Review and Comment of the 2011 Clinical Practice Guidelines of the Society for Vascular Surgery and the American Venous Forum
ABSTRACT
The Clinical Practice Guidelines of The Society for Vascular Surgery and The American Venous Forum, published in the 2011 Journal of Vascular Surgery supplement, is the most complete document on the management of varicose veins ever published in English. It is the work of leading members of the American Venous Forum, who are major contributors to advances in this field. However, most of them are vascular surgeons and this may have influenced their recommendations.
A total of 14 guidelines are recommended or suggested using the recommendation grading system of Guyatt et al. The present article will specifically review these recommendations, bearing in mind that as Europeans we may have some divergence of opinion with our American colleagues.
INTRODUCTION
The Clinical Practice Guidelines of The Society for Vascular Surgery and The American Venous Forum, published in the 2011 Journal of Vascular Surgery supplement, is the most complete document on the management of varicose veins (VVs) ever published in English. It is the work of leading members of the American Venous Forum, whose knowledge in this field is undisputed. However, most of them are vascular surgeons and this may have influenced their recommendations.
The article is 47 pages long and includes:
– 2 figures depicting the superficial, deep, and perforator veins of the lower limbs.
– 8 tables, including:
The different levels of evidence-based recommendations as described by Guyatt et al1 (Table I).
• The CEAP classification2 (Table II).
• The venous anatomic segment classification2 (Table III).
• The Revised Venous Clinical Severity Score3 (Table IV).
• A definition of the major and minor complications of endovenous ablation4 (Table V).
• The main manufacturers of endovenous ablation devices and the laser wavelengths of these devices.
• A comparison of sclerosing agents.
• The indications for sclerosing agents and the concentrations used.
No fewer than 376 references are quoted, a veritable gold mine for readers and fellow writers, especially considering that very few major articles are missing.
In total, 14 guidelines are recommended or suggested using the recommendation grading system mentioned above.1
In this review, we will focus on these guidelines, bearing in mind that our European practice may account for some divergence of opinion with our American colleagues.
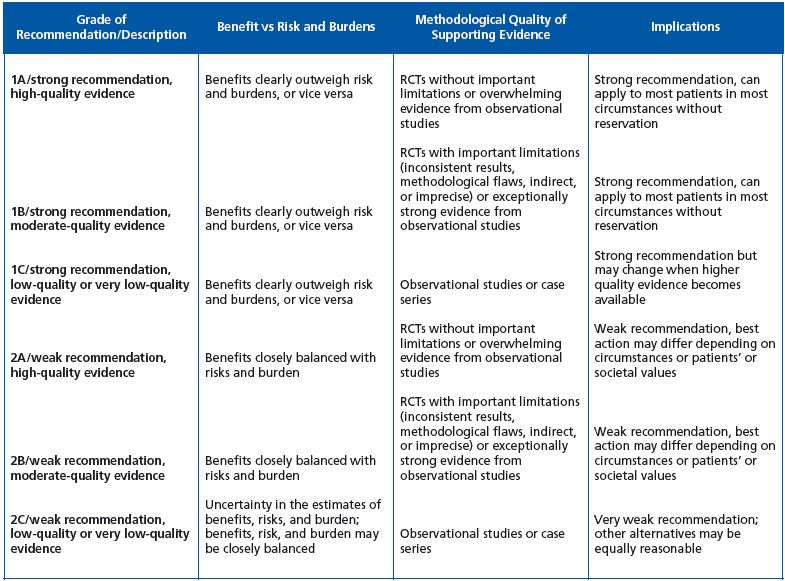
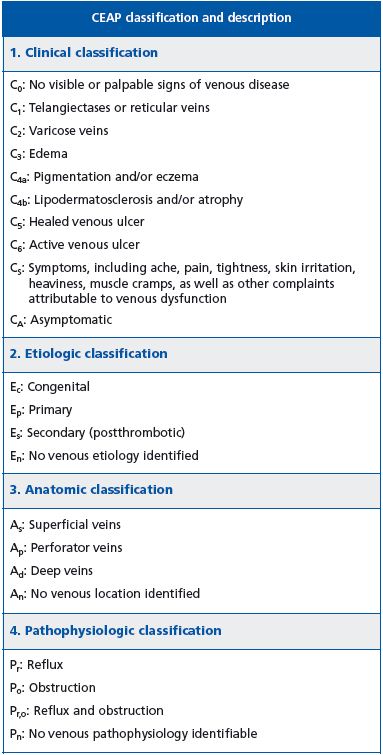
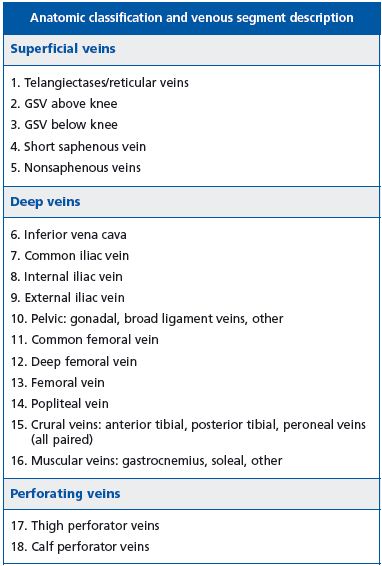
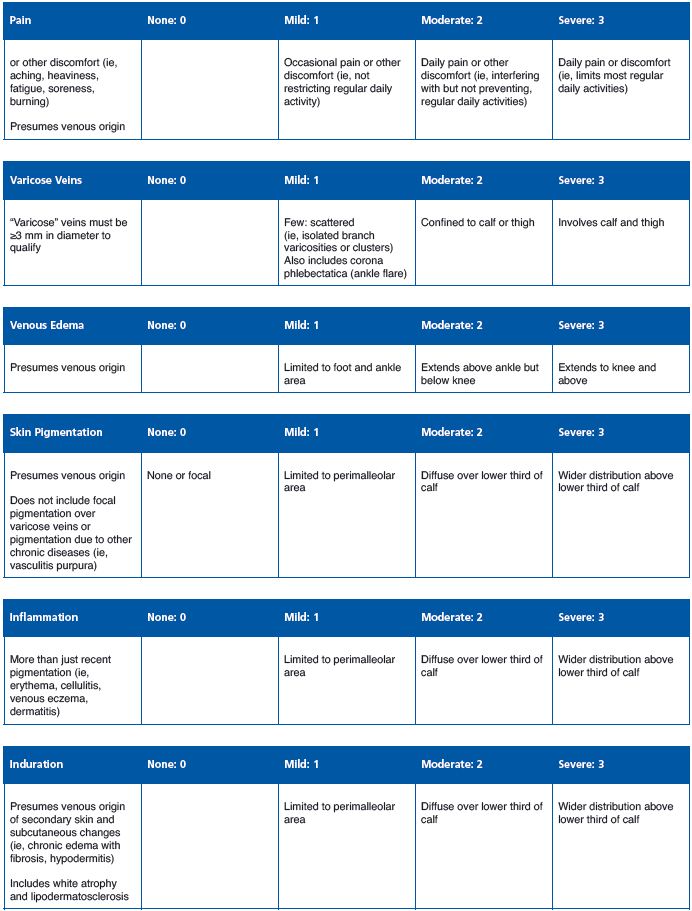
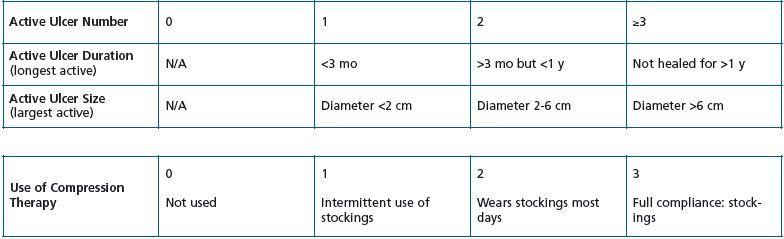
Table IV. Revised Venous Clinical Severity Score.3
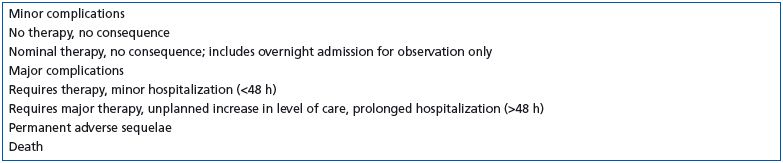
Table V. Definition of complications.4
RECOMMENDATIONS REVIEW AND COMMENTS
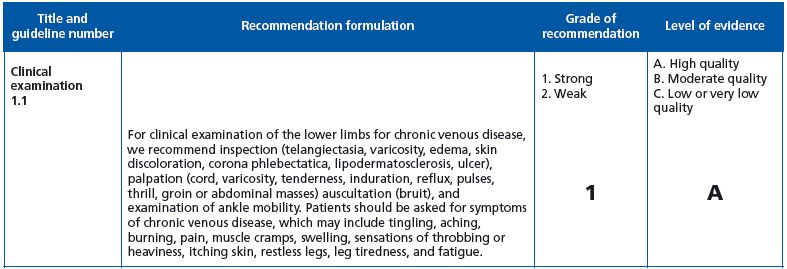
Full agreement with the grade 1A recommendation.
