SPECIAL TOPICS – Part 5
Chairpersons: J. CAPRINI (USA), H. PARTSCH (Austria)
The influence of the dynamic elasticity coefficient on the
action of compression therapy
H. A. M. NEUMANN (Netherlands)
In the presented paper, the author challenged the official CEN measurement technique for prediction of the dynamic effect of different compression hosiery in the same compression class. The second conclusion was that differences in hysteresis of the hosiery can lead to differences between static and dynamic behavior of compression hosiery. Low hysteresis in the knitwear makes hosiery more effective, with greater hysteresis the hosiery is comparable to nonelastic or textile elastic bandages.
The role of compression in preventing postthrombotic
syndrome
H. PARTSCH (Austria)
Partsch studied 37 patients 2 years after DVT. Eleven had been treated by bedrest and 26 by walking with either bandages or compression stockings. There was a significant decrease in swelling measured in 10 out of 11 of patients who had been treated by bedrest, and in 15 out of 26 of patients who were treated by compression and walking. Seven of the 11 of patients in the bedrest group suffered from pain, versus 10/26 in the walking group. In conclusion, compression and walking is an active therapy to avoid postthrombotic pain swelling.
Recurrent varicose veins:
our experience with 5 – year follow-up
C. ALLEGRA, A. CARLIZZA, M. BARTOLO (Italy)
The authors shared their experience of proceeding with recurrent varicose veins. They emphasized the role of echo and color Doppler in the diagnosis of the location and the morphology of the lesion, especially in the choice of the operative technique. Over 12 years, 1326 patients underwent surgery on varicose veins.
The patients were divided into four groups, according to the location of intervention:
1. Primary great saphenous vein 65%
2. Primary small saphenous vein 10%
3. Primary associations 8%
4. Secondary varicose veins, great saphenous vein area 17%.
Overall new recurrences at 5 years were 37.7%.
Group 1. 12.6% (A1 SF junction only – 29 patients, A2 – SF junction + Hunter canal perforators – 29 patients, A3 SF junction + Hunter canal perforators + leg perforators – 51 patients)
Group 2. 29.5%
Group 3. 36%
Group 4. 65%
The authors concluded that the location of the incompetent perforator vein (above or below the knee) and previous DVT play a leading role in the occurrence of recurrent varicose veins. The second conclusion is that the consequent surgical procedure could change the number of recurrences of varicose veins in groups 3 and 4.
A combined compression system for treatment of venous leg
ulcer influence on venous hemodynamics and clinical efficacy
J. STREJCEK (Czech Republik)
The authors presented a new method of healing venous leg ulcers that they call double-step watercushion. This simple cushion made of fine, nonallergic rubber, is partially filled with water. One part of the cushion is fixed under the sole and the other in the ulcer region. During walking the water is squeezed from the peripheral part to the part placed on the ulcer. The authors verified the activation of the muscle pump by means of duplex ultrasound and photoplethysmography.
In spite of reports in the literature about the advantage of minimally invasive methods over conservative treatment, the authors expected high clinical efficacy in healing of venous leg ulcers.
AN INTERACTIVE DEBATE
Chairpersons: A. CORNU-THENARD (France), P. RAYMOND-MARTIMBEAU
(USA), J.-F. UHL (FRANCE).
Panel of experts: J. P. BENIGNI (France), J. J. BERGAN (USA),
J. CAPRINI (USA), P. COLERIDGE SMITH (UK), M. FORRESTAL (USA),
A. FRULLINI (Italy), C. GARDE (France), J. L. GILLET (France),
L GRONDIN (Canada), J. J. GUEX (France), D. HILL (Canada),
M. LEFEBVRE-VILARDEBO (France), M. PERRIN (France),
A. A. RAMELET (Switzerland), M. SCHADECK (France), F. VIN (France)
In this special interactive session several clinical cases were presented and discussed by a panel of experts. The audience had the opportunity to share their experience of different clinical therapies through an electronic voting system.
In the treatment of telangiectasia and reticular veins, there was a general consensus in the use of sclerotherapy over other methods such as lasers. When treating matting, Dr Grondin proposed the use of telangiectatic ablation with multiple needle punctures.
