Subjective venous symptoms: review and presentation of a pilot study
Eva HAAS2
Dep. Dermatology
Leipzig, Germany
2. Laufen, Germany
SUMMARY
In phlebology practice, the symptoms of heavy legs, feeling of swelling, fatigue, and the sensation of tension in the leg (heavy leg syndrome) are often found without an organic cause. These patients frequently suffer from psychic disturbances accompanied by a reduced quality of life. The discrepancy between symptoms and lack of objective findings leads to an ineffective therapy.
In this article we discuss the problem of leg symptoms without varicose veins and present a survey of heavy leg syndrome and quality of life in phlebology practice.
The feeling of heavy, tired, and occasionally swollen legs, particularly in the ankle region, is frequently a symptom of a chronic venous disease.1,2 In some patients, however, intensive clinical and instrumental diagnosis (color-coded duplex ultrasonography, photoplethysmography, and venous occlusion plethysmography) reveals neither a venous or arterial nor a lymphological underlying disease. For the patients themselves, however, these complaints often represent a substantial impairment of their general health and quality of life. The disparity between the paucity of objective findings and severe subjective symptoms has resulted in several different names for the disorder:
• hypotonic phlebopathy,
• varicose symptoms without varices,
• functional phlebopathy,
• heavy leg syndrome.
In this article we refer to the disorder as heavy leg syndrome. The discrepancy between the symptoms and the findings is hardly ever taken seriously from the therapeutic viewpoint and has received little scientific attention. Patients with symptoms but no objective findings are therefore often ignored. This review attempts to show the problem of alleged venous symptoms and, with the aid of a pilot study, to present the actual possibilities for measuring quality of life in people with heavy leg syndrome.
HISTORICAL BACKGROUND
Venous symptoms without varicosis were postulated as an independent clinical picture as long ago as the 1970s by Bassi,3 who proposed the term functional phlebopathy. Andreozzi et al4 described a syndrome consisting of heavy legs in an upright position, restless legs, and “evening edema” as hypotonic phlebopathy, and showed its prevalence in the Sicilian population to be 15%. The syndrome affected women twice as often as men. The main symptom was “heavy leg”. Cloarec et al5 likewise reported a prevalence of 15% for the aforementioned functional complaints. According to the Bonn Vein Study,2 half of the 3072 subjects reported leg problems, the predominant ones being a feeling of heaviness, tension, and swelling, and pain after prolonged standing. The sex distribution is interesting, however. Sixty-two percent of the women and 49% of the men reported leg symptoms in the last four weeks. However, only 1 man in 6 and 1 woman in 5 had signs of a chronic venous disorder. The Basle Study6 carried out in workers from the pharmaceutical industry likewise showed that symptoms such as a feeling of swelling and tension, tiredness, and cramps have very low sensitivity and specificity in regard to venous diseases. Leg problems are a common symptom, with numerous possible differential diagnoses (Table I). Heavy leg syndrome should be an exclusion diagnosis.7
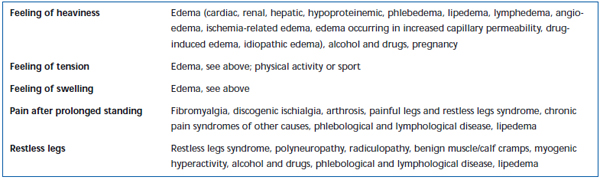
Table I. Alleged venous symptoms and common differential diagnoses.
CAUSES
The pathophysiological cause of heavy leg syndrome is unclear. It is assumed that venous hypotonia develops due to structural changes in the connective tissue8 and smooth muscle cells9 of the venous wall and to orthostatic loading of the lower extremity as a result of an upright gait. Increased capillary permeability and a change in the renin-angiotensin-aldosterone mechanism10 may also lead to heavy leg syndrome. The continuous communication between the brain and the peripheral organs is effected via various nerve and hormone signals. Under conditions of acute or chronic loading, the body uses this communication to initiate appropriate adaptive reactions. Altered adaptive reactions are also described as a cause of heavy leg syndrome in the area of psychosomatic medicine. Depressive states, anxiety states, and hypochondriac states have thus been observed in women with alleged venous leg symptoms.11
Blättler et al12 recorded psychological interviews, all of them with patients with alleged venous symptoms, in phlebology practice. The authors highlighted five principal symptoms:
• being unable to walk away,
• inability to take a step that has long been needed,
• inability to acknowledge the sex-specific attributes of the legs,
• alleged venous symptoms in the presence of a frustrated need for affection,
• obsessive personality with excessive dependence on the opinions of others.
The symptoms are evaluated as representing a conversion neurosis with projection of neurotic conflicts onto the legs.
