Subdiaphragmatic venous insufficiency – Embolization treatment using mixed technique
S. ZUBICOA EZPELETA,
M. GRIMBERG,
L. VERGARA CORREA,
J. A. JIMÉNEZ GUTIÉRREZ
Madrid-Spain
SUMMARY
Results are given for treatment administered to 2491 patients with recurrent varicose veins who were cared for in our unit from 1995 to 2003: 64.44% of the recurrences were bilateral and 35.56% unilateral. The average age was 53. These patients were divided into two groups according to the material used for embolization.
The first group of 1500 patients were treated from 1995 to 1999, and 58.3% underwent selective pelvic phlebography. Of these, 80.9% underwent embolization using coils, by which 82% of insufficient venous branches were occluded. Sometimes it was impossible to occlude leakage points in small cascade vessels associated with the hypogastric vein. Additionally embolization varicose vein surgery on the lower limbs was performed in 85.4%. Seventy-six percent of these patients reported an improvement of symptoms in the pelvis and lower limbs after 6 months. The other group of 991 patients were treated from 1999 to 2003. Of these, 55.76% underwent selective pelvic phlebography. From these, 86.59% underwent embolization using a “sandwich” method with the use of coils plus foam and, of these, 83.26% underwent varicose vein surgery on the lower limbs as a complementary treatment. After 6 months, 95.61% of patients reported an improvement in pain, pelvic heaviness, and lower-limb edema.
The aim of this study was to underline the importance of pelvic reflux in the development of recurrent varicose veins and demonstrate that embolization using a sandwich technique with the use of coils plus foam provides better results.
INTRODUCTION
Chronic venous insufficiency is one of the most common chronic diseases which affects mankind. Different studies claim that 25% to 33% of women and 16% to 20% of men suffer from the disease1-3 and varicose veins recur in the lower limbs following surgery in 20% to 80% of cases. In our institution the recurrence rate is between 20% and 30%.4-6
It is essential to treat the infradiaphragmatic venous system as one functional unit, and to understand the hemodynamic behaviour of the normal centripetal venous circulation, and of the centripetal and centrifugal flow patterns in chronic venous insufficiency.7
A pressure change in this system leads to the development of pathological collateral connections which act in certain cases as leakage points with retrograde venous flow from the pelvis to the lower sectors. This may be one of the causes which gives rise to the initial onset or recurrence of varicose veins or stasis in the lower limbs.8-13
The most common therapeutic treatments for the control of pelvic leakage points are either surgical ligature or endovascular occlusion (embolization). In our opinion the benefits of embolization make this the method of choice.14-29
We have analyzed the treatment results for 2491 patients who attended our clinics and were treated for recurrence of varicose veins in the lower limbs by our unit from 1995 to 2003, and who were assumed to be suffering from pelvic disease based on clinical symptoms, physical examination, and vascular investigative tests. These patients were divided into two groups according to the material used to occlude the insufficient veins. Gianturco coils were used with the first group of patients, while a sandwich technique using coils plus 2% polidocanol or hydroxypolyethoxydodecane foam was used with the second group.
AIM
To present the results of an analysis performed on two patient groups with recurrent lower-limb varicose veins treated intraluminally by embolization: one group underwent occlusion by means of Gianturco coils, and the other group was treated using a “sandwich” method consisting of Gianturco coils and 2% polidocanol or hydroxypolyethoxydodecane foam (Figure 1).
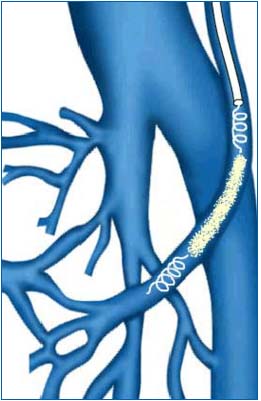
Figure 1. Mixed embolization technique (sandwich) . Coils and foam
applied alternatively.
MATERIAL AND METHODS
Study type: retrospective, selective, and descriptive, conducted from January 1995 to July 2003.
Target population: 2491 patients who attended the angiology and vascular surgery unit from 1995 to 2003 and were treated for recurrent lower-limb varicose veins for whom the clinical symptoms and results of physical examinations and vascular investigative tests suggested pelvic disease. Some of these were treated with embolization: in the first group, Gianturco coils were used for this purpose while the second group underwent a sandwich method using Gianturco coils plus 2% polidocanol or hydroxypolyethoxydodecane foam. The recurrence affected both limbs in 64.44% of patients, while 35.56% of patients developed varicose veins on one limb. The average age was 53. The youngest patient was 25 and the oldest patient was 71.
