Presence of varices after operative treatment: a review
Abstract
Background: PREsence of VArices after operatIve Treatment (PREVAIT) occurs in 13% to 65% of patients and remains a debilitating and costly problem. The second part of this review aims to provide an overview of its optimal management according to published data.
Methods: A PubMed search was conducted in English and French for the years 2000-2013 by using keywords (ie, duplex scanning, endothermal ablation, neovaricoses, recurrent varicose veins after surgery [REVAS], sclerotherapy, varices recurrence, varicose vein, and varicose vein surgery).
Results: Diagnostic and operative treatment methods for managing PREVAIT were identified and their results analyzed. Indications for PREVAIT treatment are suggested according to clinical status and ultrasound information.
Conclusion: According to published data, ultrasound-guided foam sclerotherapy (UGFS) is used as a first-line treatment, yet the grade of recommendation for such a procedure is weak. It is only 1B according to European guide for sclerotherapy to improve the UGFS grade of recommendation, we suggest that larger prospective studies with a randomized controlled design be performed and supervised by an international group of experts.
Management of Prevait
Diagnostic
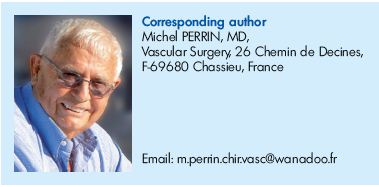
Medical history and physical examination must be completed by full duplex scanning of the three venous systems every time there is a PREsence of VArices after operatIve Treatment (PREVAIT). This investigation provides anatomic and hemodynamic data including: (i) topographical sites of recurrence that can be mapped; (ii) possible sources of reflux from the deep to the superficial venous system (Figures 1 and 2); (iii) intensity or degree of reflux; and (iv) nature of sources, keeping in mind that causes have to be classified differently if recurrence occurs in a site previously treated or not. In addition, duplex scanning (DS) gives information on perforator and deep venous systems.
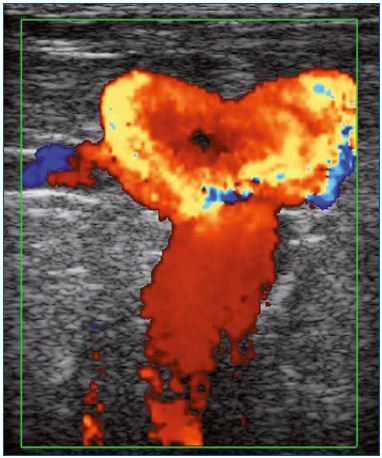
Figure 1. Presence of varices at the groin in a patient previously
treated by saphenofemoral ligation.
Color duplex ultrasound. Massive reflux induced by a Valsalva
maneuver.
Image courtesy of Dr Gillet.
One problem remains: a standardized DS investigation protocol was not universally used by the different investigators. Recently, a consensus document has been published on postoperative DS that provides a precise investigation methodology as well as a better and more precise description of the anatomic and hemodynamic anomalies according to the operative treatment modalities, surgery, or endovenous treatment.1
In a few select cases, ascending venography in 3D imaging may give complementary and valuable information. PREVAIT related to refluxing pelvic varices is investigated better by selective descending phlebography (Figure 3). Other investigation such as air plethysmography may be useful, but is never performed in routine.
Patient evaluation with quality of life questionnaires
To determine whether PREVAIT affects patients’ quality of life (QOL), the health-related QOL scores for patients can be used in different ways for clinical studies. Beresford et al compared patients presenting with recurrences after conventional surgery versus patients with untreated varicose veins.2 No survey has compared operated patients with or without PREVAIT.
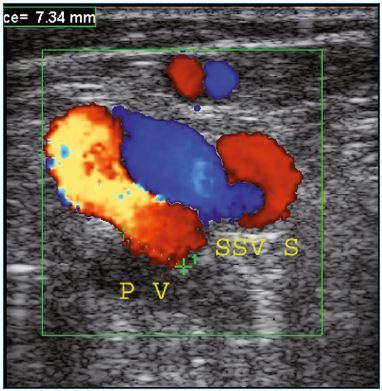
Figure 2. Presence of varices in the popliteal fossa in a patient
previously treated by saphenopopliteal ligation.