Regarding the medical and surgical dilemmas in the treatment of large veins, different issues were raised. The increasing use of foam sclerotherapy and of several endovenous closure devices rather than classical surgical management became obvious. These less invasive therapies allow the treatment of older people, who in the past would have been treated only by means of compression. The panellists cited ongoing studies that show excellent clinical results at 3 years with the use of foam sclerotherapy in the great saphenous vein compared with surgery.
Dr Caprini emphasised the important aspects of a correct clinical, hemodynamic, and radiological assessment when dealing with patients with edema and ulcers. Among the different treatment options, only the efficacy of compression therapy has been shown with randomized trial methodology, and is now a 1A grade level recommendation with an ulcer recurrence rate of 29% to 38%.
Dr Raymond-Martimbeau emphasized the importance of syringe aspiration before each injection, a correct choice of the dosage, and concentration of the sclerosing agent, and the use of US-guided monitoring when dealing with medium to large veins in order to avoid complications such us pigmentation and skin necrosis. She presented a case of severe pigmentation that occurred 7 years earlier, and reported how the appearance improved using a liposuction aspiration tissue technique.
Chairpersons: A. FRONEK (USA) A. NICOLAIDES (Cyprus)
Rollercoaster reflux: definition and clinical significance
W. S. GRADMAN (USA)
Using ultrasound methods, namely Duplex scanning, it is possible to easily identify reflux pathways that typically descend from a leaking point to a varicose vein.
At the same time, it is possible to identify subjects in whom the reflux originates at a lower point, ascends 10 or even 20 centimetres, and then descends again, with a pattern that has been described by previous authors as paradoxical flow, but that can be graphically described as a “rollercoaster reflux.” Duplex scanning is able to identify the exact origin of the reflux, and direct digital compression is able to abolish the filling of the varicose vein.
In 11 patients with this kind of reflux, the source of reflux was the femoral vein in three cases, the popliteal vein in two, the great saphenous in three, the small saphenous in two, and the tibial veins in one case.
The affected veins were the great saphenous in three cases, the Giacomini vein in two cases, and in six cases collateral veins were involved.
Being able to recognize this kind of reflux makes it possible to correct it surgically, with good clinical results.
Factor XIII-mediated inhibition of fibrinolysis accelerates
healing of venous leg ulcers
Y. HEROUY (Germany)
Factor XIII has been used topically to treat venous leg ulcers using the rationale that ulcers have a high fibrinolytic activity, and that subjects with factor XIII deficiency have difficulties in healing wounds.
Twenty patients were examined with Duplex to confirm the diagnosis, and 10 were treated with Factor XIII, while 10 received a placebo treatment. All the patients received conventional compression therapy.
The ulcer area was assessed using a computerized system that allows measurement the ulcer area expressed as number of pixels.
The subjects had punch biopsy before and after the topical treatment.
The fibrinolytic activity was increased in the placebo group and had no variation with treatment, while the patients that received topical Factor XIII showed a significant decrease. At the same time, ulcer healing was accelerated, and the ulcer area was decreased after the first week of treatment.
The author suggests that Factor XIII is an effective antifibrinolytic drug that used topically can accelerate venous leg ulcer healing.
Elastic compression stockings in the prevention of
the post-thrombotic syndrome after deep vein thrombosis:
a meta-analysis
D. N. KOLBACH (Netherlands)
Compression therapy is traditionally used in treating patients with deep vein thrombosis, but the evidence that this treatment reduces the occurrence of post-thrombotic syndrome has rarely been assessed.
The authors did a search of Medline, EMBASE, Cochrane controlled trials register, and used hand searching and personal communications, to look for confirmed deep vein thrombosis and nonpharmaceutical interventions.
Three randomized controlled trials were identified, two of them comparing elastic stockings with a compression of 30 to 40 mm Hg at the ankle against no intervention, after deep vein thrombosis, while the third study used stockings with 20 to 30 mm Hg compression, and stockings one or two size larger, as placebo.
In the treatment group only 32% developed postthrombotic syndrome, compared with 62% in the control group, with an odds ratio of 0.32, while considering only severe post-thrombotic syndrome the odds ratio was 0.39, favoring treatment.
