, including 4 randomized controlled trials (laser treatment of 2950 small saphenous veins).17-19,37-61 Studies were heterogeneous regarding energy delivery, wavelengths used (810 nm, 940 nm 980 nm, and 1470 nm), and use of pulsed and continuous modes. In almost all studies, patients underwent additional therapies (phlebectomy, sclerotherapy, and stripping). Anatomical success rates were 81% to 100% and the mean follow-up was 12.5 months (range 0.5 to 48). Deep venous thrombosis was seen in 0.8% of all patients, and postprocedural paresthesia was described in 4.8%. In a randomized controlled trial, Doganci et al37 showed that the puncture site affects the rate of nerve injury: the rate of paresthesia is significantly lower when the small saphenous vein is cannulated in the mild-calf. Hirokawa et al62 reported that the rates of pain (0% vs 25.0%) and bruising (7.0% vs 57.1%) were significantly lower in the group that used the 1470-nm laser and the radial 2-ring fiber.
Radiofrequency ablation
In radiofrequency ablation, under ultrasound guidance, a catheter electrode is inserted into the vein and the tip placed close to the junction. When activated, heat generated from the electrode results in closure of the vein. Boersma et al2 reported the results of nine articles (radiofrequency ablation treatment of 386 small saphenous veins)63-71 Studies were heterogeneous and used ClosurePlus, ClosureFast, and Celon. The anatomical success after a mean follow-up of 14.3 months ranged from 82% to 100%. Complications were poorly reported, and 5 studies described a mean deep venous thrombosis rate of 1.2% (range, 0% to 8%) and paresthesia was seen in 9.7% (mean). Park et al65 described paresthesia in 26% of patients, but radiofrequency ablation in some patients in this cohort was performed by proximal ligation and retrograde ablation. Wo´z niak et al72 published a comparative analysis of 5-year outcomes of lower extremity varicose vein therapy (13 small saphenous veins) using monopolar and segmental radiofrequency ablation and reported a 100% occlusion rate and no paresthesia.
Nonthermal techniques, including mechanochemical ablation and cyanoacrylate vein ablation, have been developed with a view to remove the risk of thermal injury. The various techniques of nonthermal ablation can completely avoid the need for tumescent anesthesia, reduce the time of the intervention, per-interventional pain, bruises, and sensory nerve lesions.
Mechanochemical endovenous ablation
Mechanochemical endovenous ablation is a hybrid endovascular procedure that has two components: mechanical abrasion via a special catheter and chemical ablation by injecting foam sclerosant (sodium tetradecyl sulfate or polidocanol). The ClariVein catheter is positioned through a micros heath with the tip of the device 2 cm distal to the saphenopopliteal junction under ultrasound guidance. The mechanical damage to the endothelium is caused by the catheter’s rotating element and the chemical damage by the sclerosants.
Witte et al,73 in a meta-analysis, reported the results of six articles (mechanochemical endovenous ablation of 254 small saphenous veins).74-79 Two publications (randomized controlled trials) included the same patient population.76,77 The primary outcome was anatomical success, defined as closure and absence of reflux on duplex ultrasound imaging. The anatomical success rate was 87% (mean) after a follow-up that ranged from 8 to 52 weeks. Studies were heterogeneous and used liquid polidocanol (1.5% or 2%) or liquid sodium tetradecyl sulfate (1.5% or 2%). There was one patient with an injury of the sural nerve after treatment resulting in transient hyperesthesia. This patient already suffered from sensory, sural neuropathy after previous saphenopopliteal junction ligation, which was aggravated by the mechanochemical endovenous ablation. Paresthesia has not been reported specifically for the small saphenous vein.
Glue cyanoacrylate ablation
n-Butyl cyanoacrylate is delivered intravascularly, and it polymerizes when it comes in contact with blood, leading to occlusion of the vessel. In animal models, the cyanoacrylate-treated veins have a granulomatous-type inflammatory response with the presence of giant cells, segmental wall thickening, and fibrosis.80 The procedure involves using an introducer sheath, a dispensing catheter, and a syringe that is attached to a dispenser gun. The catheter is advanced into the varicose vein under ultrasound guidance. The catheter is placed in specific areas along the varicose vein and the clinician conducts a series of trigger pulls to deliver the medical adhesive. Compression is applied to the leg during the procedure. When treating the small saphenous vein, the catheter tip is positioned 3 cm to 5 cm distal to the saphenopopliteal junction.81 Compression after cyanoacrylate ablation is not mandatory. Extensive data about small saphenous vein treatment are necessary to improve outcomes and achieve robust evidence.