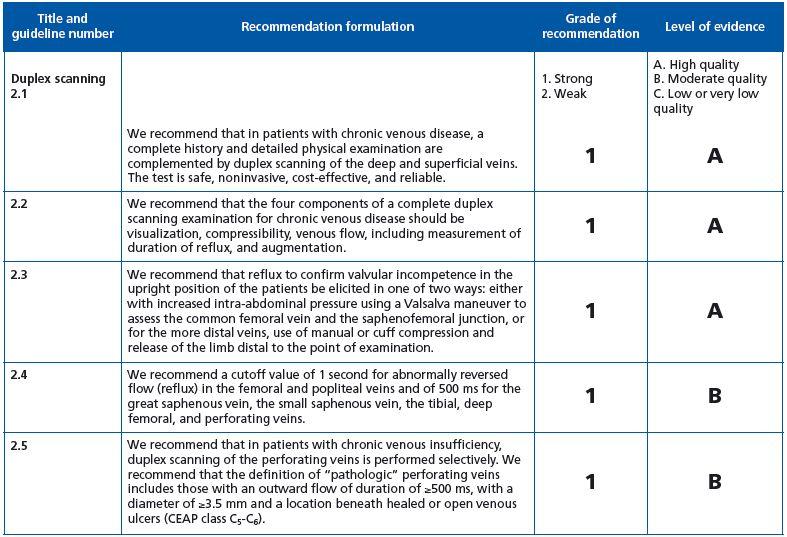
Guidelines 2-1 to 2-4: Full agreement with the quoted recommendations.
Guideline 2-5: grade 1B recommendation. One wonders why the term “pathologic” is restricted to the perforator in the presence of healed or open venous ulcer (VU). Does this mean that in the absence of VU, outward flow is not pathologic? (Figure 1)
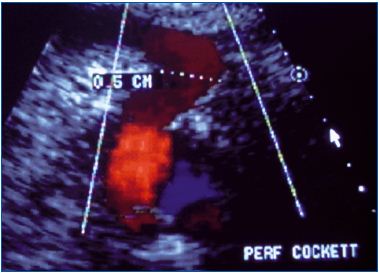
perforator in a patient presenting lipodermatosclerosis (C4b). Why
is this perforator not classified as pathologic?
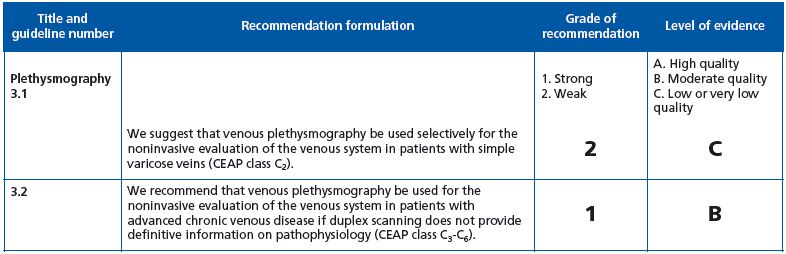
Full agreement with:
Guideline 3.1: grade 2C recommendation in C2 (uncomplicated VVs).