Diagnosis, treatment, and follow-up protocol:
1. Clinical history. History and physical examination. Signs and symptoms of pelvic stasis were recorded in detail, particularly pelvic pain, dyspareunia, hemorrhoids, vulvar varices, varicose veins in the lumbar region, pelvic dilated veins, atypical varicose veins in the posteroexternal region of the thigh, etc.30-33
2. Noninvasive and invasive vascular laboratory examination by means of: photoplethysmography and colour ultrasound imaging of the lower limbs.18-34,35 When previous clinical symptoms and examinations were positive for pelvic disease, color ultrasound imaging of this sector was requested (transparietal and transvaginal).36-38 For results to be positive, the following had to be present: gonadal axes measuring more than 8 mm in diameter, pelvic venous lakes, dilation of hypogastric axes, compression and malformation of the iliocaval sector. These signs were considered to be indications for selective pelvic phlebography.
3. Selective pelvic phlebography was used to evaluate the morphology of gonadal axes, the presence of pelvic venous lakes, hypogastric axes, compressions and malformations of the iliocaval sector, whether the direction of flow was centripetal or centrifugal from a hemodynamic view point, development of homo- and contralateral collateral circulation, and leakage points to anterior or posterior regions of the deep or superficial venous system of the lower limbs. The study was performed in an angiography room, with the patient standing on both feet on a tilting table angled at 60º. The examination began with cannulation (Seldinger’s method) of a vein in the elbow flexure (Figure 2). This was generally the right basilic vein, though some were cannulated through the right femoral vein due to anatomical variations (Figure 3). Under fluoroscopic control, a 5F guide 55 cm long was inserted until reaching the vicinity of the right auricle or inferior cava. Afterwards, a 5F multipurpose catheter 125 cm in length was introduced and the cannula was inserted with the aid of a Terumo guide in the opposite direction to the venous flow, being careful not to damage any valves en route. The hypogastric and gonadal veins were selectively cannulated (Figure 4), a nonionic contrast medium was injected manually (average of 89 cc per examination), and the patient was asked to perform the Valsalva maneuver. Throughout the procedure, the patient was fitted with a bladder drain to prevent the bladder filling with the contrast medium and thus making imaging of the intrapelvic venous pedicles more difficult.

Figure 2. Guide and catheter in elbow flexure for study and
embolizing treatment of pelvic escape points.

Figure 3. Catheterization through the right femoral vein. Venous
lakes associated with the left gonadal vein.
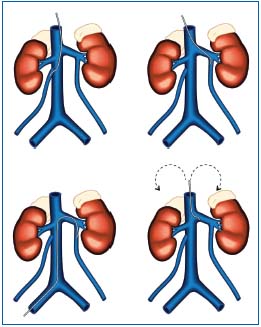
Figure 4. Drawings showing selective catheterization of the gonadal
veins from the basilic and femoral vein.
4. Embolization, if indicated as a complement to pelvic phlebography, was performed by selective occlusion of the affected venous axes. In the first group of patients, Gianturco coils measuring 5, 10, and 15 cm in length and 10 mm in diameter were used for occlusion. In the second group, embolization was performed via a sandwich method using alternatively coils with the same specifications as the previous ones plus 2% polidocanol or hydroxypolyethoxydodecane whipped as foam (Figures 5,6).

Figure 5. Mixing device with needle for foam production.

Figure 6. Hydroxypolyethoxydodecane foam being mixed and
aspirated in a syringe for perfusion through the catheter.
5. Complementary treatment of recurrent varicose veins in the lower limbs by means of surgery and sclerotherapy.
6. Short-, medium-, and long-term follow-up included evaluation of the condition of the superficial and venous system of the lower limbs and pelvis by means of a physical examination and color ultrasound after 30, 60, 90, 180, and 360 days and then each year.
RESULTS
(Table I)
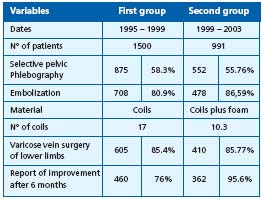
Table I. Summary of results
The first group consisted of 1500 patients treated between January 1995 and April 1999. Eighty hundred and seventy-five (58.3%) patients underwent selective pelvic phlebography of which 708 (80.9%) were embolized. These patients were implanted with Gianturco coils of various thickness and gauges and insufficient venous branches were occluded in 82% of cases.