Eroglu et al,82 in a randomized controlled trial comparing cyanoacrylate, radiofrequency ablation, and endovenous laser ablation for the treatment of superficial venous incompetence, included 28 small saphenous veins (9 with cyanoacrylate, 3 with radiofrequency ablation, and 16 with endovenous laser ablation) and, at 2 years in any patient undergoing procedures, there were no reported recanalizations, deep venous thromboses, or paresthesia. In the WAVES trial, Gibson et al83 showed, in 8 small saphenous veins, an anatomical success rate of 100% after a follow-up of 12 months. In their study, Yasim et al84 treated 11 small saphenous veins and observed, after a mean follow-up of 5.5 months, no recanalizations and no adverse effects.
Safety data
Thromboprophylaxis can be prescribed for high-risk patients (previous venous thromboembolism, documented thrombophilia, obesity, immobilized patients, patients with neoplasm, and older patients). It is recommended to perform duplex ultrasound screening after thermal and nonthermal ablation within 10 days postoperatively, but this is not clearly defined.
Conclusion
In their meta-analysis, Boersma et al2 reported that ablation techniques (endovenous laser ablation and radiofrequency ablation) were found to present higher pooled anatomic success rates (98.5% and 97.1%, respectively) as compared with surgery (58%) and ultrasound-guided foam sclerotherapy (63.6%). Neurologic complications were also more frequent after surgery than thermal ablation (19.6% vs 4.8% after endovenous laser ablation and 9.7% after radiofrequency ablation). Based on the literature and recommendations, endovenous thermal ablation should be preferred to surgery and foam sclerotherapy in the treatment of small saphenous vein incompetence. The potential benefits, particularly the reduced risk of nerve damage, might be of considerable clinical importance and may lead to a preference for nonthermal techniques in the future. Extensive data about nonthermal techniques are necessary to improve outcomes and acquire robust evidence. The cost analysis of varicose vein treatments should also be taken into account in future treatment recommendations.
REFERENCES
1. Tellings SS, Ceulen RPM, Sommer A. Surgery and endovenous techniques for the treatment of small saphenous varicose veins: a review of the literature. Phlebology. 2011;26(5):179‑84.
2. Boersma D, Kornmann VNN, van Eekeren RRJP, et al. Treatment modalities for small saphenous vein insufficiency: systematic review and meta-analysis. J Endovasc Ther. 2016;23(1):199‑211.
3. Gérard J-L. Small saphenous vein interventional treatment. Phlebolymphology. 2017;24(3):119-129.
4. Witte ME, Zeebregts CJ, de Borst GJ, Reijnen MMPJ, Boersma D. Mechanochemical endovenous ablation of saphenous veins using the ClariVein: a systematic review. Phlebology. 2017;32(10):649‑657.
5. Paravastu SC, Horne M, Dodd PD. Endovenous ablation therapy (laser or radiofrequency) or foam sclerotherapy versus conventional surgical repair for short saphenous varicose veins. Cochrane Database Syst Rev. 2016;11(11):CD010878.
6. Kerver ALA, van der Ham AC, Theeuwes HP, et al. The surgical anatomy of the small saphenous vein and adjacent nerves in relation to endovenous thermal ablation. J Vasc Surg. 2012;56(1):181‑188.
7. Uhl J-F, Gillot C. Anatomy and embryology of the small saphenous vein: nerve relationships and implications for treatment. Phlebology. 2013;28(1):4‑15.
8. Hirsch T. Varicose vein therapy and nerve lesions. Vasa. 2017;46(2):96‑100.
9. Pavlović MD, Schuller-Petrović S, Pichot O, et al. Guidelines of the first international consensus conference on endovenous thermal ablation for varicose vein disease–ETAV Consensus Meeting 2012. Phlebology. 2015;30(4):257-273.
10. National Clinical Guideline Centre (UK). Varicose Veins in the Legs: The Diagnosis and Management of Varicose Veins. London, UK: National Institute for Health and Care Excellence (UK); 2013.
11. Rabe E, Breu F, Cavezzi A, et al. European guidelines for sclerotherapy in chronic venous disorders. Phlebology. 2014;29(6):338‑354.
