Postinterventional compression in phlebology: evidence and empirical observations
Abstract
There is almost a general agreement on the effectiveness of compression therapy in preventing unwanted side effects after procedures to remove superficial venous reflux. However, there is still a great debate on which material and compression pressure to use. In order to exert its effects, compression must occlude the vein segments ruptured by surgical or endovenous procedures. At the thigh, the critical segment in every venous intervention, the intravenous pressure is about 40 mm Hg and a higher compression pressure is necessary in order to narrow and occlude the veins. Despite this, intravenous pressure compression is infrequently applied with inelastic bandages (IB) or elastic stockings (ES), on top of eccentric compression devices, which are able to overcome the intravenous pressure and compress the vein. More often, compression is applied with simple ES exerting a 20 to 40 mm Hg pressure at the ankle, which will exert about 10 to 15 mm Hg at the thigh. This pressure is not enough to interfere with the vein diameter and occlude the vein; however, ES are claimed to be as effective as, if not better than, IB. In most studies, interface pressure exerted by compression devices is not measured, raising the suspicion that a good ES was compared with a poorly applied IB. In fact, in the few studies where compression pressure was measured, compression devices exerting a strong pressure were always more effective than ES exerting a low pressure.
When ES exerting strong pressure is compared with ES of milder pressure, or when ES is compared with no compression, the compression pressure exerted at ankle level is so light that it is as if “nothing” were to be compared with “nothing.” Good results achieved when a low compression was applied post-procedure are maybe explained by painless procedures in small veins without tributaries or avoiding tributaries avulsion.
Introduction
There is an almost general agreement that leg compression after any kind of vein procedure (surgery, endovascular laser treatment, foam sclerotherapy) is effective in preventing thrombosis of the superficial and deep vein; reducing bruising, hematoma, and hemorrhage; minimizing inflammation and pain; preventing recanalization and neovascularization; and compression therapy seems to shorten recovery time and sick leave.1-10
Despite these generally accepted benefits, there are not many well-designed, randomized, clinical trials comparing different compression devices and resulting in clear outcomes. In some clinical trials, unfortunately often with major methodological flaws, different compression devices exerting mild to very strong compression pressure were reported to be effective in preventing unwanted effects and minimizing pain, and as a consequence, there is no agreement on which kind of compression should be used.
The following will give an overview on what we currently know about compression after vein procedures. As the crucial area when dealing with vein procedures is the thigh, this paper will be focused on thigh compression.
Compression pressure to occlude the thigh veins
The main purpose of postoperative compression is to narrow or occlude the vein segments that might have been traumatized by endovenous procedures (or the segments surrounding the removed vein in open surgery) in order to keep the treated veins or the vein track free from clots. To narrow/occlude the venous lumen, the compression pressure must overcome, or at least, be very close to the intravenous pressure. Ideally, the compression pressure should increase in the standing position and during muscle contraction, and should narrow/occlude the vein lumen.11
Venous pressure in the lower leg equals the weight of the blood column by the measuring point from the right heart to the lower leg. Assuming that the specific weight of blood corresponds to that of water, a blood column of 100 cm (eg, between the calf and the right heart) would exert an intravenous pressure of 73.5 mm Hg at the midcalf. Considering a distance between the midthigh and the heart of 50 cm, pressure in the midthigh femoral vein would be about 37 mm Hg in the standing position.
Duplex examination confirms that a compression pressure higher than 70 mm Hg is necessary to occlude the calf veins and 40 mm Hg is required to occlude the thigh veins.12-15 A thigh-length elastic stocking exerting a pressure of 20 to 30 mm Hg on the lower leg will provide a pressure of 10 to 15 mm Hg at thigh level. These stockings will produce some vein lumen reduction in the supine position, but will not be able to reduce the vein diameter at thigh level in the upright position.
Clinical reports on postprocedural compression
Some authors measured the pressure exerted by compression devices applied after flush ligation and stripping of the great saphenous vein.7,16,17 They reported a significant improvement in prevention of hematoma, hemorrhage, and pain when comparing strong pressure with mild pressure–superficial and deep vein thrombosis never occurred. Travers et al7 compared strong compression using a short-stretch, adhesive bandage on one leg with low compression using a nonadhesive crevic-crepe bandage on the other leg in ten patients who underwent bilateral high ligation and stripping. The primary outcome was postsurgical bleeding measured by using 99 m Tclabeled red blood cells. He concluded that bleeding was significantly reduced in the strong compression group.