Guideline 3.2: grade 1B recommendation in C3-6 (complicated VVs).
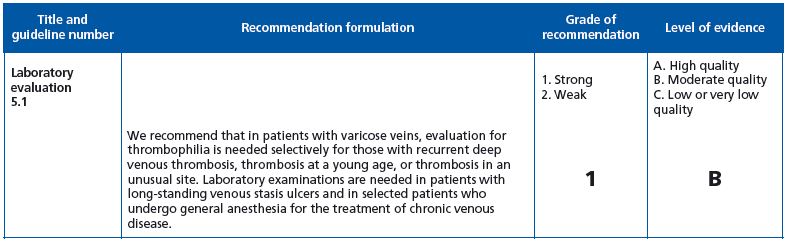
Guideline 5.1: Agreement with the grade 1B recommendation although some clinical situations are not sufficiently detailed.
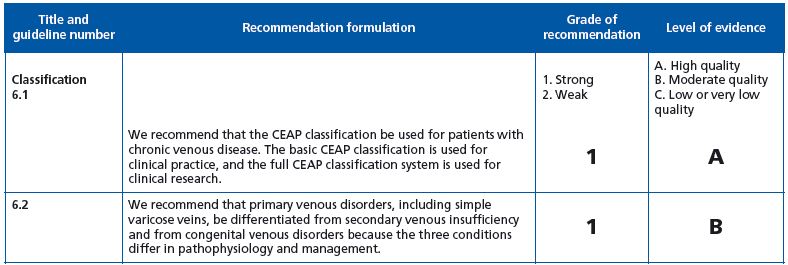
Guideline 6.1: Use of the basic and advanced CEAP classifications according to clinical practice and clinical research.2
We agree with the use of C for clinical class (grade 1A recommendation), but it should be underlined that C2 does not describe in detail the extension and importance of VVs.
Guideline 6.2: We agree with the grade 1B recommendation for the classification of VV etiology as primary, secondary, and congenital, knowing that this classification is not fully satisfying in some other types of chronic venous disease. It seems advisable to rename “secondary” as “postthrombotic.”
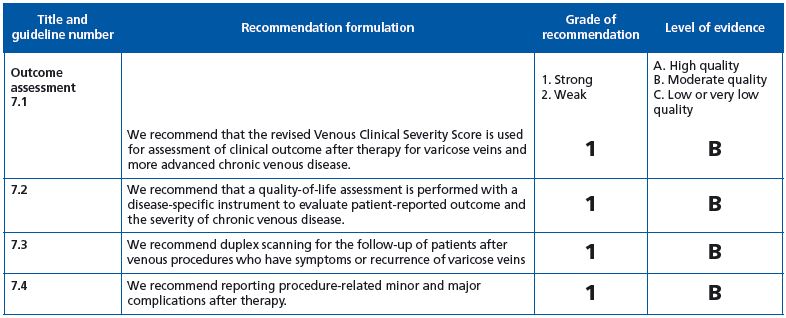
Four recommendations are listed in this section
Guideline 7.1: As previously stated in various articles—including one published in VEINews on March 22nd, 2011— the revised venous clinical severity score is an excellent tool in chronic venous insufficiency patients, but its effectiveness in C2 patients including those who are symptomatic does not deserve a grade 1B recommendation. Guidelines 7.2-7.4: Full agreement with the grade 1B recommendation.