12. Wittens C, Davies AH, Bækgaard N, et al. Management of chronic venous disease: clinical practice guidelines of the European Society for Vascular Surgery (ESVS). Eur J Vasc Endovasc Surg. 2015;49(6):678‑737.
13. American Vein & Lymphatic Society. Guidelines & standards: treatment of superficial venous disease of the lower leg guidelines. https://www.myavls.org/ member-resources/clinical-guidelines. html. Accessed February 10, 2020.
14. Conmision Nacional de Bibliotecas Populares. Guías latinoamericanas de terapeútica para la patología venosa. http://www.conabip.gob.ar/ node/278122. Accessed February 10, 2020.
15. Gianesini S, Obi A, Onida S, et al. Global guidelines trends and controversies in lower-limb venous and lymphatic disease. Phlebology. 2019;34(suppl 1):4‑66.
16. Kürşat Bozkurt A, Lawaetz M, Danielsson G, et al. European College of Phlebology guideline for truncal ablation. Phlebology. 200;35(2):73‑83.
17. Nandhra S, El-sheikha J, Carradice D, et al. A randomized clinical trial of endovenous laser ablation versus conventional surgery for small saphenous varicose veins. J Vasc Surg. 2015;61(3):741‑746.
18. Brittenden J, Cotton SC, Elders A, et al. Clinical effectiveness and costeffectiveness of foam sclerotherapy, endovenous laser ablation and surgery for varicose veins: results from the Comparison of LAser, Surgery and foam Sclerotherapy (CLASS) randomised controlled trial. Health Technol Assess. 2015;19(27):1‑342.
19. Roopram AD, Lind MY, Van Brussel JP, et al. Endovenous laser ablation versus conventional surgery in the treatment of small saphenous vein incompetence. J Vasc Surg Venous Lymphat Disord. 2013;1(4):357‑363.
20. Ikponmwosa A, Bhasin N, Weston MJ, Berridge DC, Scott DJA. Outcome following saphenopopliteal surgery: a prospective observational study. Phlebology. 2010;25(4):174‑178.
21. O’Hare JL, Vandenbroeck CP, Whitman B, Campbell B, Heather BP, Earnshaw JJ. A prospective evaluation of the outcome after small saphenous varicose vein surgery with one-year follow-up. J Vasc Surg. 2008;48(3):669‑673.
22. Allegra C, Antignani PL, Carlizza A. Recurrent varicose veins following surgical treatment: our experience with five years follow-up. Eur J Vasc Endovasc Surg. 2007;33(6):751‑756.
23. Dumas BE, Spronk S, Boelhouwer RU, den Hoed PT. Subfascial ligation at three different levels versus partial exeresis of the incompetent short saphenous vein: a randomized clinical trial. J Vasc Nurs. 2007;25(1):12‑18.
24. Whiteley MS, Lewis G, Holdstock JM, et al. Minimally invasive technique for ligation and stripping of the small saphenous vein guided by intraoperative duplex ultrasound. Surgeon. 2006;4(6):372‑377.
25. Rashid HI, Ajeel A, Tyrrell MR. Persistent popliteal fossa reflux following saphenopopliteal disconnection: persistent popliteal fossa reflux following saphenopopliteal disconnection. Br J Surg. 2002;89(6):748‑751.
26. van Groenendael L, Flinkenflögel L, van der Vliet JA, Roovers EA, van Sterkenburg SMM, Reijnen MMPJ. Conventional surgery and endovenous laser ablation of recurrent varicose veins of the small saphenous vein: a retrospective clinical comparison and assessment of patient satisfaction. Phlebology. 2010;25(3):151‑157.
27. Tessari L, Cavezzi A, Frullini A. Preliminary experience with a new sclerosing foam in the treatment of varicose veins. Dermatol Surg. 2001;27(1):58‑60.
28. Hamel-Desnos CM, Guias BJ, Desnos PR, Mesgard A. Foam Sclerotherapy of the saphenous veins: randomised controlled trial with or without compression. Eur J Vasc Endovasc Surg. 2010;39(4):500‑507.
29. Asciutto G, Lindblad B. Catheterdirected foam sclerotherapy treatment of saphenous vein incompetence. Vasa. 2012;41(2):120‑124.
30. Darvall KAL, Bate GR, Silverman SH, Adam DJ, Bradbury AW. Mediumterm results of ultrasound-guided foam sclerotherapy for small saphenous varicose veins. Br J Surg. 2009;96(11):1268‑1273.