TREATMENT
One therapeutic approach—though not one that has been confirmed by randomized studies was found by Partsch et al,13 who showed that, in 12 was subjects with evening edema, lower leg edema was reduced by wearing knee-high compression stockings. Compression therapy increases the interstitial tissue pressure, decreases the transmural pressure gradient, so that, and edema is resorbed. There is an improvement in the:
• venous macrocirculation,
• cutaneous microcirculation, and
• lymph drainage.
Compression stockings mainly work when the patient is moving. Muscle exercises to increase ankle pump function, of the kind which are recommended for CVI patients,14 might also represent a treatment option for patients with heavy leg syndrome. Medication to protect the patient against edema may be another treatment option. For example, an in-vitro study15 performed with venule cells showed that biflavonoids from red vine leaf extract promoted repair of damaged endothelial barriers.
It is known from numerous chronic diseases that quality of life can be significantly improved by the use of supportive psychosocial measures.15 For doctors with the appropriate background, such an approach could possibly also be very helpful in dealing with patients with heavy leg syndrome who are receptive to the possibility of their symptoms having a psychosomatic origin. Thus, in our experience, empathy and an explanation that the disease is harmless should feature among the initial psychosocial measures to let the patient know that he is being taken seriously as a whole individual. The literature databases (eg, Medline, Med Pilot) do not contain any reports of psychotherapeutic or psychopharmacological treatment in relation to heavy leg syndrome.
PILOT STUDY
This pilot study sought to establish the most common symptoms in heavy leg syndrome and whether there is impairment of general health.
PATIENTS AND METHODS
Inclusion criteria
Presentation in a practice specialized in venous disorders (01/05-06/05): clinical examination and color-coded duplex ultrasonography show no chronic venous insufficiency, no reflux in the subfascial and epifascial venous system, no obstructions of arterial blood flow, no lymphedema (negative for Stemmer’s sign); CEAP classification16: C (0,1,S), E (p,n), A(n), P(n), feeling of heaviness in the legs (in an upright position, particularly in the afternoon and evening), and patient’s written consent.
Exclusion criteria
Reflux in the subfascial and epifascial venous system, phlebothrombosis or post-thrombotic syndrome, peripheral arterial occlusive disease, lymphedema, lipedema, women during pregnancy or the breastfeeding period, acute lumbago, heart failure, renal insufficiency, severe concomitant disease.
Questionnaire
After clinical and instrumental confirmation of the exclusion diagnosis heavy leg syndrome, the patients were interviewed using a three-part questionnaire consisting of:
• a general part covering personal details, the duration of the complaints, and any concomitant diseases and their treatment,
• a symptom questionnaire with a 10-point scale (0: no symptoms, 10: extremely severe symptoms) for the symptoms:
– feeling of heaviness in the legs,
– leg problems,
– swollen legs,
– feeling of tension in the legs,
– feeling of tiredness in the legs,
– feeling of restlessness in the legs,
– pain in the legs,
– influence of menstruation on leg complaints,
• standardised SF-12 questionnaire (physical, psychological scale) for general state of health.
STATISTICS
The questionnaires were evaluated after checking for completeness and plausibility with SPSS 11.0 statistics software (www.spss.com) run on the Windows XP operating system. The statistical analysis was carried out mainly with descriptive statistical methods (mean, standard deviation); P values <0.05 were regarded as statistically significant.
RESULTS
In the period between 01/05 and 06/05, 21 people (2 men, 19 women) who had been given the exclusion diagnosis heavy leg syndrome were prepared to answer the detailed questionnaire. The mean age of the women was 52.2 years, with an SD of 17.0 years, and the mean age of the men was 25.0 years, with an SD of 5.6 years. The overall mean age was 49.6 years with an SD of 18.1 years (Table II). The mean duration of the complaints was 9.3 (± 6.3 years).
The mean body mass index (BMI) was 23.7 kg/m2 with an SD of 3.0 kg/m2. The question about whether or not there was known phlebological leg disease in the family was answered in the affirmative by approximately half (57%) of the subjects. One, female patient (5%) mentioned smoking, and two women (10%) reported taking ovulation inhibitors. The most common secondary diagnosis was hypertension (14%).
We then asked about various leg complaints, which the subjects rated on a scale of 0-10. The feeling of heaviness, which was the reason for the phlebological investigation, was reported by all and was given a mean rating of 5.3 (± 2.4) on the 10-point scale. A feeling of swelling, feeling of tiredness, and feeling of tension in the legs were reported very frequently, as were general leg problems (Table III). The ratings for restless legs (2.1 ± 2.0) and pain in the legs (2.8 ± 3.3), on the other hand, were relatively low, and these symptoms were reported less often. Six women reported that menstruation had an effect on the leg complaints.