Sometimes it was impossible to occlude leakage points in small cascade vessels associated with the hypogastric vein. Varicose surgery of the lower limbs was performed complementary to embolization in 605 (85.4%) of patients.
On these patients’ follow-up, it was found that after 6 months 76% of patients reported an improvement in the following symptoms: pain and heaviness of the pelvis and lower limbs, an improvement in sexual intercourse and menstrual periods. The relatively low success rate was attributed to the impossibility of approaching certain axes. Each patient required ± 17 coils, which makes the procedure very costly compared with others.
The other group consisted of 991 patients (1982 limbs) treated between May 1999 and July 2003. Of these, 552 (1104 limbs) (990/552; 55.76%) underwent selective pelvic phlebography. Of these, 478 were embolized (956 limbs) (552/478; 86.59%) and, of these, 410 (478/410; 85.77%) underwent additional surgery of lower limbs varicose veins after embolization (Figure 7).
When selective pelvic phlebography was performed in 552 patients, 310 patients (552/310, 56.16%) displayed 1 or 2 dilated avalvular gonadal vessels (Figure 8) measuring more than 8 mm in diameter. 446 (552/446; 80.8%) patients presented significant venous lakes or pelvic varices, while 530 (552/530; 96.01%) patients displayed leakage points from the hypogastric vein to the lower limbs. Escape routes showed as follows: to the great saphenous vein or its tributaries in 66 patients (66/530; 12.45%); to the deep venous system, deep femoral veins in 84 patients (84/530; 15.85%) and to the residual embryonic sciatic veins (Figure 9) in 38 patients (38/530; 7.17%). A high number of patients, 342 (342/530; 64.53%) displayed mixed reflux in both superficial and deep venous systems (Figure 10).

Figure 7. Distal catheterisation of the right gonadal vein during
mixed embolization (sandwich technique). Coils visible in the path
of the previously embolized left gonadal vein.

Figure 8. Severe periuterine pelvic varicose veins leading from the
left gonadal vein. Coils in the path of the right gonadal vein. Mixed
embolization. Sandwich technique.

Figure 9. Pelvic escape points from the right gluteal vein to the sciatic
veins.

Figure 10. Periuterine pelvic varicose veins associated with the right
gonadal vein. Coils in the path of the left gonadal vein. Mixed
embolization. Sandwich technique.
Of the 552 patients who underwent selective pelvic phlebography, 478 were embolized (86.59%) with the following notes: 34 patients (7.11%) had previously undergone a hysterectomy which meant that the gonadal veins were not evaluated, embolization of the right gonadal vein was not completed in 2 (0.42%) patients due to technical problems (cannulation difficulty) and the normal gonadal areas displayed a reflux route only to the hypogastric area in one patient (0.21%). For the remaining 438 patients (91.63%) embolization was bilateral, 810 gonadal axes were occluded, and there were 872 leakage points to the lower limbs. The sealed vessels, in order of frequency, were the left gonadal vein and the pudendal hypogastric branches, the inferior gluteus, and the obturator vein.
The coils most commonly used in both axes were 5, 10, and 15 cm, placed beginning with the longest. An average of 10.3 coils were used per patient. Procedure duration was 30 to 40 minutes.
Seventy-four (13.41%) patients were excluded, 6 (1.09%) due to iliac posthrombotic syndrome, 22 (3.99%) due to pelvic venous compression syndrome; 10 (1.81%) due to venous malformations (agenesis of the vena cava, double inferior vena cava etc.) 36 (6.52%) due to the impossibility of identifying veins for embolization.
Complications arising during the procedure were never significant. Some were inherent to the percutaneous method itself: (1.45%) 8 patients showed a slight hematoma at the puncture site, (1.09%) 6 patients displayed minor mechanical phlebitis symptoms, and (0.54%) 3 patients extravasation of the contrast medium. Since the embolizing treatment is designed to achieve controlled thrombosis of the pelvic venous axes, symptoms noted following the technique were those typical of venous thrombosis. We described these as postembolization syndrome in previous studies, and the symptoms and signs disappeared within 1 week of treatment.
This group displayed the following postembolization syndrome symptoms: 258 (46.74%) radiating pain, particularly in the gluteal region, and sciatic-like pain in the posterior surface of the lower limbs radiating in fewer cases to the hypogastric and lumbar region: 122 (22.1%) general malaise with headache; 49 (8.88%) a fever of ~38º C – and 23 (4.17%) superficial phlebitis.
