Phlebolymphology N°105 – Editorial
Chronic venous disease management:
Thematic index of randomized controlled trials
Vascular Surgery; Editor in Chief of Phlebolymphology
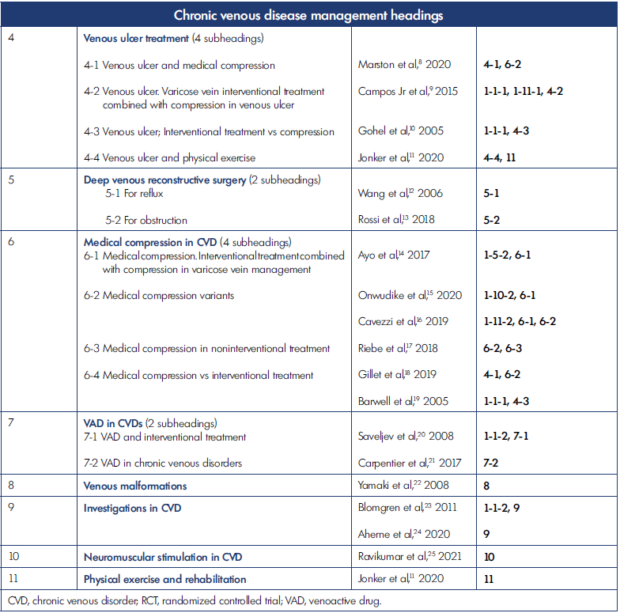
There is currently no available index on chronic venous disease (CVD) management allowing the quick and easy identification of pertinent randomized controlled trials. Furthermore, it can be difficult to determine from article titles what precise treatment–whether interventional or not–and diagnosis tool were used in the studies, which can be problematic. To address this issue, we developed an index of treatment procedures and diagnosis methods as explained below (and in a simplified version in Table I). There are currently 11 chronic venous disease management headings, as follows:
14 procedures are listed for varicose vein treatment.
All of them, except 1-9, have 2 subheadings specifying if the procedure is compared with another one or is a variant of the procedure.
Heading 1-9 is devoted to varices recurrence or more precisely to presence of varices after interventional treatment (PREVAIT) that include recurrence, varices not treated, and disease evolution when this data is available in the randomized controlled trial (RCT).
Examples:
Rasmussen LH et al. Randomized clinical trial comparing endovenous laser ablation, radiofrequency ablation, foam sclerotherapy and surgical stripping for great saphenous veins. Br J Surg. 2011;98:1079-1087. Management classification: 1-1-1, 1-5-1, 1-10-1, 1-11-1.
Morrison N et al. Five-year extension study of patients from a randomized clinical trial (VeClose) comparing cyanoacrylate closure versus radiofrequency ablation for the treatment of incompetent great saphenous veins. J Vasc Surg Venous Lymphat Disord. 2020;8(6):978-989. Management classification: 1-3-1, 1-9, 1-10-1.
Vuylsteke M et al. Endovenous laser treatment: is there a difference between using a 1500 nm and a 980 nm diode laser. A multicenter randomized clinical trial. Int Angiol. 2011;30(4):327-334. Management classification: 1-5-2.
Nyamekye IK et al. A randomised controlled trial comparing three different radiofrequency technologies: short-term results of the 3-RF Trial. Eur J Vasc Endovasc Surg. 2019;58:401-408. Management classification: 1-10-2. 2.
Example:
McCoy S et al. Sclerotherapy for leg telangiectasia—a blinded comparative trial of polidocanol and hypertonic saline. Dermatol Surg. 1999;25:381-386. Management classification: 2.
This heading groups all the RCTs dealing with perforator ablation, either comparing perforator ablation procedures or varices ablation with or without complementary perforator division.
Examples:
Pierik EG et al. Endoscopic versus open subfascial division of incompetent perforating veins in the treatment of venous leg ulceration: a randomized trial. J Vasc Surg. 1997;26:1049-1054. Management classification: 3.