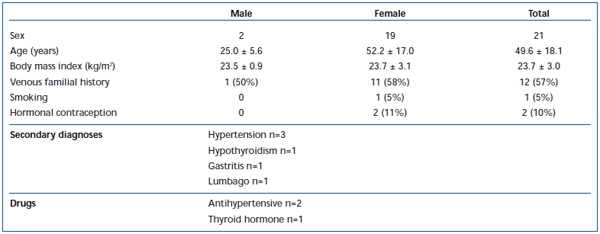
Table II. Patient group (n=21).
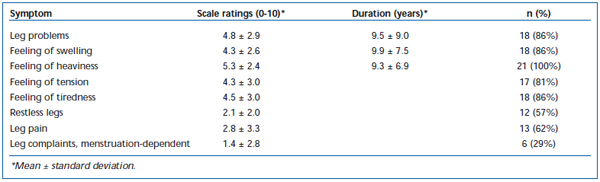
Table III. Leg complaints: results of the symptom scale (10-point scale; 1: no symptoms, 10: severe symptoms).
The standardized evaluation of the physical summary scale yielded a mean value of 46.48 (± 10.21) in the group investigated; the mean value for the psychological summary scale, on the other hand, was 46.94 (± 8.95). Table IV shows the results for the healthy normal German population for the purposes of comparison.
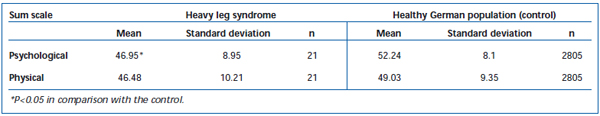
Table IV. SF-12 summary scales for heavy leg syndrome and the random sample of the healthy German population (not affected by venous disease).21,24
On the standardized psychological global scale the psychological scores were significantly higher in the control than patients with heavy leg syndrome (P<0.05). The same trend was seen for the physical summary scale, but no statistical difference was reached.
DISCUSSION
The number of patients in this study is very small, 21, and skewed in terms of sex distribution (19 women and 2 men). The investigation should therefore be regarded as a pilot study. It is clear, however, that the principal symptoms of the functional diagnosis heavy leg syndrome are a feeling of heaviness, feeling of swelling, feeling of tension, and feeling of tiredness in the legs. In addition to physical symptoms, with a mean duration of 9.3 (± 6.9) years, there is a psychosocial burden and impaired quality of life. The term quality of life refers to well-being and the ability to function psychologically, physically, socially, and in everyday life, from the point of view of the patient.17,18
Standardized, tested, valid methods for the measurement of quality of life have now been available for some time.19,20 One of the best known includes the SF-36 and SF-12 Health Survey which, despite its notable brevity, fulfils all test-statistical requirements very well. To obtain information on the quality of life of persons with heavy leg syndrome, we employed the SF-12 questionnaire21 using the interview technique. The SF-12 questionnaire is standardized for the general German population, ie, the data for the different sexes and age groups of the German population are already known.21-26 In the short, 12-item version of SF-36, the evaluation is made with a physical summary scale (consisting of the subscales physical functional ability, physical role function, pain, and general health perception) and psychological summary scale (consisting of the subscales vitality, social functional ability, emotional role function, and psychological well-being). It should be noted, however, that different test instruments may yield different results (agreement validity).18
The pilot study shows that alleged venous symptoms produce a change on the psychological summary scale. However, whether a psychogenic disease leads to the symptoms or whether the leg symptoms produce reactive, psychosomatic symptoms (somatoform disorder) cannot be decided on the basis of the data from the pilot project. The results suggest that patients in the present study have an impaired quality of life due to the heavy leg syndrome they suffer from.
CONCLUSION
Patients with alleged venous symptoms are part of everyday phlebology practice. The exclusion diagnosis heavy leg syndrome should only be made after extensive clinical, instrumental, and quality-of-life investigations. Patients with the above-mentioned symptoms frequently complain of contradictory information and a lack of knowledge of the treatment options on the part of their doctors. Our chief concern should therefore be to provide these patients with effective diagnosis and treatment. Controlled therapeutic studies conducted within a methodologically rigorous framework are desirable.
This article is a modification of the original article published in the journal Phlebologie: Kendler M, Haas E. Subjective venous symptoms: review and presentation of a pilot study. Phlebologie. 2006;35:19-23. It is published here with the kind permission of Maren ULLRICH, Schattauer GmbH, Stuttgart, Germany.