No serious side effects were mentioned.
There is evidence enough to suggest that elastic compression stockings should be systematically added to the treatment of deep vein thrombosis, to prevent post-thrombotic syndrome.
It remains unclear when to prescribe the stockings, for how long, and what the effect is of different compression classes.
Changes of venous valvular function in patients with chronic
venous disease undergoing heat stress
T. OGAWA (Japan)
The authors studied 25 subjects with chronic venous disease, using a Duplex scanner to measure vein diameter, peak reflux velocity, reflux time and volume, after 5 minutes in a cold bath at 15° and then after 5 minutes in a bath at 40°.
The common and superficial femoral veins were studied, together with the great saphenous vein. Eight refluxes appeared after the hot bath, two in the superficial system, and six in the deep veins, and vein diameter increased in all cases. The authors conclude that heat stress deteriorates venous function.
This observation could have practical applications considering that patients are studied at different times of the year, and under different temperature conditions.
Corona phlebectatica:
clinical and hemodynamic significance
J. F. UHL (France)
Corona phlebectatica, also called malleolar or ankle flare, is defined as fan-shaped intradermal telangectases on the medial or lateral aspect of the foot.
In the CEAP classification, it is part of the C1 class definition, but there is controversy on the importance of this finding as a prognostic tool.
Using classification software, called CVR, the authors studied 347 patients, and found that ankle flare was present in 27.5%, and it was graded as severe in 13, moderate in 25, and mild in 54.
It seems to be correlated with the severity of the disease, and particularly with reflux in the perforators, but it appears to occur early.
Its prognostic significance is unclear.
Longitudinal studies will be required in order to validate it as a valuable tool for the clinical prediction of the development of severe chronic venous disease.
Efficacy of a short-stretch tubular compression orthosis
compared with a short-stretch bandage in the treatment of
venous leg ulcers
M. JUENGER (Germany)
The treatment of venous leg ulcers is based on local compression.
It is usually accomplished using short-stretch bandages, that have the disadvantage of tending to slip and lose shape; above all their efficacy is highly dependent on the skill of the fitter.
Using a new short-stretch tubular compression orthosis, Tubulcus, that exerts a 30 to 40 mm Hg pressure at the ankle level, appropriate pressure is applied, independently the skill of the fitter.
One hundred and eighty-eight patients suffering from ulcers not older than 3 months with a maximum diameter of 5 cm were studied in 32 centers for 12 weeks. Half were treated with the new orthosis, and half with a short stretch bandage applied by experienced personnel.
The study showed that there was no significant difference between the two groups, and that a commercial compression device can compare favorably with an expertly applied elastic bandage.
The side effects mainly consisted of discomfort, and a choice of size well-suited to the patient is indispensable.
The effects of elastic stockings on venous hemodynamics
M. M. FIGUEIREDO (Brazil)
While compression stockings are an evidencebased therapy for chronic venous disease, it is not so easy to quantify the effects they exert.
The use of an air plethysmograph allowed the author to study 29 limbs of 17 patients, in CEAP classes 4 and 5, before, during, and immediately after wearing compression stockings.
The venous reflux was reduced with the stockings, as expressed by a reduction in venous filling index, and the venous volume was reduced too, but the calf muscle pump function was only slightly affected, and the ejection fraction and residual volume fraction were virtually unaffected.
As soon as the stocking is removed, the beneficial effects are no longer exerted, and the plethysmographic parameters return to their initial value.
Placebo compression stockings: myth or reality?
H. PARTSCH (Austria)
In assessing the efficacy of compression stockings, some studies use stockings one or two size larger, as placebo.
These stockings are supposed to be devoid of active properties, but using special equipment to measure the pressure under the stockings, it was found that stockings two sizes too large, as compared with almost 35 mm Hg exerted by fitting II class stockings, exert a pressure of slightly more than 5 mm Hg. Studying 20 volunteers with venous occlusion magnetic field plethysmography it was found that a very mild (5 mm Hg) pressure is able to increase venous outflow (nonsignificant), to reduce swelling (nonsignificant), and to increase tissue compliance (P >0.001).
So some effects can be expected, as long as the stockings do not slip down, and real placebo compression does not exist.