Kianifard B et al. Randomized clinical trial of the effect of adding subfascial endoscopic perforator surgery to standard great saphenous vein stripping. Br J Surg. 2007;94:1075-1080. Management classification: 1-1-2, 1-9, 3.
This heading has 4 subheadings.
4-1 Venous ulcer and medical compression.
Example:
Marston WA et al. Economic benefit of a novel dual-mode ambulatory compression device for treatment of chronic venous leg ulcers in a randomized clinical trial. J Vasc Surg Venous Lymphat Disord. 2020;8:1031-1040. Management classification: 4-1, 6-2.
4-2 Venous ulcer and varicose vein interventional treatment
Example:
Campos W Jr et al. A prospective randomised study comparing polidocanol foam sclerotherapy with surgical treatment of patients with primary chronic venous insufficiency and ulcer. Ann Vasc Surg. 2015;29(6):1128-1135. Management classification: 1-1-1, 1-11-1, 4-2.
4-3 Venous ulcer. Varicose vein interventional treatment combined with compression in venous ulcer
Example:
Gohel MS et al. Randomized clinical trial of compression plus surgery versus compression alone in chronic venous ulceration (ESCHAR study)- haemodynamic and anatomical changes. Br J Surg. 2005;92:291-297. Management classification: 1-1-1, 4-3.
4-4 Venous ulcer and physical exercise
Example:
Jonker L et al. A multi-centre, prospective, randomised controlled feasibility study of plantar resistance exercise therapy for venous leg ulcers – results of the PREVUE study. Phlebology. 2020;35:237-246. Management classification: 4-4, 11.
This heading has 2 subheadings.
5-1 For reflux
Example:
Wang SM et al. Effect of external valvuloplasty of the deep vein in the treatment of chronic venous insufficiency of the lower extremity. J Vasc Surg. 2006;44:1296-1300. Management classification: 5-1.
5-2 For obstruction
Example:
Rossi FH et al. Randomized double-blinded study comparing medical treatment versus iliac vein stenting in chronic venous disease. J Vasc Surg Venous Lymphat Disord. 2018;6:183-191. Management classification: 5-2.
This heading has 4 subheadings.
6-1 Medical compression. Interventional treatment combined with compression in varicose vein management
Examples:
Ayo D et al. Compression versus no compression after Endovenous Ablation of the Great Saphenous Vein: a randomized controlled trial. Ann Vasc Surg. 2017;38:72-77. Management classification: 1-5-2, 6-1.
Onwudike M et al. Role of Compression After Radiofrequency Ablation of Varicose Veins: a randomised controlled trial. Eur J Vasc Endovasc Surg. 2020;60:108-117. Management classification: 1-10-2, 6-1.
6-2 Medical compression variants
Examples:
Cavezzi A et al. Compression with 23 mmHg or 35 mmHg stockings after saphenous catheter foam sclerotherapy and phlebectomy of varicose veins: a randomized controlled study. Phlebology. 2019;34:98-106. Management classification: 1-11-2, 6-1, 6-2.
Riebe H et al. Advantages and disadvantages of graduated and inverse graduated compression hosiery in patients with chronic venous insufficiency and healthy volunteers: a prospective, mono-centric, blinded, open randomized, controlled and cross-over trial. Phlebology. 2018;33(1):14-26. Management classification: 6-2, 6-3.
6-3 Medical compression in noninterventional treatment
Example:
Gillet JL et al. Clinical superiority of an innovative two-component compression system versus four-component compression system in treatment of active venous leg ulcers: a randomized trial. Phlebology. 2019;34:611-620. Management classification: 4-1, 6-2.
6-4 Medical compression vs interventional treatment
Example:
Barwell JR et al. Comparison of surgery and compression with compression alone in chronic venous ulceration (ESCHAR study): randomised controlled trial. Lancet. 2005;363:1854-1859. Management classification of CV: 1-1-1, 4-3.