Postoperative duplex scanning identified reflux in the SSVS that
feeds the varicose network after the compression-decompression
maneuver.
Abbreviations: PV, popliteal vein; SSVS, short saphenous vein
stump.
Image courtesy of Dr Gillet.
Figure 3. Selective phlebography of the right pudendal vein
feeding the left GSV.
Abbreviations: GSV, great saphenous vein.
Image courtesy of Dr Monedero and Dr Zubicoa.
Treatment methods
Compression therapy
Compression for improvement in both symptoms and signs of varicose veins is frequently recommended, but it does not cure the disease.
Drugs
In varicose veins, venoactive drugs are prescribed mainly to improve edema and symptoms. The most commonly used are flavonoids, more particularly, the micronized flavonoids.
Operative procedures
The final objective of any operative procedure is multiple and consists of decreasing the ambulatory venous pressure, preventing worsening of chronic venous disorders, avoiding further recurrences, and of course, relieving patients of their symptoms, signs, and any unpleasant cosmetic aspects of their legs.
Operative procedures share the same goals: (i) supress reflux from deep to superficial venous systems, when reflux exists; (ii) ablate varices; (iii) in some specific cases, to suppress deep vein abnormalities to prevent new recurrences; and (iv) suppress the reflux from pelvic and gonadal varices, when it exists, since the reflux feeds recurrent varices of the lower limbs.
Sclerotherapy. This treatment has been used for a very long time for the treatment of recurrent varicose veins after surgery (REVAS). Different protocols have been used, but no comparative study was available. Recently, ultrasoundguided foam sclerotherapy (UGFS) has entered the ring, and a minimal consensus exists on the techniques, doses, concentrations, or sclerosing agents according to the location and extent of varices.3 One of the main advantages of UGFS is that the process is cheap, simple, less invasive than other operative procedures, and easily repeatable. UGFS can obliterate the refluxive varices and suppress most of the leak points between the deep and superficial venous systems, that is to say an incompetent saphenofemoral junction (SFJ), saphenopopliteal junction (SPJ), and perforator. For pelvic reflux, coils are used in association with a sclerosing agent.
Superficial vein surgery. Procedures can be classified into three groups according to their objective, and should be used in combination.
Procedures suppressing reflux from deep to superficial venous systems
Persistent reflux at the SFJ or SPJ. According to the extent of postoperative fibrosis, redo surgery may be difficult. Complications following reexploration of the groin are common.4
Patch interposition at the SFJ has been recommended for avoiding new recurrences,5 as well as closure of the cribiform fascia6 or reflected pectineal flap.7 No data are available concerning redo surgery outcomes at the SPJ.
Incompetent perforator ablation. When severe cutaneous and subcutaneous changes are present, subfascial endoscopic perforator surgery (SEPS) was the favored surgical technique, but chemical or thermal endovenous procedures can be used.
Procedures ablating refluxing varices. According to the location and type of varicose vein, various techniques can be used: stab avulsion and phlebectomy are the most used techniques, while stripping, thermal ablation, and chemical ablation are used for treating the residual saphenous trunk.
Correction of deep reflux. Various procedures whose goal is to suppress deep vein reflux should be used as valvuloplasty or valve transfer, legitimated by several studies demonstrating that primary deep axial reflux is frequently associated with REVAS.8,9
Embolization using coils and foam of the pelvic and gonadic veins. In patients whose varices are fed by pelvic or gonadic reflux, this procedure is less invasive than direct ligation.10
Results
Compression therapy and drugs
We have no specific data on the efficacy of compression treatment and drugs in patients presenting with PREVAIT.