The follow-up data refer to the 410 patients who underwent embolization and then varicose vein surgery of the lower limbs after the procedure. A 6-month follow-up revealed that 95.61% (410/392 of patients) reported an improvement in pain, pelvic heaviness and lower-limb edema.
CONCLUSIONS
Our results suggest that the subdiaphragmatic venous system made up of the pelvic and lower-limb veins should be treated as one functional unit. This approach helps to explain the appearance of varicose veins, and stasis and recurrence following surgery. Many normal communication routes are present between the venous systems which make up the subdiaphragmatic venous system, but pathological communications may appear in response to pressure changes which determine changes in blood flow direction and magnitude.
Selective occlusion of insufficient veins with embolization by means of coils plus foam achieved very satisfactory results for the patients in terms of alleviation of clinical symptoms, reduction of pain in the lower limbs and pelvis, edema, pelvic heaviness, and complaints during sexual intercourse. We believe that in cases of pelvic varicose veins with centrifugal collateral circulation without any other morphological changes, embolization using Gianturco coils and 2% polidocanol or hydroxypolyethoxydodecane (foam) is very effective because it allows closure of the small vessels which act as leakage points from the pelvis to the lower limbs.
This method allows us to reach more distal sectors where surgical access is very difficult and may be associated with severe complications.
Embolization using Gianturco coils and 2% polidocanol or hydroxypolyethoxydodecane (foam) has allowed more conclusive treatment and a reduction in the number of recurrences.
In our experience, the embolization technique is simple, can be performed on an outpatient basis, and is well tolerated in most patients. We did not encounter severe complications related to this management. Significant costs currently incur due to the number of coils used.
Two percent polidocanol or hydroxypolyethoxydodecane foam obtained by whipping the sclerosing substance increases its volume up to 300%. Its use allows the number of coils to be reduced and consequently the cost of the procedure.
Embolization is a minimally invasive method and did not lead to significant complications in our hands.
Our results obtained following clinical examination and venous laboratory examination fully support the existence of a functional infradiaphragmatic unit.
We treated the centrifugal leakage points because other collateral connections may supplement the distal to proximal circulation.
We achieved better hemodynamic and clinical results through embolization via occlusion of cascade leakage points using a mixed method.
In hemodynamic terms, the subdiaphragmatic venous system behaves as one functional unit. It includes different areas which intercommunicate in the form of a network, and the connections may be physiological or pathological depending on flow direction and magnitude (centrifugal or centripetal) in response to changes in venous pressure or anatomical dysfunction.
REFERENCES
2. Abenhaim L, Kurz X. the Veines Study (Venous Insufficiency Epidemiologic and Economic Study). An international cohort study on Chronic Venous Disorders of the legs. Angiology. 1997;48:59-65.
3. Wienert V. The epidemiology and socioeconomics of venous disorders in Germany. Phlebologie. 1993;46:225-233.
4. Perrin M, Guex JJ, Ruckley CV, De Palma RG, et al. Recurrent varices after surgery (REVAS), a consensus document. REVAS Cardiovas Surg. 2000; 8:233-245.
5. Perrin M, Bayon JM, Hiltbrand B. Nicolini P. Deep venous insufficiency and recurrent varicose vein after surgery of superficial venous insufficiency. J Mal Vasc. 1997;22:343-347.
6. Perrin M, Gobin JP, Nicolini P. Recurrent varicose veins in the groin after surgery. J Mal Vasc. 1997;22:303-312.
7. Leal Monedero J, Zubicoa Ezpeleta S, et al. Insuficiencia venosa crónica: definición, fisiopatología y clasificación. Phlebology Digest. 1996;1:4-8.
8. Perrin M. The contribution of Doppler echography in the diagnosis and therapeutic plan in chronic venous insufficiency surgery.
9. Norgren L. Various aspects of phlebology in Sweden. Phlebologie. 1997;45:444-446.
10. Hobbs JT. Pelvic congestion syndrome. Br J Hosp Med. 1990;43:200-206.
11. Gottlob R, May R. Venous Valves. Vienna: Springer-Verlag; 1986;159-174.
12. Le Page PA, Villavicencio JL, Gómez ER, Sheridan MN, Rich NM. The valvular anatomy of the iliac venous system and its clinical implications. J Vasc Surg. 1991;14:678-683.
13. Del Portillo L. Epidemiología y fisiopatología del varicocele. III Congreso nacional Andrología. Asesa, Zaragoza, España, 1987;3-12.
14. Leal Monedero J, Zubicoa Ezpeleta S, et al. Insuficiencia venosa crónica de la pelvis y de los miembros inferiores. Madrid: Mosby/Doyma Libros; 1997:61-74.