In the paper by Benigni et al,16 53 patients underwent great saphenous vein ligation and stripping and received an elastic stocking postoperatively with or without a stiff pad applied along the vein track. The pressure exerted by compression increased in the supine position from about 14 mm Hg without the pad to about 49 mm Hg when the pad was added. Pain, the primary outcome in this study, was decreased by half in the patients where the stiff pad was added.
In our experience,17 54 patients who underwent flush ligation and stripping were randomly divided into three groups to postsurgically receive one elastic stocking exerting a very light pressure (≈10 mm Hg) on the thigh; the same stocking on top of a stiff rubber foam pad firmly stuck to the skin over the vein track by means of plasters to locally increase the pressure (exerting a pressure >60 mm Hg); or a stiff inelastic adhesive bandage exerting a pressure of about 40 mm Hg. Pain, bleeding, hematoma, superficial and deep vein thrombosis were the primary outcomes. The patients treated with a stocking on top of the stiff device or an inelastic adhesive bandage had significantly better outcomes regarding pain, hemorrhage, and bleeding when compared with elastic stockings alone.
In the paper by Lugli et al,18 where compression pressure was not measured, 200 patients treated by endovenous laser ablation were randomly assigned to receive one elastic stocking exerting a pressure of 35 mm Hg at the ankle or the same stocking on top of a self-made cotton roll firmly stuck to the skin over the vein track by means of plasters to locally increase the pressure. Even if the compression pressure was not measured, it is conceivable that, when the cotton roll was added, the local pressure along the great saphenous vein was increased under the same stocking. The primary outcome in this paper was post-procedure pain. The primary outcome was significantly lower in the group treated with stronger compression and was achieved by placing the cotton roll under the stocking.
In conclusion, strong compression pressure over the treated segments is obviously more effective to control the side effects compared with lower compression. Strong compression is widely used after surgery, foam sclerotherapy, and other endovascular procedures.19-22
Bradbury et al19 suggest minimizing pain and inflammation after sclerotherapy by applying cotton rolls over the treated veins and tributaries, fixing the rolls to the skin with crevic-crepe bandages, and finally, superimposing an elastic stocking. Biemans et al20 and Rasmussen et al21,22 compared endovenous laser ablation, foam sclerotherapy, and vein stripping in 861 patients, globally. Following vein procedures, they applied some dressing over the treated area and an inelastic bandage for 2 days and then moved to an elastic stocking. Therefore, at least for the first 2 days, when the greatest part of inflammatory and hemorrhagic events takes place, a strong pressure over the thigh was exerted.
This attitude of applying a strong compression pressure following vein procedures has been questioned in other publications that claim to have a greater or similar effectiveness with strong elastic stockings vs light elastic stockings, or with elastic stockings vs bandages.2,5,23,24 Shouler et al2 compared high vs low compression stockings (40 mm Hg vs 15 mm Hg at the ankle) after varicose vein surgery and found that both were equally effective in controlling bruising and thrombophlebitis. Scurr et al,23 Bond et al,5 and Mariani et al24 compared compression exerted by elastic stockings and by different types of bandages after sclerotherapy23 or flush ligation and stripping,5,24 and did not find any difference between groups or a better reported outcome with elastic stockings.24
In other publications, post-procedure compression is considered useless.25-27 In the paper by Pittaluga and Chastanet,25 the authors performed a minor surgery with some small side branch avulsion under local anesthesia. After this procedure, an elastic stocking was donned by all the patients for the first 24 hours; then patients were divided into two groups and only one group continued with compression for 8 days without any additional benefit compared with the group without any compression.
In the second work, by Maurins et al, 94 patients were divided in three groups after laser ablation of the great saphenous vein with 1470 nm diode laser and 2 rings fiber.26 The first group wore elastic compression stockings only during the day for one week, the second group wore elastic compression stockings during the day for four weeks, and the third group did not receive compression. At the end of the observation period, the outcomes were the same–in terms of both vein occlusion and pain.