Chemical ablation
The efficacy of liquid sclerotherapy using one protocol–the compass technique–has been reported on a large series (253 legs) with a follow-up of 3.1±1.7 years (range, 1.5- 5.7 years). The cumulative obliteration rate was sustained at >90% and there was a significant decrease in the venous dysfunction score. Unfortunately, the end point of sclerotherapy sessions was not given.11 UGFS has been reported in 4 studies.
In a series by Kakkos et al, 45 lower limbs presenting REVAS were treated by UGFS (3% sodium tetradecyl sulfate foam). After the UGFS sessions they were assessed by DS.12 In 28 legs, a reflux appeared at the level of the groin, in 5 legs at the perforator vein level, and isolated GSV in the rest of legs. Despite further sclerotherapy (single session with an injection of 6 mL in 58% of legs; ≥3 treatment sessions in 11%), complete occlusion at the end of treatment was achieved in only 39 of the 45 retreated lower limbs (87%).12
Darke and Baker treated recurrent GSV varices in 18 legs with UGFS (3% polidocanol foam). Persistent or reconstituted GSV trunks were seen in all legs. In the 6 weeks following treatment, clinical examination of re-treated legs and DS were performed. One treatment was sufficient to reach a complete occlusion in 10 legs, while 2 treatments had to be done in a further 5 legs. The 3 remaining legs had partial occlusion after 1, 2, or 3 treatments.13
Coleridge Smith reported the outcome of a series of 267 recurrent varices due to incompetence of the GSV managed by UGFS (mostly 3% STS foam). A total of 106 legs (40%) were reviewed at a mean follow-up interval of 11 months after treatment. The GSV had remained obliterated in 98/106 (92%); better than the 86% occlusion rate seen in primary incompetence.14
O’Hare et al reviewed 32 recurrent veins at 6 months after UGFS (3% STS foam). Occlusion rate on DS was 72% (23/32), and 88% (28/32) of the patients were satisfied with the results. There was no significant difference in occlusion rates between primary (45/60, 75%) and recurrent (23/32, 72%) veins. Unfortunately, information regarding the type of recurrence treated is missing.15
The most convincing data was the Birmingham’ series. A total of 91 patients presenting with symptomatic recurrent great saphenous varicose veins were treated by 1 or 2 UGFS sessions. At a 1-year follow-up, above the knee reflux was eradicated in 81/88 lower limbs and below the knee reflux in 72/80 legs. Unfortunately, no data were provided concerning the presence or absence of symptoms and varices.16
Surgery
Surprisingly, very few data are available on the results provided by redo surgery in patients investigated preoperatively with DS. We reported a series of 145 limbs with a follow-up of 5 to 6 years. All had major reflux from the deep system at the SFJ or SPJ feeding recurrent varices that were treated by surgery. Postoperative sclerotherapy was performed in all patients during the first 2 years. An external audit revealed a global objective improvement of 85%, but there was better improvement in signs and symptoms than cosmetic appearance.17
The results of 2 studies using an interposition patch for treating recurrence at the SFJ have been published. Creton used this procedure without resection of the groin cavernoma, but with combined resection of varices (saphenous trunks and/or tributaries) had only 4.2% of recurrences at the SFJ at a mean 4.9-year follow-up (range, 3-7 years) in 119 extremities. Nevertheless, 22.6% of patients had diffuse varices, with a new site of incompetence between the deep and femoral systems.18
De Maeseneer et al compared the results at 5 years of 2 nonrandomized groups with and without a patch, respectively, group 1 and 2 in a prospective study. All patients had recurrent SFJ incompetence. At 5 years, thigh varicosity recurrences were observed in 58% of group 2 versus 26% of group 1.19
Thermal ablation
Fassiadis et al described his clinical experience on the use of radiofrequency ablation (RFA) in 18 treated legs for recurrent GSV. Recurrences were due to neovascularization at the SFJ in 15 legs, a persisting midthigh perforator in 2 legs, and a refluxing anterior thigh branch reconnecting with the GSV in 1 leg. None of the 18 legs had recanalization of the GSV at 1 month, and all patients returned to daily activities within 3 days. At 12 months, the occlusion rate was also 100% in the 16 follow-up patients. The only complication was a temporary sensory disturbance at the inner thigh in one-third of patients.20