31. O’Hare JL, Parkin D, Vandenbroeck CP, Earnshaw JJ. Mid term results of ultrasound guided foam sclerotherapy for complicated and uncomplicated varicose veins. Eur J Vasc Endovasc Surg. 2008;36(1):109‑113.
32. Darke SG, Baker SJA. Ultrasoundguided foam sclerotherapy for the treatment of varicose veins. Br J Surg. 2006;93(8):969‑974.
33. Smith PC. Chronic venous disease treated by ultrasound guided foam sclerotherapy. Eur J Vasc Endovasc Surg. 2006;32(5):577‑583.
34. Gillet J, Lausecker M, Sica M, Guedes J, Allaert F. Is the treatment of the small saphenous veins with foam sclerotherapy at risk of deep vein thrombosis? Phlebology. 2014;29(9):600‑607.
35. Marsden G, Perry M, Kelley K, Davies AH. Diagnosis and management of varicose veins in the legs: summary of NICE guidance. BMJ. 2013;347:f4279.
36. Al Shakarchi J, Wall M, Newman J, et al. The role of compression after endovenous ablation of varicose veins. J Vasc Surg Venous Lymphat Disord. 2018;6(4):546‑550.
37. Doganci S, Yildirim V, Demirkilic U. Does puncture site affect the rate of nerve injuries following endovenous laser ablation of the small saphenous veins? Eur J Vasc Endovasc Surg. 2011;41(3):400‑405.
38. Aktas AR, Celik O, Ozkan U, et al. Comparing 1470- and 980- nm diode lasers for endovenous ablation treatments. Lasers Med Sci. 2015;30(5):1583‑1587.
39. Park JA, Park SW, Chang IS, et al. The 1.470-nm bare-fiber diode laser ablation of the great saphenous vein and small saphenous vein at 1-year follow-up using 8–12 W and a mean linear endovenous energy density of 72 J/cm. J Vasc Interv Radiol. 2014;25(11):1795‑1800.
40. Spreafico G, Piccioli A, Bernardi E, et al. Endovenous laser ablation of great and small saphenous vein incompetence with a 1470-nm laser and radial fiber. J Vasc Surg Venous Lymphat Disord. 2014;2(4):403‑410.
41. Moul DK, Housman L, Romine S, Greenway H. Endovenous laser ablation of the great and short saphenous veins with a 1320-nm neodymium:yttriumaluminum- garnet laser: retrospective case series of 1171 procedures. J Am Acad Dermatol. 2014;70(2):326‑331.
42. Lakhwani MN. Holistic management of venous ulcers especially with endovenous laser treatment using 980nm laser in an ethnically diverse society. Med J Malasia. 2013;68(6):453- 458.
43. von Hodenberg E, Zerweck C, Knittel M, Zeller T, Schwarz T. Endovenous laser ablation of varicose veins with the 1470 nm diode laser using a radial fiber – 1-year follow-up. Phlebology. 2015;30(2):86‑90.
44. Ozkan U, Sariturk C. Early clinical improvement in chronic venous insufficiency symptoms after laser ablation of saphenous veins. Diagn Interv Radiol. 2012;18(6):594-598.
45. Desmyttère J, Grard C, Stalnikiewicz G, Wassmer B, Mordon S. Endovenous laser ablation (980nm) of the small saphenous vein in a series of 147 limbs with a 3-year follow-up. Eur J Vasc Endovasc Surg. 2010;39(1):99‑103.
46. Janne d’Othée B, Walker TG, Kalva SP, Ganguli S, Davison B. Endovenous laser ablation of the small saphenous vein sparing the saphenopopliteal junction. Cardiovasc Intervent Radiol. 2010;33(4):766‑71.
47. Ravi R, Trayler EA, Barrett DA, Diethrich EB. Endovenous thermal ablation of superficial venous insufficiency of the lower extremity: single-center experience with 3000 limbs treated in a 7-year period. J Endovasc Ther. 2009;16(4):500‑505.
48. Huisman LC, Bruins RMG, van den Berg M, Hissink RJ. Endovenous laser ablation of the small saphenous vein: prospective analysis of 150 patients, a cohort study. Eur J Vasc Endovasc Surg. 2009;38(2):199‑202.