In the third work, by Hamel-Desnos et al,27 a small dose of foam polidocanol at a light concentration (4 mL at 1% on average) was injected in the great saphenous trunk. The patients were subsequently divided into two groups: (i) the “no treatment” group did not receive compression; (ii) the control group wore a light compression stocking for some hours during the day and the compliance was very poor (only 40% of patients wore the elastic compression stockings as prescribed). Therefore, it is not hard to understand that, in these conditions, no differences were found between groups.
Recommendations from the guidelines
Even if it was clearly shown that thigh veins could be compressed only by exerting a strong compression, the guidelines are quite vague in giving recommendations. Reflecting the lack of proven clinical effectiveness of one compression modality compared with others, the NICE (National Institute for Health and Care Excellence) guidelines do not provide any recommendation,28 while other guidelines indifferently suggest compression with any kind of modality (elastic stockings, elastic bandages, or inelastic bandages).29-33
Empirical observations
In our own clinical practice, we usually apply cotton rolls along the veins treated by flush ligation and stripping, endovenous laser ablation, or foam sclerotherapy. We fix them tightly to the skin by means of a crevic-crepe bandage and finally superimpose an elastic stocking exerting 23 to 32 mm Hg at the ankle. This kind of bandage is easy to apply, taking only a few minutes, and is generally well tolerated. In 30 patients, we measured the pressure exerted at the thigh with this compression device and found an average compression pressure of 33.5 mm Hg (interquartile range [IQR], 30-37) in the supine position and about 50 mm Hg (IQR, 48-53) in the standing position (Figure 1). We ask that the patients wear all of this material for as long a time as they are able to tolerate, but at least for 3 days, and then they can remove the bandages and cotton rolls and keep on only with the elastic stockings.
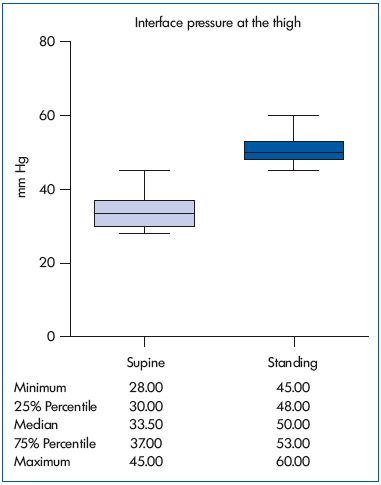
Figure 1. Compression pressure measured at the thigh in the
supine and standing position with a compression device made
up of an elastic compression stocking plus an inelastic bandage
made up of an eccentric compression device and crevic-crepe
bandage.
In our experience, some patients complain about a light discomfort caused by the compression system, but never about inflammation and pain. When it happens that poorly compliant patients remove their compression device too soon, they frequently experience pain, and this pain can be strong, requiring a new consultation. By reapplying a strong compression, pain disappears within a few hours.
Discussion
It remains to be clarified why so many colleagues are satisfied with light compression or even no compression on the thigh after vein procedures and why in some comparative studies elastic stockings exerting no more than 10 to 15 mm Hg at the thigh are reported to be equivalent to, or even more effective than, bandages that should exert a much stronger pressure.
There are some possible explanations:
1. I n the studies comparing different compression devices, compression pressure at the thigh was almost never measured. When stockings exerting a strong pressure, up to 40 mm Hg, were compared with stockings exerting a light pressure at the ankle,2 they achieved about 15 mm Hg at the thigh, which is not enough to compress the thigh veins; therefore almost nothing was compared with nothing and it is not surprising that the difference between treatments was not significant.
