Rationale for surgery in the treatment of venous ulcer of the leg
SUMMARY
Venous ulcer of the leg is the most severe clinical presentation of chronic venous insufficiency. The aim of this article is to review the disease in terms of evidence-based medicine in order to determine the potential of surgery as a component of efficient treatment.
OVERVIEW
In leg ulcer, the venous etiology is more frequent than an arterial, combined (arterial and venous) or nonvascular etiology. A venous etiology accounts for 70% to 80% of cases, depending on whether or not combined ulcers are included.
A venous ulcer (VU) of the leg may be defined as a full thickness defect in the skin most frequently at the ankle that fails to heal spontaneously sustained by chronic venous disease.
VU is the most severe complication of chronic venous disease (CVD). It is therefore not surprising that the CEAP classification system allocates the highest clinical classes (C5-C6). Similarly, in the American Venous Forum’s1 clinical severity score, ulcer contributes almost one third of the severity points (9/30). The prevalence of active venous ulcer is of the order of 0.2% to 0.3% in the adult population of Western countries.2 However, if subjects whose ulcers have healed are also taken into account, the C5-C6 prevalence is between 1% and 1.5%. The prevalence is two- to threefold higher in women than in men, and increases with age.
The incidence is less well documented, but is reported to be of the order 0.035% per year in subjects aged over 45 years.
Venous ulcer gives rise to substantial health care expenditures.
PATHOPHYSIOLOGICAL REVIEW
A constant finding in patients presenting with chronic venous insufficiency (CVI) and, particularly, the severe form, VU, consists of elevated venous pressure in ambulatory settings. The increase in ambulatory venous pressure may be related to two pathophysiological factors: reflux and obstruction, or a combination of those two factors.
The pathophysiological abnormalities may affect one of the three venous systems (superficial, deep, and perforating veins) in isolation or a combination of those systems. The distribution of the various presentations is shown in Table I. It can be seen that, in about two thirds of cases, reflux affects several systems. The last important factor to be determined is the etiology. Doppler ultrasound investigation of leg ulcers, if VU only are considered, shows that, in 40% to 50% of cases, the primary etiology is located in the superficial venous network (with or without the perforators), ie, primary varices.8 It is thus undeniable that the postthrombotic syndrome (PTS) constitutes a much less frequent etiology than previously believed.
In combined ulcer, the tissue ischemia resulting from arterial disease acts jointly with the permanently increased orthostatic venous pressure.
Precise determination of the anatomical lesions and pathophysiological disorders is essential since the therapeutic indications and, more particularly, the surgical options are based on those data.
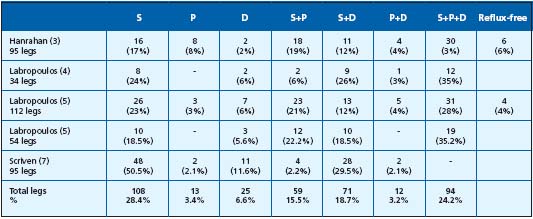
Table I. Reflux distribution in the three venous systems of the legs in patients presenting with venous ulcer. Superficial venous insufficiency
(SVI) was identified in 86.8% of cases, deep venous insufficiency (DVI) in 52.7% and perforator insufficiency (PI) in 46.3%. SVI and DVI were concomitantly present in 43% of cases, SVI and PI in 39.7% of cases and DVI and PI in 27.4% of cases.
CLINICAL PRESENTATION
The diagnosis of ulcer is essentially clinical, but clinical feature does not always enable determination of the etiology or, most importantly, the anatomical lesions and pathophysiological disorders. The latter are determined by investigations, which are scheduled in relation to potential surgical treatment (Figure 1).
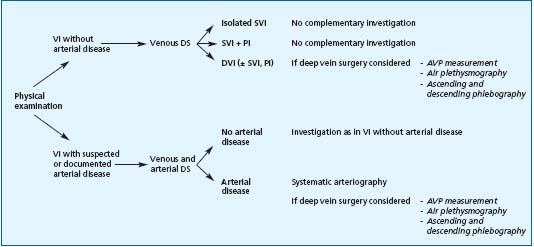
Figure 1. Investigation algorithm.
Abbreviations: DS: Duplex scan, VI: venous insufficiency, SVI: superficial venous insufficiency, PI: Perforator insufficiency, DVI: deep venous insufficiency, AVP: ambulatory venous pressure.
TREATMENT
Treatment has a dual objective: obtaining ulcer healing, then preventing recurrence. Accordingly, the permanent increase in venous pressure must be reduced or eliminated. In the event of concomitant arterial disease, it is also necessary to increase the arterial tissue perfusion pressure.
The surgical methods may be classified as a function of their aims.
Among the methods used to promote VU healing are excision of the ulcer and its inflammatory base in the hypodermis ie, lipodermatosclerosis, and its variation, such as shave therapy (Figure 2 a, b, c).
The methods used to prevent VU recurrence are classified in terms of the venous system to be treated: excision of the pathological superficial venous network, ligation of incompetent perforators, and restorative surgery on the deep vein network with the aim of alleviating obstruction and/or reflux. In addition to those direct methods, German authors recommend fasciotomy.
In combined ulcer, open-wound arterial reconstruction and/or transluminal procedures may be employed.

Figures 2a-c: Shave therapy – Figure 2a: Circular chronic venous ulcer of the lower half of the leg – Figure 2b: Physical feature after shave therapy procedure – Figure 2c: Healed ulcer: Excision of lipodermatosclerotic tissue has enhanced the “champagne bottle” aspect.