15. Tulloch WS. Consideration of sterility. Subfertility in the male. Edinburgh Med J. 1952;59:29-36.
16. Amelar RD, Dubin L. Therapeutic implications of left, right and bilateral varicocelectomy. Urology. 1987;30:53-59.
17. Leal Monedero J, Zubicoa Ezpeleta S, et al. Alternativas terapéuticas del varicocele. Paper presented at VII Congreso de Andrología, Bilbao, España, 1995.
18. Leal Monedero J, Zubicoa Ezpeleta S, et al. La exploración no invasiva en la insuficiencia venosa crónica. In Leal J, ed. Insuficiencia venosa crónica de la pelvis y de los miembros inferiores. Madrid: Mosby/Doyma Libros; 1997:61-74.
19. Shafik A, Mohi-el-Din M. Pelvic organ venous communications. Anatomy and role in urogenital diseases; a new technique of cystovaginohysterography. Am J Obstet Gynecol. 1988;159:347-351.
20. Wheatley JK, Bergman WA, Green B, Walther M. Transvenous occlusion of clinical and subclinical varicoceles. Fertility Sterility. 1991;37:362-365.
21. Herman RJ, Neiman HL, Yao JST. Descending venography: a method of evaluating lower extremity venous valvular function. Radiology. 1980;137:63.
22. Kistner RL, Ferris EB, Randhawa G. A method of performing descending venography. J Vasc Surg. 1986;4:464.
23. Leal Monedero J, Zubicoa Ezpeleta S, et al. Métodos invasivos en el diagnóstico de la insuficiencia venosa crónica: radiología pélvica y de miembros inferiores. In: Leal J, ed. Insuficiencia venosa crónica de la pelvis y de los miembros inferiores. Madrid: Mosby/Doyma Libros; 1997:75-88
24. Lechter A, Alvarez A. Pelvic varices and gonadal veins. In Negus D, Jantet G, eds. Phlebology. 1985. London: John Libbey; 1986:225-228.
25. Langeron P. Stase veineuse pelvienne, varicoceles pelviens: problèmes hémodynamiques, pathogéniques et cliniques. Phlébologie. 2000;53:155-160.
26. Lechter A. Pelvic varices: Treatment. J Cardiovasc Surg. 1985;26:111.
27. Leal Monedero J, Zubicoa Ezpeleta S, et al. Embolización en el varicocele pélvico. In Leal J, ed. Insuficiencia venosa crónica de la pelvis y de los miembros inferiores. Madrid: Mosby/Doyma Libros; 1997:115- 128.
28. Boosmsma JHB, Potocky V, Kievit CEL, Verhulsdonck JCJ. Phlebography and embolization in women with pelvic vein insufficiency. Medicamundi. 1998;42:22-29.
29. Leal Monedero J. La pathologie veineuse pelvienne. Traitement embolisant. Phlébologie. 1999;52:299-309.
30. Hargrave TB, Liakatas J. Physical examination for varicocele. Br J Urol. 1991;67:28.
31. Bassi G. Les varices des membres inferieurs. 10 ed. Edition Doin; 1967.
32. Lechter A, López G, Martínez C, Camacho J. Anatomy of the gonadal veins: a reappraisal. Surgery. 1991;109:735-739.
33. Beebe HG, Bergan JJ, Bergqvist D, et al. Classification and grading of chronic venous disease in the lower limbs. A consensus statement. Eur J Vasc Endovasc Surg. 1996;12:487-491; discussion 491-492.
34. Nicolaides AN, Miles C. Photoplethysmography in the assessment of venous insufficiency. J Vasc Surg. 1987;5:405-412.
35. Cavezzi A. Long saphenous vein and perforating veins haemodynamics: new echo colour Doppler patterns Abstracts of XIII World Congress of Phebology. Sydney 1998:109.
36. Perrin M. The contribution of Doppler echography in the diagnosis and therapeutic plan in chronic venous insufficiency surgery. Phlebologie. 1993;46:655-662.
37. Selfa S, Diago T, Ricart M, Chulía R, Martín F. Insuficiencia venosa crónica primaria de los miembros inferiores. Valoración prequirúrgica con Ecodoppler color. Radiología. 2000;42:343-348.
38. Nicolaides AN, Zukowski A, Lewis R, Kyprianou P, Malouf GM. Venous pressure measurements in venous problems. In: Bergan JJ, Yao JST, eds. Surgery of the Veins. Orlando, Fl: Grune & Stratton; 1985:111-118.