2. In the cases where elastic stockings were compared with bandages: (i) we do not know anything about the compression pressure of the bandages because it was not measured; (ii) we do not know what kinds of bandages were applied (elastic or inelastic); and (iii) the skill of bandagers, bandage slippage, or bandage rolling are never reported. In this condition, the suspicion that an effective elastic stocking was compared with a poorly applied bandage is very strong. Another explanation suggesting that compression pressure significantly falls with inelastic bandages,6 coming close to or lower than the compression exerted by an elastic stocking, is hard to accept. When we measured interface pressure at the thigh after vein surgery, immediately after application, and after 1 week, the pressure exerted by a correctly applied inelastic bandage, despite a massive pressure drop, was still, on average, 17 mm Hg and 31 mm Hg in supine and standing position, respectively, which was always significantly higher than that of an elastic stocking (12 and 14 mm Hg in supine and standing positions, respectively).17
3. When compression by an elastic stocking is compared with no compression, especially when using compression stockings classified according to the French standard,25,27 the pressure at thigh level is so light that practically the comparison is nothing vs nothing, which is especially true when patient compliance is poor.27
4. There are some important variables that are hardly considered in reported papers, but which could explain some satisfactory results also with low or no compression: (i) the diameter of the treated trunks and number of tributaries, and avulsion or no avulsion of tributaries; (ii) laser wavelength (new laser wavelength of 1470 nm is almost painless); (iii) the amount and concentration of sclerosing agent; (iv) the level of pain tolerance by patients; and (v) the level of acceptance of unwanted effects by surgeons. To make it very simple: we need to face two completely different situations when treating patients affected by huge great saphenous trunk and many varicosities by flush ligation and stripping, and multiple stab avulsion or tributary phlebectomy; or treating a patient with a small great saphenous vein without varices not needing stab avulsion or tributary phlebectomy by a 1470 nm laser. It is conceivable that the first patient will need strong compression pressure and the second maybe only an elastic stocking for a few days.
Conclusion
If the compression of calf veins is necessary to minimize the traumatized veins after procedures and prevent undesired effects, we need a strong compression pressure in order to overcome the intravenous pressure. This pressure needs to be higher than 40 mm Hg when standing, which is out of the range of a compression stocking. Only inelastic bandages firmly stretched or elastic stockings with some eccentric compression devices can exert this pressure range, and are to be used when large vein trunks and varices are treated.
It is conceivable that when using poorly traumatic procedures, such as new laser wavelengths or small amounts of sclerosing agent in small vein trunks without performing varicectomies stab avulsion or tributary phlebectomy, a light compression may be enough.
REFERENCES
1. Partsch H. Evidence based compression therapy. VASA. 2004;32:10-11.
2. Shouler PJ, Runchman PC. Varicose veins: optimum compression after surgery and sclerotherapy. Ann R Coll Surg Engl. 1989;71:402-404.
3. Travers JP, Makin GS. Reduction of varicose vein recurrence by use of postoperative compression stockings. Phlebology. 1994;9:104-109.
4. Rodrigus I, Bleyn J. For how long do we have to advise elastic support after varicose vein surgery? A prospective randomized study. Phlebology. 1991;6:95-98.
5. Bond R, Whyman MR, Wilkins DC, Walker AJ, Ashley S. A randomised trial of different compression dressings following varicose vein surgery. Phlebology. 1999;14:9-11.
6. Coleridge-Smith PD, Scurr JH, Robinson KP. Optimum methods of limb compression following varicose veins surgery. Phlebology. 1987;2:165-172.
7. Travers JP, Rhodes JE, Hardy JG, Makin GS. Postoperative limb compression in reduction of heamorrhage after varicose vein surgery. Ann R Coll Surg Engl. 1993;75:119-122.
8. Biswas S, Clark A, Shields DA. Randomised clinical trial of the duration of compression therapy after varicose vein surgery. Eur J Vasc Endovasc Surg. 2007;33:631-637.
9. Creton D. Neovascularisation. Phlebologie. 2008;37:134-141.
10. Munasinghe A, Smith C, Kianifard B, Price BA, Holdstock JM, Whiteley MS. Strip-track revascularization after stripping of the great saphenous vein. Br J Surg. 2007;94:840-843.
11. Partsch B, Mayer W, Partsch H. Improvement of ambulatory venous hypertension by narrowing of the femoral vein in congenital absence of venous valves. Phlebology. 1992;7:101-104.
12. Partsch B, Partsch H. Calf compression pressure required to achieve venous closure from supine to standing positions. J Vasc Surg. 2005;42:734-738.
13. Partsch B, Partsch H. Which pressure do we need to compress the great saphenous vein on the thigh? Dermatol Surg. 2008;34:1726-1728.
14. Partsch H, Mosti G. Thigh compression. Phlebology. 2008;23:252-258.
15. Partsch H, Mosti G, Mosti F. Narrowing of leg veins under compression demonstrated by magnetic resonance imaging (MRI). Int Angiol. 2010;29:408- 410.