Chairpersons: N. MORISSON (USA), H.A.M. NEUMANN (Netherlands)
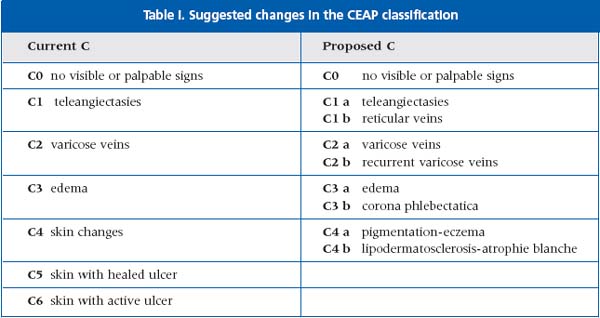
CEAP revised classification
A. CORNU-THENARD (France)
The current C covers all the aspects of the classification, and moreover the external consistency is good, so why create a new classification?
After the UIP in Rome, other definitions and refinements were suggested.
C 4, skin changes, covers pigmentation, eczema, lipodermatosclerosis, atrophie blanche, and as lipodermatosclerosis and atrophie blanche are more closely related to the pre-existence of an ulcer, C4 a and C4 b were created.
The same pathway was followed for corona phlebectatica, known from the Widmer Classification. Corona is a sign of chronic venous insufficiency over a long period and the prevalence of corona is related to edema, so C3 a and C3 b were created.
We need a computerized venous registry to evaluate the need for a new classification.
Changes in endothelial activity caused by
venoactive drugs measured by photoplethysmography and
circulating endothelial cells
J. STREJCEK (Czech Republic)
Impairment of endothelial activity is one of the early signs of vascular disease development. Changes in endothelial activity are also present in chronic venous insufficiency. These changes can be detected by several methods. In this paper photoplethysmography and counting of circulating endothelial cells in veins was used.
It is presumed that a venoactive drug stabilizes the endothelial cells in the veins and causes an increase in their activity.
In a group of 37 patients with chronic venous insufficiency (CEAP 3-4) the authors measured:
– number of circulating endothelial cells
– number of circulating endothelial cells after venous stress (leg occlusion)
– changes in endothelial activity after acetylcholine iontophoresis
After 2 months of venoactive drug (troxerutinum 300 mg, heptaminol 300 mg, extract of ginkgobiloba, twice a day) the results were compared with those obtained before treatment and in a group of untreated volunteers in CEAP 3-4.:
– increase in endothelial stability as a statistically significant lower number of
– circulating endothelial cells after 2 months of treatment
– increase in endothelial activity measured by photoplethysmography after acetylcholine iontophoresis
These results demonstrate, by two independent methods, an increase in endothelial stability after 2 months of medication with a combination of venoactive drugs.
Primary sclerotherapy registry and trial; the sclero 10-year,
randomized CVI study
G. BELCARO (Italy)
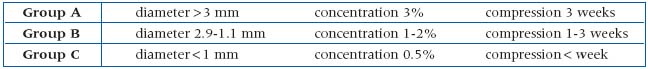
This study compared two sclerosing agents, sodium tretradecyl sulfate and athoxy-sclerol. A comparable group of patients aged 25 to 65 with uncomplicated chronic venous insufficiency and varicose veins were included.
Patients were divided into three groups according to the vein diameters, and the concentration of sclerosing agent and duration of compression was indicated.
Three-month and 6-month vein closure, skin reactions, systemic reactions, local inflammation, pain, target vein trombosis, tolerability, and main trunk 5-and 10-year closure were investigated. They were all significantly in favour of A ethoxy-sclerol.
Ultrasound features of sciatic nerve varices
S. RICCI (Italy)
Sciatic nerve varices are believed to be a rare clinical finding. Patients present with a symptomatology of sciatic pain because the vein follows the fibular saphenous nerve, its mother branch, the common fibular nerve at the popliteal site and the great sciatic nerve in the thigh.
On clinical exanination one sees typical small or large varicose veins on the anteroposterior part of the leg (appearing just below the popliteal crease and extending lateral to the small saphenous vein), and a painful point can be found at the site of the “vein disappearance” below the popliteal crease.