Hinchliffe et al reported a randomized control trial in 16 patients with recurrent varices initially treated by isolated SFJ ligation.21 For each patient, 1 leg was selected at random to receive redo high ligation (HL) + conventional stripping and the other RFA. RFA treatment was faster than traditional redo groin surgery (25.5 min vs 40 min; P=0.02), and caused less pain and bruising. On DS examination at a 12-month follow-up, 15 lower limbs in the group treated by RFA had complete GSV occlusion, 3 had partial occlusion. In the group treated by surgery, complete GSV stripping was reported in 14/16 lower limbs. The authors were in favor of RFA this was justified by shorter operative time and lesser postoperative bruising and pain.21
Van Groenendael et al22 retrospectively compared outcomes of 2 different procedures in 216 patients with a recurrent varicosity of the GSV. A total of 149 underwent conventional surgery consisting of redo HL+incompetent GSV or tributary phlebectomy and 67 patients were treated with endovenous laser ablation (EVLA).17 All patients had previously been treated at least once with a saphenofemoral disconnection (SFD) with or without stripping of the GSV. Of the surgically treated legs, 87% had previously been stripped, while there were 57% who underwent EVLA. The conventional surgery was performed successfully in all legs and success was achieved in 100% of the EVLA legs. All treated veins remained occluded postoperatively according to the DS made an average of 8 weeks after EVLA in 46 legs (69%).
After a follow-up period of an average of 13.5 months in the conventional surgery group and of 15.0 months in the EVLA group, clinical recurrences occurred in 26% of the surgically-treated limbs and in 12% of the EVLA-treated limbs (P=0.024). This was no longer significant after correction for the length of follow-up. It must be highlighted that no definition was given for “clinical recurrence” by the authors and that repeated DS investigations were not performed. The postoperative pain score was significantly lower in the surgery group than in the EVLA group (P=0.02), and the median duration of postoperative pain was shorter (4.5 days in the surgery group vs 7 days in the EVLA group; P=0.03), but the use of nonsteroidal anti-inflammatory drugs was significantly higher in the surgical group. The authors concluded that if anatomically suitable EVLA is a good treatment alternative for recurrent GSV, only 31% of patients were suitable for EVLA in their series.22
In a series of 42 patients presenting PREVAIT in the SSV territory, 26 were treated by EVLA and 16 by surgery including redo SPJ ligation+SSV ablation}tributary phlebectomy. After correction for the follow-up duration, the difference in terms of results did not reach statistical difference.23
Embolization
At a 6-month follow-up, 90% of 215 patients treated by embolization of gonadal and pelvic veins were significantly improved in both signs and symptoms.10 Conversely, Castenmiller et al, with a mean 1.8-year follow-up (range, 1-3.5 years), 33 patients presenting PREVAIT after previous surgical treatment of lower varices disappeared only in 12% (4/33) after embolization. The explanation, as suggested by the authors, may be related to inadequate treatment of incompetent pelvic veins as only ovarian veins were treated by embolization.24,25
Abstract
Indications for treating Prevait patients
Patients complaining of symptoms
They present symptoms and/or esthetic concerns, and/or signs of chronic venous disease (C2-C6). In all cases, these patients need to be investigated by DS.
Subjects attending a routine follow-up
The decision whether to undertake DS, or not, depends on the presenting complaint and physical findings. In practice, DS is usually done.
Asymptomatic patients
When hemodynamic or anatomic abnormalities are found in asymptomatic patients without severe signs, who are not concerned by their minor varices as cosmetic problems, the decision to treat depends of the severity of the noninvasive findings. In all cases, follow-up is required knowing that abnormal DS findings precede symptoms and signs.