REFERENCES
2. Rabe E, Pannier-Fischer F, Bromen K, et al. Bonner Venenstudie der deutschen Gesellschaft für phlebologie. Epidemiologische Untersuchung zur Frage der Häufigkeit und Ausprägung von chronischen venenkrankheiten in der städtischen und ländlichen Wohnbevölkerung. Phlebologie. 2003;32:1- 14.
3. Bassi G. La patologia venosa funzionale. In: Bassi G, editor. Compendio di terapioe flebologica. Torino: Minerva Medica Ed, 1985.
4. Andreozzi GM, Signorelli S, Di Pino L, et al. Varicose symptoms without varicose veins: the hypotonic phlebopathy, epidemiology and pathophysiology. The ACIREALE project. Minerva Cardioangiologica. 2000;48:277-285.
5. Cloarec M, Barbe B, Griton P, et al. Update on functional venous insufficiency. Phlebolymphol. 1997;3:3-9
6. Tschopp SC. Beinbeschwerden: Subjektive Beschwerden und objektiver Befund. Ergebnisse des Basler Venenprojektfollow- up. Dissertation Universität Basel 1990.
7. Levesesque H, Cailleux N. Heavy and swollen legs. Rev Prat. 2000;50:1183-1188.
8. Maurel E, Azema C, Deloy J, e al. Collagen of the normal and the varicose human saphenous vein: a biochemical study. Clin Chim Acta. 1990;193:27-37.
9. Renaudin JM, Fiscel C, Mercier F, et al. Smooth muscle differentiation in human vein wall at valvular level: comparison with nonvalvular wall and correlation with venous function. Angiology. 1999;50:21-30.
10. Oparil S, Weber MA. Hypertension: a companion to Brenner and Rector’s, “The Kidney”. Philadelphia: WB Saunders. 2000:235-244.
11. Yang D, Vandongen YK, Stacey MC. Effect of exercise on calf muscle pump function in patients with chronic venous disease. Br J Surg. 1999;86:338-341.
12. Blätter W, Davatz U. Zur psychogenes vermeintlich venös bedingter Beinsbeschwerden. Phlebologie. 1993;22:57-60.
13. Partsch H, Winiger J, Lun B. Compression stockings reduce occupational leg swelling. Dermatol Surg. 2004;30:737-743.
14. Yang D, Vandongen YK, Stacey MC. Effect of exercise on calf muscle pump function in patients with chronic venous disease. Br J Surg. 1999;86:338-341.
15. Bross F, Földi E, Vanscheidt W, et al. Psychosoziale Krankheitsbelastungen und Lebensqualität beim Lymphödem. Phlebologie. 1999;28:70-73.
16. Eklöf B, Rutherford RB, Bergan JJ, et al. Revison of the CEAP classification for chronic venous disorders: Consensus statement. J Vasc Surg. 2004;40:1248-1252.
17. Bullinger M. Quality of life – definition, conceptualization and implications – a methodologists view. Theoretical Surgery. 1991;3:21-36.
18. Schölmerich P, Thews G (Hrsg). Lebensqualität als Bewertungskriterium in der Medizin. Stuttgart: Fischer 1990.
19. Anderson RT, Aaronson NK, Bullinger M, et al. A review of the progress towards developing health-related quality-of-life instruments for international clinical studies and outcomes research. Pharmacoeconomics. 1996;10:336-355.
20. Heinzer H, Mir TS, Huland E, et al. Subjective and objective prospective, longterm analysis of quality of life during inhaled interleukin-2-immunotherapy. J Clin Oncol. 1999;17:3612-3620.
21. Bullinger M, Kirchberger I, Ware J. Der deutsche SF-36 Health Survey. Übersetzung und psychometrische Testung eines krankheitsübergreifenden Instruments zur Erfassung der gesundheitsbezogenen Lebensqualität. Zeitschrift für Gesundheitswissenschaften. 1995;3:21-36.
22. Neuner B, Miller PM, Felsmann B, et al. Health-related quality of life in urban surgical emergency department patients: comparison with a representative German population sample. Health Qual Life Outcomes. 2005;3:77.
23. Ellert U, Kurth BM. Methodological views on the SF-36 summary scores based on the adult German population. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2004;47:1027-1032.
24. Gandek B, Ware JE, Aaronson NK, et al. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA (International Quality of Life Assessment) Project. J Clin Epidemiol. 1998;51:1171- 1178.
25. Kurth BM, Ellert U. The SF-36 questionnaire and its usefulness in population studies: results of the German Health Interview and Examination, Survey 1998. Soz Praventivmed. 2002;47:266-277.
26. Bullinger M. German translation and psychometric testing of the SF-36 Health Survey: preliminary results from the IQOLA (International Quality of Life Assessment) Project. Soc Sci Med. 1995;41:1359-1366.