Clinical diagnosis must be confirmed by color duplex: this shows a superficial varicose vein lateral to the small saphenous vein, becoming subfascial at the popliteal crease for a short distance and progressively getting deeper in the thigh muscular spaces. The vein described follows the fibular saphenous nerve.
One patient was treated with foam sclerotherapy, with a good clinical result at 1-month follow-up examination.
Another patient was treated the same way by another specialist, and this resulted in an irreversible nervus fibularis palsy.
Efficiency in the treatment of perforating veins in
combination of transilluminated miniphlebectomy and
preoperative duplex ultrasound
A. FLOR (Austria)
There are different modalities of treatment for insufficient perforant veins in cases of severe chronic venous insufficiency. SEPS requires increased technical requirements which are costly, and phlebectomy is sometimes inappropriate because one cannot determine the exact localization where the vein perforates the fascia. A cheap and effective method has been proposed by the author.
He starts with a preoperative mapping of the perforating veins by duplex ultrasound.
Peroperatively, a luminiferous 5- mm rod which features at its oblique tip a cannular opening to allow the flow of saline or tumescent solution is inserted into the subcutaneous tissue. After hydrodissection, the xenon light emerging from the rod provides excellent visualization of the suprafascial perforating veins. The perforating veins are then retrieved by means of the hook through microincisions above the place of fascial perforation.
In this way, unnecessary manipulation and the total amount of stich incisions can be reduced in a diseased skin region.
Popliteal vein entrapment as a cause of multiple recurrences
of small saphenous vein insufficiency
R. MILLERET (France)
The study included 8 patients with recurrences of small saphenous vein insufficiency who had been operated on twice or more.
Symptomatology: leg pain when standing and walking, swelling of the leg in the early morning, tension of the calf.
Clinical findings: unequal in calf diameter, swelling of the calf during exercise, rarely disappearance of posterior tibial artery pulse during plantar flexion.
Diagnosis: duplex scanning, confirmed by dynamic ascending phlebography which shows compression of the deep veins at the popliteal level during active plantar flexion of the foot.
Treatment: surgery is only performed in cases of positive dynamic phlebography. Under general anesthesia, the popliteal fossa is explored through an incision after M. Perrin (longitudinal incision of the skin, vertical incision of the fascia). The popliteal vein is dissected free with section of any fibrous element that mighty compress the vessel. After removal of the varicose recurrences, the vena poplitea is closed with a Teflon patch.
Results: No complications occurred and the patients were relieved of symptoms, calf diameter decreased, and there was no recurrence after a mean period of 18 months.
Chairpersons: A. FRONEK (USA), M. SCHADECK (France)
Venous hemodynamic mapping (VHM):
terminology and symbolism
S. MANDOLESI (Italy)
Concepts and terminology related to venous hemodynamic surgery have been in constant evolution since its initial description in 1988. There are several institutions worldwide performing this type of surgery for the treatment of varicose veins, and the authors presented the most recent and widely accepted terminology used in this surgical strategy. The main purpose of this classification is to divide the veins of the lower extremities into four systems:
1. R1: all the veins inside the deep fascia
2. R2: all the veins between the superficial and deep fascia (greater and lesser saphenous veins, Giacomini and anterior saphenous vein)
3. R3: all the veins in the subcutaneous tissue
4. R4: those veins in the R3 system connecting two R2.
With this type of division different types of venovenous shunts between these systems are described, and a surgical strategy can be developed and drawn in a diagram (Figure 1).
In our view this is a very practical way of approaching varicose disease with an echoguided surgical strategy, directed to the identification of the refluxing points, and the elimination of shunts. Further worldwide consensus and discussion on this matter is important, as well as future results of several prospective studies that are under way.
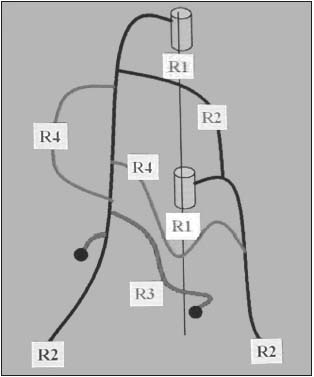
Figure 1. Division of veins of the lower extremities.