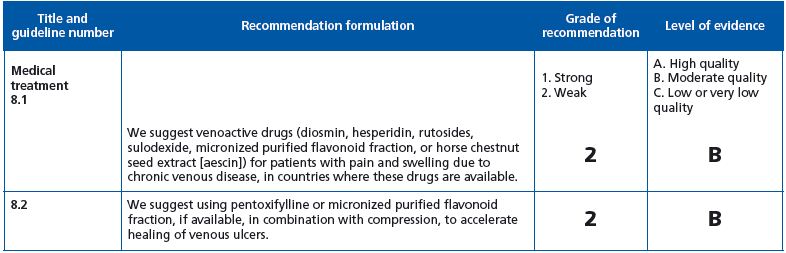
Guidelines 8.1 and 8.2: Full agreement with the grade 2B recommendation
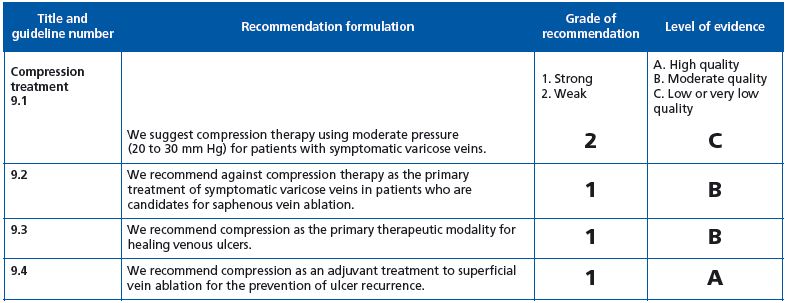
Guideline 9.1: grade 2 C recommendation. Full agreement with this very weak recommendation, as other treatments should be considered.
Guideline 9.2 and 9.3: grade 1B recommendation. Full agreement.
Guideline 9.4. To prevent ulcer recurrence in C5 patients, the grade 1A recommendation is unsatisfactory. In our opinion, if after superficial ablation no superficial/perforator/deep anomaly is present, and in the absence of edema, lipodermatosclerosis compression is not beneficial.
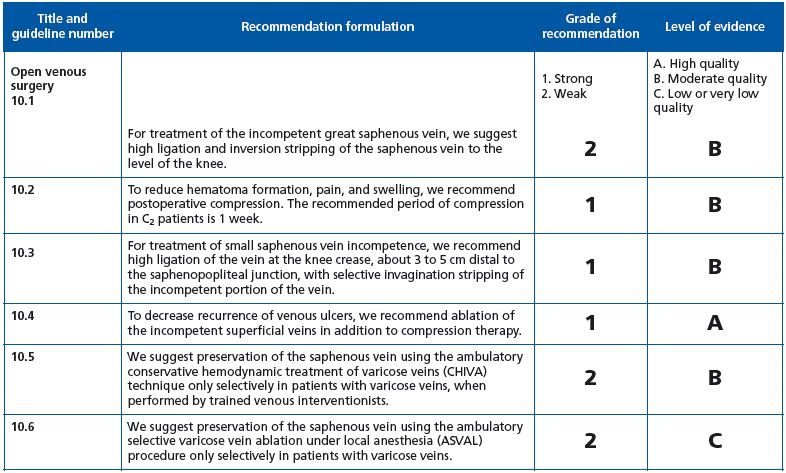
Guideline 10.1: The grade 2B recommendation seems harsh for classic GSV surgery for two reasons; firstly, because long-term RCTs comparing open surgery with thermal ablation are not available, and secondly, because open surgery performed under local tumescent anesthesia and using atraumatic techniques is less invasive than traditional procedures.
Guideline 10.2: grade 1B recommendation. Full agreement.
Guideline 10.3: grade 1B recommendation. What is the rationale for recommending nonflush ligation of the saphenopopliteal junction? As far as we know, there is no RCT comparing flush and nonflush ligation.
Guideline 10.4: grade 1A recommendation. See the comment on classic surgery in guideline 10.1.
Guideline 10.5 to 10-8: Full agreement.
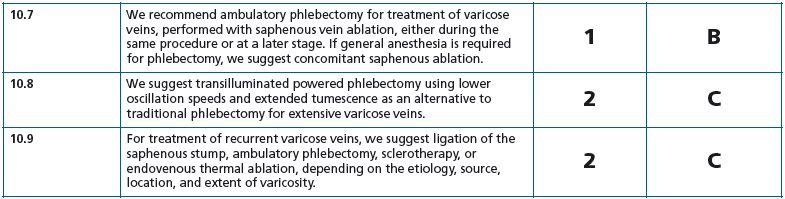
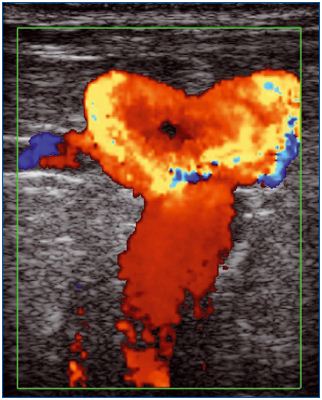
Guideline 10.9 deals with VV recurrence after open surgery termed REVAS,5 but not PREVAIT, as defined in the VEIN-TERM consensus article.6 We agree with the grade 1C recommendation as there are very few RCTs comparing the various operative treatments in this situation. Nevertheless, in practice, ultrasound-guided foam sclerotherapy is the first-line treatment used, except perhaps in the presence of a large refluxing saphenous stump (figures 2a, 2b).