This heading has 2 subheadings.
7-1 VAD and interventional treatment
Example:
Saveljev VS et al. Stripping of the great saphenous vein under micronized purified flavonoid fraction (MPFF) protection (results of the Russian multicenter controlled trial DEFANCE). Phlebolymphology. 2008;15:45-51. Management classification: 1-1-2, 7-1.
7-2 VAD in CVDs
Example:
Carpentier P et al. Clinical efficacy and safety of a new 1000-mg suspension versus twice-daily 500-mg tablets of MPFF in patients with symptomatic chronic venous disorders: a randomized controlled trial. Int Angiol. 2017;36(5):402- 409. Management classification: 7-2.
Example:
Yamaki T et al. Prospective randomized efficacy of ultrasound-guided foam sclerotherapy compared with ultrasoundguided liquid sclerotherapy in the treatment of symptomatic venous malformations. J Vasc Surg. 2008;47:578-584. Management classification: 8.
Examples:
Blomgren LG et al. Late follow-up of a randomized trial of routine duplex imaging before varicose vein surgery. Br J Surg. 2011;98:1112-1116. Management classification: 1-1-2, 9.
Aherne TH et al. Does longitudinal or transverse orientation of the ultrasound probe improve cannulation success in minimally invasive venous surgery: a multicentre randomised controlled trial. Phlebology. 2020;35:686-692. Management classification: 9.
Example:
Ravikumar R et al. A randomised controlled trial of neuromuscular stimulation in nonoperative venous disease improves clinical and symptomatic status. Phlebology. 2021;36:290-312. Management classification: 10.
Example:
Jonker L et al. A multi-centre, prospective, randomised controlled feasibility study of plantar resistance exercise therapy for venous leg ulcers – results of the PREVUE study. Phlebology. 2020;35:237-246. Management classification: 11.
In this classification, one or several numbers are attributed to each article; those numbers are added to the usual reference. To illustrate, all headings are listed as in Table 1 and Table 2 below. Many articles of RCTs have been attributed several numbers for CVD management classification in order to facilitate identification according to topic. This CVD management list is open to modification and can be supplemented with new treatments or investigations evaluated by RCT.
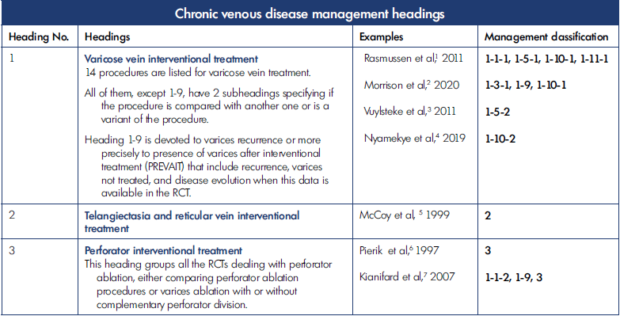
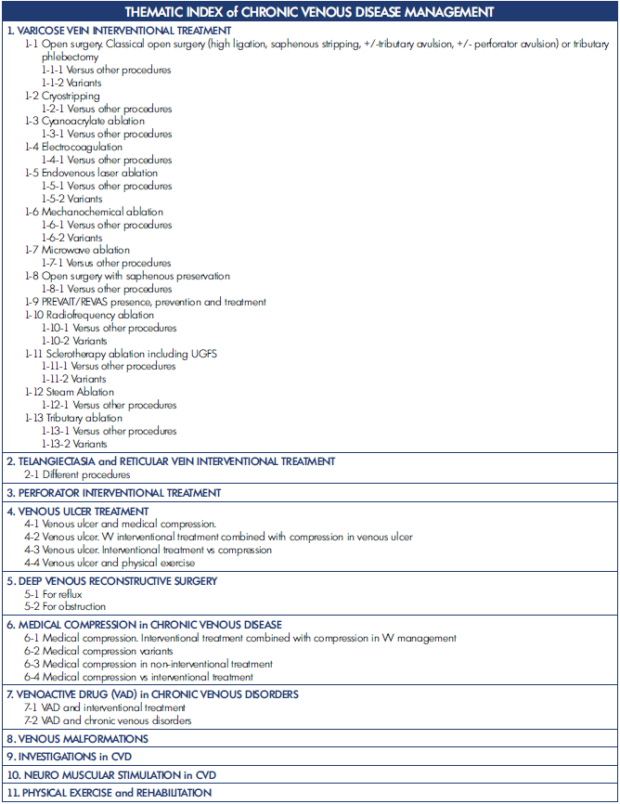
Table 2. List of topics in the Thematic index of RCTs
PREVAIT/REVAS, presence of varices after interventional treatment / recurrent varices after surgery; UGFS, ultrasound-guided foam
sclerotherapy; VV, varicose vein
Conclusion
More than 300 RCTs on CVD have been published in the last 30 years. In order to facilitate identification of the topic of a particular RCT, a modifiable index of CVD management, including treatment and diagnosis, has been created.