Venous hypertension, inflammation, and valve remodeling
M. N. PASCARELLA, (USA)
Blood flow is directly related to the pressure in blood vessels, as was demonstrated by Poisseuille in 1884. Different blood flow patterns (laminar vs turbulence), change the shear stress which in turn regulates physiological vascular responses. Turbulent flow has been found to be capable of triggering an inflammatory reaction through leukocyte activation and transmigration into the vascular wall.1 The authors presented very interesting work, with the objectives of defining the key elements of venous inflammation in its early stages, and also defining the anti-inflammatory effects of micronized purified flavonoid fraction (MPFF) (MPFF at a dose of 500 mg, Servier, France). For this purpose they created a model of venous hypertension in mice performing an AV fistula in the right groin, with ligation of the epigastric vein and the femoral vein above the fistula (
The study design included 35 animals separated in these groups:
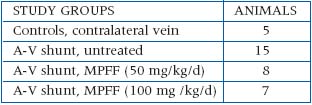
The authors studied the leukocyte infiltration (Figure 2), adhesion molecule expression (Figure 3), apoptotic markers, transcription factors, and preformed intravital microscopy of gracilis muscle microcirculation.
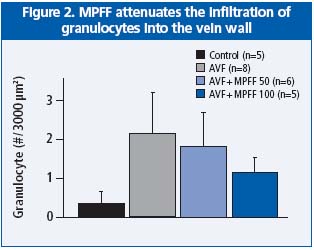
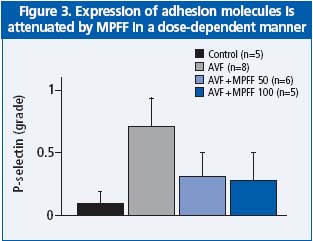
Several interesting conclusions are obtained from this new model of venous hypertension:
1. In this model of leukocyte infiltration, adhesion molecule expression and apoptosis of endothelial cells, the hallmarks of inflammation, are seen.
2. Veins subjected to AV fistula pressure show lesions mimicking the findings in human surgical specimens
3. MPFF attenuates the inflammatory process in a dose-dependent manner. References:
Combined endovenous laser and duplex – guided foam
sclerotherapy in the treatment of varicose veins
M. N. ISAACS (USA)
With the objective of reducing the incidence of varicose veins collaterals that can be present after treatments of greater or lesser saphenous veins trunks with laser therapy, the authors proposed a method of combined laser and duplex-guided foam sclerotherapy of open distal segments and abnormal open branches with foam sclerosing agents.
The proposed method starts with the usual procedure for endovenous laser. After placement of the laser catheter in his place, the vein distal to catheter insertion is treated with foam 3% STD, 2 to 4 cc in total, while deep vein junction is compressed. After perivenous tumescent anesthesia is administered, endovenous laser is performed as usual.
The authors presented a group of 84 veins treated without combined foam sclerotherapy and a rate of 18% persistent open segments and a short series of 17 veins in patients with the combined therapy and a 6% rate of persistent open segments.
Although the number of patients in the combined therapy group is somewhat low to draw a conclusion, from duplex-guided foam sclerotherapy complements endovenous laser in a safe way, resulting in fewer open segments requiring further treatments.
Current laser and light-based technology in the treatment
of leg veins
R. ADRIAN (USA)
The purpose of this study was to improve the understanding of the mechanism of action of different lasers are employed in the superficial treatment of small varicosities. The response to laser therapy is often seen histologically as a decrease in vessel size, intravascular coagulation, endothelial damage, and an increase in perivascular collagen (Figure 1).
Although recent advances in our understanding of pulse duration and pulse delivery have increased safety and efficacy, most practitioners are disappointed with the lack of consistent clinical improvement achievable with all these systems. Pulse dye lasers are associated with significant dermal hemorrhage, but the main problem with these systems remains the postprocedural long-term hyperpigmentation.
The speaker concluded that in his wide experience with lasers, sclerotherapy is by far the best way to treat leg vein varicosities.

Figure 1. Laser-induced changes in dermal tissue.