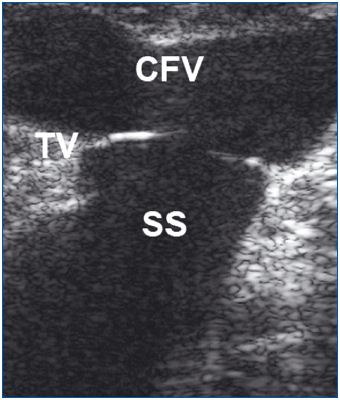
B mode. The terminal valve is identified at the saphenofemoral
junction.
CFV: common femoral vein;
SS: saphenous stump; TV: terminal valve.
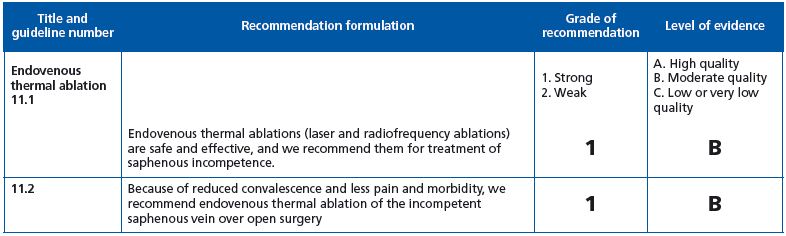
Guideline 11.1: grade 1B recommendation. Full agreement. It is worth noting that, for the authors, endothermal ablation has now become the gold standard for treating saphenous incompetence operatively, instead of HL+ stripping.
Guideline 11.2. See the comment on classic surgery in guideline 10.1
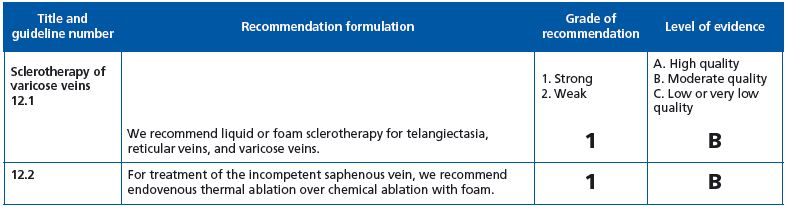
Guideline 12.1: grade 1B recommendation. Agreement for telangectasias and reticular veins, but not VVs. According to many articles, foam has given better results than liquid.
Guideline 12.2: grade 2B recommendation. Agreement with this weak recommendation, as there is no RCT comparing the long-term outcome after chemical ablation and thermal ablation.
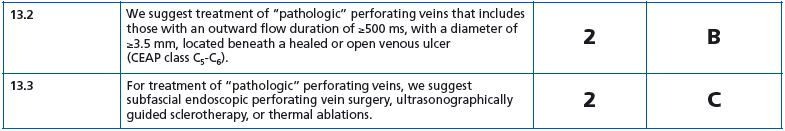
Guideline 13.1: grade 1B recommendation. Agreement
Guideline 13.2: grade 2B recommendation. Agreement
Guideline 13.3: grade 2C recommendation. Agreement
There is no RCT comparing the outcome after the different procedures.