REFERENCES
1. Rasmussen LH, Lawaetz M, Bjoern L, Vennits B, Blemings B, Eklof B. Randomized clinical trial comparing endovenous laser ablation, radiofrequency ablation, foam sclerotherapy and surgical stripping for great saphenous veins. Br J Surg. 2011;98:1079-1087.
2. Morrison N, Gibson K, Vasquez M, Weiss R, Jones A. Five-year extension study of patients from a randomized clinical trial (VeClose) comparing cyanoacrylate closure versus radiofrequency ablation for the treatment of incompetent great saphenous veins. J Vasc Surg Venous Lymphat Disord. 2020;8(6):978-989.
3. Vuylsteke M, De Bo TH, Dompe G, Di Crisci D, Abbad C, Mordon S. Endovenous laser treatment: is there a difference between using a 1500 nm and a 980 nm diode laser. A multicenter randomized clinical trial. Int Angiol. 2011;30(4):327-334.
4. Nyamekye IK, Dattani N, Hayes W, Harding D, Holloway S, Newman J. A randomised controlled trial comparing three different radiofrequency technologies: short-term results of the 3-RF Trial. Eur J Vasc Endovasc Surg. 2019;58:401-408.
5. McCoy S, Evans A, Spurrier N. Sclerotherapy for leg telangiectasia—a blinded comparative trial of polidocanol and hypertonic saline. Dermatol Surg. 1999;25:381-386.
6. Pierik EG, van Urk H, Hop WC, Wittens CH. Endoscopic versus open subfascial division of incompetent perforating veins in the treatment of venous leg ulceration: a randomized trial. J Vasc Surg. 1997;26:1049-1054.
7. Kianifard B, Holdstock J, Allen C, Smith C, Price B, Whiteley MS. Randomized clinical trial of the effect of adding subfascial endoscopic perforator surgery to standard great saphenous vein stripping. Br J Surg. 2007;94:1075-1080.
8. Marston WA, Kirsner RS, Tallis A, et al. Economic benefit of a novel dual-mode ambulatory compression device for treatment of chronic venous leg ulcers in a randomized clinical trial. J Vasc Surg Venous Lymphat Disord. 2020;8:1031- 1040.
9. Campos W Jr, Torres IO, Simão da Silva E, Casella IB, Puech-Leão P. A prospective randomised study comparing polidocanol foam sclerotherapy with surgical treatment of patients with primary chronic venous insufficiency and ulcer. Ann Vasc Surg. 2015;29(6):1128-1135.
10. Gohel MS, Barell JR, Earnshaw JJ, et al. Randomized clinical trial of compression plus surgery versus compression alone in chronic venous ulceration (ESCHAR study)- haemodynamic and anatomical changes. Br J Surg. 2005;92:291-297.