The results of surgery
Ulcer healing
A controlled study has shown that surgical treatment of varices associated with compression did not procure any advantage over compression alone with respect to ulcer healing.9 In recalcitrant ulcers, resection of the inflammatory base in the hypodermis, and skin grafting enabled ulcer healing on 60% to 80% of cases.
Ulcer recurrence prevention. Surgical treatment of superficial venous insufficiency was compared with compression in a controlled study10 with 1 year of follow-up. The benefit in terms of absence of ulcer recurrence was only significant (P=0.008) in the absence of concomitant deep venous insufficiency (DVI).
It is difficult to assess the results of perforator surgery since analysis of various series reported shows that the procedure was almost always associated with other surgical procedures.
At 2 years’ follow-up surgical treatment of deep vein obstructive syndromes had procured 62% recurrence-free ulcer healing in patients who had not experienced healing or presented with recurrence on conservative treatment.11 Surgical treatment of deep vein reflux is credited with various rates of absence of ulcer recurrence at 5 years’ follow-up, depending on the etiology. In primary reflux, the rate is about 70% while in PTS the rate is between 40% and 70%.12
In combined ulcer the success of arterial surgery is the decisive factor. In Treiman’s series,13 the presence of DVI and, particularly, PTS constituted a negative predictive factor.
THE INDICATIONS FOR SURGERY
(Figure 3)
It must be borne in mind that concomitant diseases must always be treated, particularly diabetes mellitus and obesity. When the physical examination shows restricted mobility of the ankle, physiotherapy (active and passive joint mobilization) is to be prescribed, as soon as the ulcer is no longer painful or when it has healed.
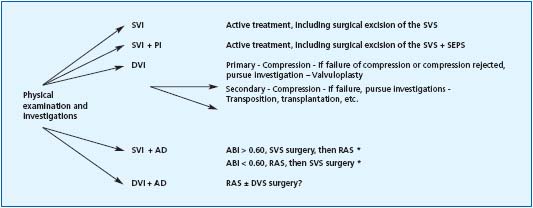
igure 3. Surgical treatment algorithm for the prevention of ulcer recurrence.
Abbreviations: AD: arterial disease, RAS: restorative arterial surgery, SEPS: subfascial endoscopic perforator surgery, DS: Duplex scan, DVS: deep venous system PI: perforator insufficiency, VI: venous insufficiency, ABI: ankle/brachial index, SVI: superficial venous insufficiency, SVS: superficial venous system
* according to Treiman (13)
The surgical indications may be summarized as follows: in venous ulcer, surgery is exceptionally justified in order to obtain ulcer healing. Surgery to eradicate primary varices is indicated in the absence of deep venous insufficiency in order to prevent ulcer recurrence. Conversely, the management of perforator disease is more problematic, but a degree of consensus exists with regard to endoscopic ligation of large-caliber perforators of the legs. The indications for reconstructive surgery of the deep vein network remain controversial. Surgery may be envisaged following failure of conservative treatment.
In combined ulcers, reconstructive arterial surgery is necessary, when potentially feasible, in order to obtain ulcer healing and to prevent recurrence.
Aknowledgment: thanks to HJ Hermanns MD for providing the figures on shave therapy
REFERENCES
2. Fowkes FGR. Epidemiology of venous ulcer. Phlébologie.1999; 52:377-382.
3. Hanrahan LM, Araki, CT, Rodriguez AA, Kechejian JK, LaMorte WW, Menzoian JO. Distribution of valvular incompetence in patients with venous ulceration. J Vasc Surg. 1991:13:805-12.
4. Labropoulos N, Giannoukas AD, Nicolaides AN, Ramaswani G, Leon M, Burke P. New insights into the pathophysiologic condition of venous ulceration with color-flow duplex imaging: implications for treatment. J Vasc Surg. 1995;22:45-50.
5. Labropoulos N, Leon M, Geroulakos G, Volteas N, Chan P, Nicolaides AN. Venous hemodynamic abnormalities in patients with leg ulceration. Am J Surg. 1995;169:572-574.
6. Labropoulos N. Clinical correlation to various patterns of reflux. Vasc Surg. 1997;31;242-248.
7. Scriven JM, Harsthorne T, Bell PR, Naylor AR, London NJ. Single-visit venous ulcer assessment clinic: the first year. Br J Surg. 1997;84:334-336.
8. Grabs AJ, Wakely MC, Nyamekye I, Ghauri ASK, Poskitt KR. Colour duplex ultrasonography in the rational management of chronic venous ulcers. B J Surg. 1996;83:1830-1832.
9. Guest M, Smith JJ, Tripuraneni G,Howard A, et al. Randomized clinical trial of varicose vein surgery with compression versus compression alone for the treatment of venous ulceration. Phlebology. 2003:18:130-136.
10. Barwell J, Davies C, Tailor M, Deacon J, Usher DC, Mitchell JJ et al. The ESCHAR venous ulcer study: a randomised controlled trial assessing venous surgery in 500 leg ulcers (abstract) B J Surg. 2003;90:497.
11. Raju S, Owen Jr S, Neglen P. The clinical impact of iliac venous stents in the management of chronic venous insufficiency. J Vasc Surg. 2002;38:8-15.
12. Perrin M. Reconstructive surgery for deep venous reflux. Cardiovasc Surg. 2000;8:246-255.
13. Treiman GS, Copland S, McNamara RM, Yellin AE, Schneider RL, Treiman RL. Factors influence ulcer healing in patients with combined arterial and venous insufficiency. J Vasc Surg. 2001;33:1158-1164.