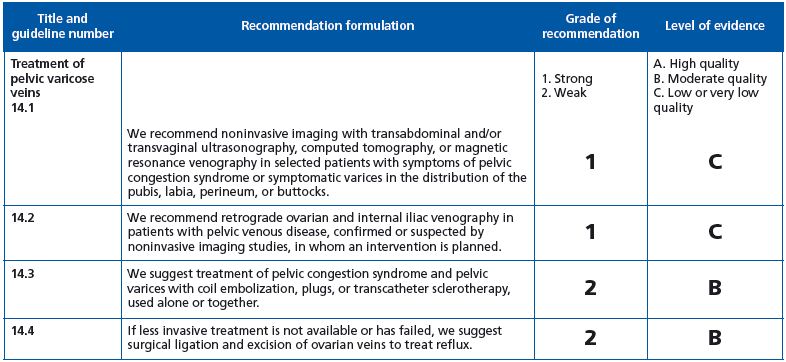
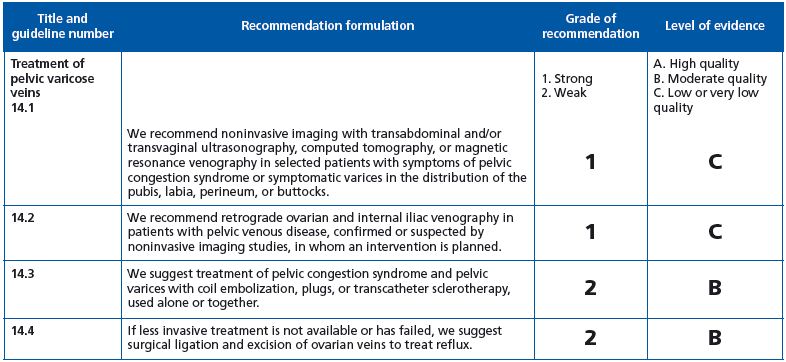
Guideline 14.1: grade 1C recommendation. Full agreement.
Guideline 14.2: grade 1C recommendation. We suggest 1B.
Guideline 14.3: grade 2B recommendation. We suggest 1C.
Guideline 14.4: grade 2B recommendation. Agreement.
CONCLUSION
The Clinical Practice Guidelines of The Society for Vascular Surgery and The American Venous Forum, published in the 2011 Journal of Vascular Surgery supplement, gathers information that had never been analyzed in depth before, and the authors deserve to be congratulated for their outstanding work.
The recommendations stated in this document should be commented by members of the international phlebology community according to their specialization, ie, angiology, surgery, dermatology, internal medicine, and phlebology, as well as in light of the health regulations in their respective countries.
Nevertheless, knowing how fast interventional procedures evolve with the development of new techniques or devices, one can bet that some of these recommendations will quickly become outdated.
The main problem with varicose veins can be summarized as follows: on the one hand, chronic venous disease—including varicose veins—evolves slowly and long-term follow-up is required to assess its outcome and management, and on the other hand, investigation and operative procedures change very fast. In other words, by the time RCT results become available, the procedures they compare have become obsolete.
REFERENCES
1. Guyatt G, Gutterman D, Baumann MH, et al. Grading strength of recommendations and quality of evidence in clinical guidelines: report from an American College of Chest Physicians task force. Chest. 2006;129:174-181.
2. Eklof B, Rutherford RB, Bergan JJ, et al. Revision of the CEAP classification for chronic venous disorders: consensus statement. J Vasc Surg. 2004;40:1248- 1252.
3. Vasquez MA, Rabe E, McLafferty RB, et al. Special revision of the venous clinical severity score. Communication of the American Venous Forum Ad Hoc Outcomes Working Group. J Vasc Surg. 2010;52:1387-1396.
4. Kundu S, Lurie F, Millward SF, et al. Recommended reporting standards for endovenous ablation for the treatment of venous insufficiency: joint statement of the American Venous Forum and the Society of Interventional Radiology. J Vasc Surg. 2007;46:582-589.
5. Perrin MR, Guex JJ, Ruckley CV, et al. Recurrent varices after surgery (REVAS), a consensus document. Cardiovasc Surg. 2000;8:233-245.
6. Eklöf B, Perrin M, Delis K, Rutherford R; VEIN-TERM Transatlantic Interdisciplinary Faculty. Updated terminology of chronic venous disorders: the VEIN-TERM Transatlantic Interdisciplinary consensus document. J Vasc Surg. 2009;49:498-501.