16. Benigni JP, Allaert FA, Desoutter P, Cohen- Solal G, Stalnikiewicz X. The efficiency of pain control using a thigh pad under the elastic stocking in patients following venous stripping: results of a case-control study. Perspect Vasc Surg Endovasc Ther. 2011;23:238-243.
17. Mosti G, Mattaliano V, Arleo S, Partsch H. Thigh compression after great saphenous surgery is more effective with high pressure. Int Angiol. 2009;28:274-280.
18. Lugli M, Cogo A, Guerzoni S, Petti A. Maleti O. Effects of eccentric compression by a crossed-tape technique after endovenous laser ablation of the great saphenous vein: a randomized study. Phlebology. 2009;24:151-156.
19. Bradbury AW, Bate G, Pang K, Darvall KA, Adam DJ. Ultrasound-guided foam sclerotherapy is a safe and clinically effective treatment for superficial venous reflux. J Vasc Surg. 2010;52:939-945.
20. Biemans AA, Kockaert M, Akkersdijk GP, et al. Comparing endovenous laser ablation, foam sclerotherapy, and conventional surgery for great saphenous varicose veins. J Vasc Surg. 2013;58:727- 734.
21. Rasmussen L, Lawaetz M, Bjoern L, Blemings A, Eklof B. Randomized clinical trial comparing endovenous laser ablation and stripping of the great saphenous vein with clinical and duplex outcome after 5 years. J Vasc Surg. 2013;58:421-426.
22. Rasmussen LH, Lawaetz M, Bjoern L, Vennits B, Blemings A, Eklof B. Randomized clinical trial comparing endovenous laser ablation, radiofrequency ablation, foam sclerotherapy and surgical stripping for great saphenous varicose veins. Br J Surg. 2011;98:1079-1087.
23. Scurr JH, Coleridge-Smith P, Cutting P. Varicose veins: optimum compression following sclerotherapy. Ann R Coll Surg Engl. 1985;67:109-111.
24. Mariani F, Marone EM, Gasbarro V, et al. Multicenter randomized trial comparing compression with elastic stocking versus bandage after surgery for varicose veins. J Vasc Surg. 2011;53:115-122.
25. Pittaluga P, Chastanet S. Value of postoperative compression after surgical treatment of varicose veins. In: Proceedings from the European Venous Forum Annual Meeting. 2011; Ljubljana, Slovenia.
26. Maurins U, Rits J, Rabe E, Pannier F. Prospective randomized trial after endothemal laser ablation of great saphenous vein with 1470 nM diode laser and 2 ring fibers comparing compression therapy 0 days, 7 days and 28 days after therapy: preliminary reports. In: Proceedings from the German Society of Phlebology. Annual Meeting. 2012; Lubeck, Germany.
27. Hamel-Desnos CM, Guias BJ, Desnos PR, Mesgard A. Foam sclerotherapy of the saphenous veins: randomised controlled trial with or without compression. Eur J Vasc Endovasc Surg. 2010;39:500-507.
28. NICE clinical guideline 168. Varicose veins in the legs. The diagnosis and management of varicose veins. Available at: guidance.nice.org.uk/cg168. Accessed July 2013.
29. Pavlovic MD, Schuller-Petrovic S, Pichot O, et al. Guidelines of the First International Consensus Conference on Endovenous Thermal Ablation for Varicose Vein Disease – ETAV Consensus Meeting 2012. Phlebology. 2014 Feb 17. Epub ahead of print.
30. Rabe E, Breu F, Cavezzi A, et al; Guideline Group. European guidelines for sclerotherapy in chronic venous disorders. Phlebology. 2013;29:338-354.
31. Gloviczki P, Comerota AJ, Dalsing MC, et al; Society for Vascular Surgery; American Venous Forum. The care of patients with varicose veins and associated chronic venous diseases: clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg. 2011;53:2S-48S.
32. Khilnani NM, Grassi CJ, Kundu S, et al; Cardiovascular Interventional Radiological Society of Europe; American College of Phlebology; Society of Interventional Radiology Standards of Practice Committees. Multi-society consensus quality improvement guidelines for the treatment of lowerextremity superficial venous insufficiency with endovenous thermal ablation. J Vasc Interv Radiol. 2010;21:14-31.
33. Agus GB, Allegra C, Arpaia G, De Franciscis S, Gasbarro V. Linee Guida – Revisione 2013. Acta Phlebol. 2013;14:1- 160.