Telangiectases and reticular veins: how to quantify
treatment results
J. F. UHL (France)
The presence of telangiectases is often an indicator of a complex incompetent venous network beneath the skin. The recent use of transillumination has been a first step in realizing some reticular mappings. The authors presented a new system (VARITAS), based on a computerized digital imaging technology that allows a record of the precise location of the reticular and telangiectatic veins and to compare and validate the results of different treatments (Figure 1).
Pixel-counting quantitates the degree of abnormality of each lesion. A comparison of the pixel count before and after treatment quantitates efficacy of treatment and allows statistical analysis. The system is still under development and not commercially available
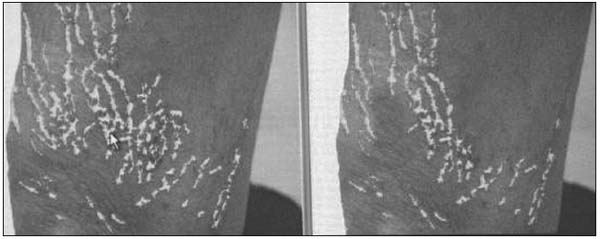
Figure 1. Computerized mapping of pre-and posttelangiectasia treatment.
Chairpersons: J. CHUNGA CHUNGA (Peru), A. J. COMEROTA (USA)
Skin manifestations of CVI
A. A.RAMELET (Switzerland)
The author presented a review of all the main skin disorders resulting from CVI. He divided them into two groups:
a) acute manifestations: purpura, contact and stasis dermatitis, infections, panniculitis, drugrelated eruptions, and necrosis
b) chronic manifestations: “dermite ocre,” teleangiectasias, pseudo-Kaposi (acroangiodermatitis), dermatitis, lymphedema, papillomatosis, liodermatosclerosis, calcifications, atrophie blanche, and leg ulcers.
It is important to realize that venous hypertension may also aggravate all types of dermatoses of the leg, such as psoriasis or lichen rubber planus on one hand, and can induce hyperhidrosis or diminution of follicular features on the other. In the short discussion that followed, some of the audience suggested that CVI can lead to many types of skin inflammatory disorders. The conclusion of the presentation was that CVI includes numerous skin manifestations, and it would be an advantage for specialists in phlebology also have experience in dermatology.
Incompetent perforating veins of the foot
I. UCHINO (USA)
This short presentation discussed incompetent perforating veins of the foot. Similarly to other areas, valvular insufficiency was considered to be present when venous reflux was over 0.5 seconds. About 90% of these veins are localized in four anatomical regions of the foot: near the lateral and medial malleolus and the lateral and medial sole of midfoot.
Localized varicose veins, clusters of spider veins, skin pigmentation, and ulcers are the typical signs of these disorders.
Investigation was performed in a small group of patients with typical signs of perforating veins insufficiency of this area using continuous wave Doppler ultrasound and color-flow duplex imaging. The results were very interesting:
• 88% of incompetent perforating veins were found in typical anatomical regions
• All incompetent veins were diagnosed by continuous wave Doppler ultrasound
• Color flow duplex Doppler documented incompetent perforating veins only in 50% of the time
• Over 90% of incompetent perforating veins were associated with venous reflux of the leg.
In conclusion, the author suggests that venous reflux of the leg may be a possible etiologic factor which leads to perforating vein insufficiency in the foot region.
Venous leg ulcers and apoptosis: a TIMP 3-mediated pathway?
Y. HEROUY (Germany)
The causes of vein pathology are still unrecognized. A new method of investigation – molecular biology – may provide answers to questions on many important subjects such as apoptosis. There are several genes in human DNA which are recognized as inducers of programmed cell death. However, not only genes regulate programmed cell death. There are many intra-and extracellular factor, that can initiate this process. One of them is the tissue inhibitor of metalloproteinase -3 (TIMP-3). The prodeath domain of TIMP-3 resides in its N-terminal region, and apoptosis is induced by the activation of a signaling cascade involving caspase-8 and caspase-9.
The results of these investigations provide evidence that venous leg ulcer could be the result of an apoptotic signaling pathway which may be induced through a TIMP-3 mediated inhibition of proteinase-dependent extracellular matrix degradation. These results suggest that controlling programmed cell death may have therapeutic potential in preventing venous ulceration.