Symptomatic patients
In these patients presenting PREVAIT and hemodynamic anomalies, operative treatment must be considered. Although there is no RCT comparing redo surgery with chemical ablation, there is a consensus for treating them with UGFS as a first-line treatment for reasons exposed in the methods evaluation.16,24 The European guidelines for sclerotherapy in chronic venous disorders gives a recommendation grade 1B in PREVAIT.3 In very few cases, when DS reveals an intact and large incompetent saphenous stump at the SFJ or SPJ with a massive reflux filling the varicose network (Figure 1), redo surgery at the junction should be considered in combination with UGFS.
Patients in CEAP class C4b-C6, with PREVAIT and primary deep vein axial reflux
UGFS and valvuloplasty, in association, must be considered in active patients reluctant to wear lifelong compression or with a recurrent ulcer.
Guidelines for prospective studies
In order to know the prevalence and annual incidence of PREVAIT after nonconservative treatment, we need prospective, detailed, and well-documented studies from the outset of surgical treatment as was done in the series by Kostas.26 These studies may give information on: (i) the value of routine postoperative scanning in the early detection of persisting reflux; (ii) the relationship between hemodynamics and clinical recurrence; and (iii) the possible role of compression therapy and/or complementary postoperative sclerotherapy in preventing recurrences.
These studies may use both the updated CEAP and REVAS classification and a QOL questionnaire. Regarding the choice of the procedure, UGFS should be the first-line treatment for PREVAIT according to its satisfying outcomes. This method was assigned a 1B recommendation in the European Guidelines,2 despite the lack of RCTs comparing UGFS versus other methods–such studies are difficult to implement.
Conclusion
PREVAIT is a frequent condition frustrating both patients and physicians and has been poorly evaluated. In order to build a scientifically convincing evidence base and to achieve a greater degree of comparability between studies, an international consensus on conformity is required.
1. De Maeseneer M, Pichot O, Cavezzi A, et al. Duplex ultrasound investigation of the veins of the lower limbs after treatment for varicose veins: UIP Consensus Document. Eur J Vasc Endovasc Surg. 2011;42:89-102.
2. Beresford T, Smith JJ, Brown L, Greenhalgh RM, Davies AH. A comparison of health-related quality of life of patients with primary and recurrent varicose veins. Phlebology. 2003;18:35- 37.
3. Rabe E, Breu FX, Cavezzi A, Coleridge Smith P, Frullini A, Gillet JL. European guidelines for sclerotherapy in chronic venous disorders. Phlebology. 2013;28:308-319.
4. Hayden A, Holdsworth J. Complications following re-exploration of the groin for recurrent varicose veins. Ann R Coll Surg Engl. 2001;83:272-273.
5. De Maeseneer MG, Vandenbroeck CP, Van Schil PE. Silicone patch saphenoplasty to prevent repeat recurrence after surgery to treat recurrent saphenofemoral incompetence: long-term follow-up study. J Vasc Surg. 2004;40:98- 105.
6. De Maeseneer MG, Philipsen TE, Vandenbroeck CP, et al. Closure of the cribriform fascia: an efficient anatomical barrier against postoperative neovascularisation at the saphenofemoral junction? A prospective study. Eur J Vasc Endovasc Surg. 2007;34:361-366.
7. Gibbs PJ, Foy DM, Darke SG. Reoperation for recurrent saphenofemoral incompetence: a prospective randomised trial using a reflected flap of pectineus fascia. Eur J Vasc Endovasc Surg. 1999;18:494-498.
8. Guarnera G, Furgiuele S, Di Paola FM, Camilli S. Recurrent varicose veins and primary deep venous insufficiency: relationship and therapeutic implications. Phlebology. 1995;10:98-102.
9. Almgren B, Eriksson I. Primary deep vein incompetence in limbs with varicose veins. Acta Chir Scand. 1989;155:455- 460.
10. Leal Monedero J, Zubicoa Ezpeleta S, Castro Castro J, Calderón Ortiz M, Sellers Fernández G. Embolization treatment of recurrent varices of pelvic origin. Phlebology. 2006;21:3-11.