49. Kontothanassis D, Di Mitri R, Ferrari Ruffino S, et al. Endovenous laser treatment of the small saphenous vein. J Vasc Surg. 2009;49(4):973-979.e1.
50. Nwaejike N, Srodon PD, Kyriakides C. 5-years of endovenous laser ablation (EVLA) for the treatment of varicose veins – a prospective study. Int J Surg. 2009;7(4):347‑349.
51. Myers KA, Jolley D. Outcome of endovenous laser therapy for saphenous reflux and varicose veins: mediumterm results assessed by ultrasound surveillance. Eur J Vasc Endovasc Surg. 2009;37(2):239‑245.
52. Pannier F, Rabe E, Maurins U. First results with a new 1470-nm diode laser for endovenous ablation of incompetent saphenous veins. Phlebology. 2009;24(1):26‑30.
53. Hamel-Desnos C, Gérard J-L, Desnos P. Endovenous laser procedure in a clinic room: feasibility and side effects study of 1700 cases. Phlebology. 2009;24(3):125‑130.
54. Elmore FA, Lackey D. Effectiveness of endovenous laser treatment in eliminating superficial venous reflux. hlebology. 2008;23(1):21‑31.
55. Trip-Hoving M, Verheul JC, van Sterkenburg SMM, de Vries WR, Reijnen MMPJ. Endovenous laser therapy of the small saphenous vein: patient satisfaction and short-term results. Photomed Laser Surg. 2009;27(4):655‑658.
56. Jung IM, Min SI, Heo SC, Ahn YJ, Hwang K-T, Chung JK. Combined endovenous laser treatment and ambulatory phlebectomy for the treatment of saphenous vein incompetence. Phlebology. 2008;23(4):172‑177.
57. Park SJ, Yim SB, Cha DW, Kim SC, Lee SH. Endovenous laser treatment of the small saphenous vein with a 980-nm diode laser: early results. Dermatol Surg. 2008;34(4):517.
58. Gibson KD, Ferris BL, Polissar N, Neradilek B, Pepper D. Endovenous laser treatment of the short saphenous vein: efficacy and complications. J Vasc Surg. 2007;45(4):795‑803.
59. Theivacumar NS, Beale RJ, Mavor AID, Gough MJ. Initial experience in endovenous laser ablation (EVLA) of varicose veins due to small saphenous vein reflux. Eur J Vasc Endovasc Surg. 2007;33(5):614‑618.
60. Perkowski P, Ravi R, Gowda RCN, et al. Endovenous laser ablation of the saphenous vein for treatment of venous insufficiency and varicose veins: early results from a large singlecenter experience. J Endovasc Ther. 2004;11(2):132‑138.
61. Proebstle TM, Gül D, Kargl A, Knop J. Endovenous laser treatment of the lesser saphenous vein with a 940-nm diode laser: early results. Dermatol Surg. 2003;29(4):357‑361.
62. Hirokawa M, Ogawa T, Sugawara H, Shokoku S, Sato S. Comparison of 1470 nm laser and radial 2ring fiber with 980 nm laser and bare-tip fiber in endovenous laser ablation of saphenous varicose veins: a multicenter, prospective, randomized, non-blind study. Ann Vasc Dis. 2015;8(4):282‑289.
63. Schuller- Petrović S, Pavlović MD, Schuller- Lukić B, Schuller S. Retrospective analysis of routine use of a double heat cycle (DHC) during radiofrequency segmental ablation (ClosureFASTTM) of saphenous veins. J Eur Acad Dermatol Venereol. 2016;30(6):1009‑1012.
64. Doerler M, Blenkers T, Reich-Schupke S, Altmeyer P, Stücker M. Occlusion rate, venous symptoms and patient satisfaction after radiofrequencyinduced thermotherapy (RFITT_): are there differences between the great and the small saphenous veins? Vasa. 2015;44(3):203‑210.
65. Park JY, Galimzahn A, Park HS, Yoo YS, Lee T. Midterm results of radiofrequency ablation for incompetent small saphenous vein in terms of recanalization and sural neuritis. Dermatol Surg. 2014;40(4):383‑389.
66. Harlander-Locke M, Jimenez JC, Lawrence PF, et al. Management of endovenous heat-induced thrombus using a classification system and treatment algorithm following segmental thermal ablation of the small saphenous vein. J Vasc Surg. 2013;58(2):427‑432.