11. Jonker L, Todhunter J, Schutter J, Halliday C, Fisher S. A multi-centre, prospective, randomised controlled feasibility study of plantar resistance exercise therapy for venous leg ulcers – results of the PREVUE study. Phlebology. 2020;35:237-246.
12. Wang SM, Hu ZJ, Li SQ, Huang XL, Ye CS. Effect of external valvuloplasty of the deep vein in the treatment of chronic venous insufficiency of the lower extremity. J Vasc Surg. 2006;44:1296-1300.
13. Rossi FH, Kambara AM, Izukawa NM, et al. Randomized double-blinded study comparing medical treatment versus iliac vein stenting in chronic venous disease. J Vasc Surg Venous Lymphat Disord. 2018;6:183-191.
14. Ayo D, Blumberg SN, Rockman CR, et al. Compression versus no compression after Endovenous Ablation of the Great Saphenous Vein: a randomized controlled trial. Ann Vasc Surg. 2017;38:72-77.
15. Onwudike M, Abbas K, Thompson P, McElvenny DM. Role of Compression After Radiofrequency Ablation of Varicose Veins: a randomised controlled trial. Eur J Vasc Endovasc Surg. 2020;60:108-117.
16. Cavezzi A, Mosti G, Colucci R, Quinzi V, Bastiani L, Urso SU. Compression with 23 mmHg or 35 mmHg stockings after saphenous catheter foam sclerotherapy and phlebectomy of varicose veins: a randomized controlled study. Phlebology. 2019;34:98-106.
17. Riebe H, Konschake W, Haase H, Jünger M. Advantages and disadvantages of graduated and inverse graduated compression hosiery in patients with chronic venous insufficiency and healthy volunteers: a prospective, mono-centric, blinded, open randomized, controlled and cross-over trial. Phlebology. 2018:33(1):14-26.
18. Gillet JL, Guex JJ, Allaert FA, et al. Clinical superiority of an innovative two-component compression system versus four-component compression system in treatment of active venous leg ulcers: a randomized trial. Phlebology. 2019;34:611-620.
19. Barwell JR, Davies CE, Deacon J, et al. Comparison of surgery and compression with compression alone in chronic venous ulceration (ESCHAR study): randomised controlled trial). Lancet. 2005;363:1854- 1859.
20. Saveljev VS, Pokrovsky AV, Kirienko AI, Bogachev VY, Zolotukhin IA, Sapelkin SV. Stripping of the great saphenous vein under micronized purified flavonoid fraction (MPFF) protection (results of the Russian multicenter controlled trial DEFANCE). Phlebolymphology. 2008;15:45-51.
21. Carpentier P, van Bellen B, Karetova D, et al. Clinical efficacy and safety of a new 1000-mg suspension versus twice-daily 500-mg tablets of MPFF in patients with symptomatic chronic venous disorders: a randomized controlled trial. Int Angiol. 2017;36(5):402-409.
22. Yamaki T, Nozaki M, Sakurai H, Takeuchi M, Soejima K, Kono T. Prospective randomized efficacy of ultrasound-guided foam sclerotherapy compared with ultrasound-guided liquid sclerotherapy in the treatment of symptomatic venous malformations. J Vasc Surg. 2008;47:578- 584.
23. Blomgren LG, Johansson G, Emanuelsson L, Dahlberg-Åkerman A, Thermaenius P, Bergqvist D. Late follow-up of a randomized trial of routine duplex imaging before varicose vein surgery. Br J Surg. 2011;98:1112-1116.
24. Aherne TH, Zafar AS, Gourlay D, et al. Does longitudinal or transverse orientation of the ultrasound probe improve cannulation success in minimally invasive venous surgery: a multicentre randomised controlled trial. Phlebology. 2020;35:686- 692.
25. Ravikumar R, Lane TR, Babber A, Onida S, Davies AH. A randomised controlled trial of neuromuscular stimulation in non- operative venous disease improves clinical and symptomatic status. Phlebology. 2021;36:290-312.