11. McDonagh B, Sorenson S, Gray C, et al. Clinical spectrum of recurrent postoperative varicose veins and efficacy of sclerotherapy management using the compass technique. Phlebology. 2003;18:173-185.
12. Kakkos SK, Bountouroglou DG, Azzam M, Kalodiki E, Daskapoulos M, Geroulakos G. Effectiveness and safety of ultrasoundguided foam sclerotherapy for recurrent varicose veins: immediate results. J Endovasc Ther. 2006;13:357-364.
13. Darke SG, Baker SJA. Ultrasound-guided foam sclerotherapy for the treatment of varicose veins. Br J Surg. 2006;93:969- 974.
14. Coleridge Smith P. Chronic venous disease treated by ultrasound guided foam sclerotherapy. Eur J Vasc Endovasc Surg. 2006;32:577-583.
15. O’Hare JL, Parkin D, Vandenbroeck CP, Earnshaw JJ. Mid term results of ultrasound guided foam sclerotherapy for complicated and uncomplicated varicose veins. Eur J Vasc Endovasc Surg. 2008;36:109-113.
16. Darvall KA, Bate GR, Adam DJ, Silverman SH, Bradbury AW. Duplex ultrasound outcomes following ultrasound-guided foam sclerotherapy of symptomatic recurrent great saphenous varicose veins. Eur J Vasc Endovasc Surg. 2011;42:107- 114.
17. Perrin M, Gobin JP, Grossetete C, Henri F, Lepretre M. Valeur de l’association chirurgie itérative-sclérothérapie après échec du traitement chirurgical des varices [in French]. J Mal Vasc. 1993;18:314-319.
18. Creton D. A nondraining saphenous system is a factor of poor prognosis for long-term results in surgery of great saphenous vein recurrences. Dermatol Surg. 2004;30:744-749.
19. De Maeseneer MG, Tielliu IF, Van Schil PE, De Hert SG, Eyskens EJ. Clinical relevance of neovascularization on duplex ultrasound in long term follow up after varicose vein operation. Phlebology. 1999;14:118-122.
20. Fassiadis N, Kianifard B, Holdstock JM, Whiteley MS. A novel approach to the treatment of recurrent varicose veins. Int Angiol. 2002;21:275-276.
21. Hinchliffe RJ, Uhbi J, Beech A, Ellison J, Braithwaite BD. A prospective randomised controlled trial of VNUS closure versus surgery for the treatment of recurrent long saphenous varicose veins. Eur J Vasc Endovasc Surg. 2006;31:212- 218.
22. van Groenendael L, van der Vliet JA, Flinkenflögel L, Roovers EA, van Sterkenburg SM, Reijnen MM. Treatment of recurrent varicose veins of the great saphenous vein by conventional surgery and endovenous laser. J Vasc Surg. 2009;50:1106-1113.
23. van Groenendael L, Flinkenflögel L, van der Vliet JA, Roovers EA, van Sterkenburg SMM, Reijnen MMPJ. Conventional surgery and endovenous laser ablation of recurrent varicose veins of the small saphenous vein: a retrospective clinical comparison and assessment of patient satisfaction. Phlebology. 2010;25:151-157.
24. Castenmiller PH, de Leur K, de Jong TEAM, van der Laan L. Clinical results after coil embolization of theovarian vein in patients with primary and recurrent lower-limb varices with respect to vulval varices. Phlebology. 2013;28:234-238.
25. Perrin M, Gillet JL. Recurrent varices at the groin and popliteal fossa after surgical treatment [in French]. J Mal Vasc. 2006;31:236-246.
26. Kostas TT, Ioannou CV, Veligrantakis M, Pagonidis C, Katsamouris AN. The appropriate length of great saphenous vein stripping should be based on the extent of reflux and not on the intent to avoid saphenous nerve injury. J Vasc Surg. 2007;46:1234-1241.