67. Choi JH, Park H-C, Joh JH. The occlusion rate and patterns of saphenous vein after radiofrequency ablation. J Korean Surg Soc. 2013;84(2):107‑113.
68. Gabriel V, Jimenez JC, Alktaifi A, et al. Success of endovenous saphenous and perforator ablation in patients with symptomatic venous insufficiency receiving long-term warfarin therapy. Ann Vasc Surg. 2012;26(5):607‑611.
69. Bisang U, Meier TO, Enzler M, Thalhammer C, Husmann M, Amann- Vesti BR. Results of endovenous ClosureFast treatment for varicose veins in an outpatient setting. Phlebology. 2012;27(3):118‑123.
70. Monahan TS, Belek K, Sarkar R. Results of radiofrequency ablation of the small saphenous vein in the supine position. Vasc Endovascular Surg. 2012;46(1):40‑44.
71. Boon R, Akkersdijk GJM, Nio D. Percutaneus treatment of varicose veins with bipolar radiofrequency ablation. Eur J Radiol. 2010;75(1):43‑47.
72. Woźniak W, Kielar M, Mlosek RK, Ciostek P. Comparative analysis of five-year outcomes of lower extremity varicose vein therapy using monopolar and segmental radiofrequency ablation. Int Angiol. 2018;37(6):457-464.
73. Witte ME, Zeebregts CJ, de Borst GJ, Reijnen MMPJ, Boersma D. Mechanochemical endovenous ablation of saphenous veins using the ClariVein: a systematic review. Phlebology. 2017;32(10):649‑657.
74. Boersma D, van Eekeren RRJP, Werson DAB, van der Waal RIF, Reijnen MMJP, de Vries J-PPM. Mechanochemical endovenous ablation of small saphenous vein insufficiency using the ClariVein_ device: one-year results of a prospective series. Eur J Vasc Endovasc Surg. 2013;45(3):299‑303.
75. Deijen CL, Schreve MA, Bosma J, et al. Clarivein mechanochemical ablation of the great and small saphenous vein: early treatment outcomes of two hospitals. Phlebology. 2016;31(3):192‑7.
76. Bootun R, Lane T, Dharmarajah B, et al. Intra-procedural pain score in a randomised controlled trial comparing mechanochemical ablation to radiofrequency ablation: The Multicentre VenefitTM versus ClariVein_ for varicose veins trial. Phlebology. 2016;31(1):61‑65.
77. Lane T, Bootun R, Dharmarajah B, et al. A multi-centre randomised controlled trial comparing radiofrequency and mechanical occlusion chemically assisted ablation of varicose veins – final results of the Venefit versus Clarivein for varicose veins trial. Phlebology. 2017;32(2):89‑98.
78. Tang T, Kam J, Gaunt M. ClariVein_ – early results from a large single-centre series of mechanochemical endovenous ablation for varicose veins. Phlebology. 2017;32(1):6‑12.
79. Vun S, Rashid S, Blest N, Spark J. Lower pain and faster treatment with mechanico-chemical endovenous ablation using ClariVein_. Phlebology. 2015;30(10):688‑692.
80. Almeida JI, Min RJ, Raabe R, McLean DJ, Madsen M. Cyanoacrylate adhesive for the closure of truncal veins: 60-day swine model results. Vasc Endovascular Surg. 2011;45(7):631‑635.
81. Anwar MA, Lane TR, Franklin IJ, et al. Cyanoacrylate for the treatment of small saphenous vein venous incompetence. Cureus. 2014;6(10): e221.
82. Eroglu E, Yasim A. A randomised Clinical trial comparing n-butyl cyanoacrylate, radiofrequency ablation and endovenous laser ablation for the treatment of superficial venous incompetence: two year follow up results. Eur J Vasc Endovasc Surg. 2018;56(4):553-560.
83. Gibson K, Minjarez R, Gunderson K, Ferris B. Need for adjunctive procedures following cyanoacrylate closure of incompetent great, small and accessory saphenous veins without the use of postprocedure compression: Three-month data from a postmarket evaluation of the VenaSeal System (the WAVES Study). Phlebology. 2019;34(4):231‑237.
84. Yasim A, Eroglu E, Bozoglan O, Mese B, Acipayam M, Kara H. A new nontumescent endovenous ablation method for varicose vein treatment: early results of N-butyl cyanoacrylate (VariClose_). Phlebology. 2017;32(3):194‑199.
