Superficial vein thrombosis: more dangerous than anticipated
ABSTRACT
Physicians were once taught that superficial venous thrombosis is a rather benign condition. However, more recent information suggests that in quite a number of cases this thrombosis may be complicated by pulmonary embolism. Diverse mechanisms play a role in its development, but it is most frequently linked to varicose veins. Diagnosis is clinical, but ultrasound visualization of the venous segment is essential for the initiation of adequate management. Compression and mobilisation are the cornerstones of treatment. For a short segment thrombosis, nonsteroidal anti-inflammatory drugs exert a proven favorable effect. For longer segments, low molecular weight heparins are preferred. In case of extensive thrombosis, fondaparinux is usually the first line treatment. Information on the effect of the newer anticoagulant drugs for the treatment of superficial venous thrombosis is lacking. Physicians are advised to adapt their views on superficial vein thrombosis according to this new information.
INTRODUCTION
Superficial vein thrombosis (SVT) of the lower limbs is considered by most clinicians to be a rather innocent entity. However, recent information indicates that SVT has a high prevalence and is quite often accompanied by pulmonary embolism, putting the patient at immediate risk.1 Essential aspects of this new information will be summarised in the present review.
DEFINITION
SVT is a clinical entity well known by experts in venous disease and most physicians in general. It presents as an acute clinical condition characterized by a painful, warm and erythematous cutaneous area following the course of a peripheral vein, which often takes on the external aspect of a cord-like structure. It occurs most frequently in the lower limbs, but with increased use of intravenous catheters and injections in the arm, its prevalence in upper limbs has increased sharply.
Thrombus formation in SVT is largely due to an inflammatory process in the venous wall. It typically occurs in varicose veins (primary thrombosis), but can occur in nonvaricose veins, where both thrombosis and inflammation play a role. The thrombus adheres better to the wall of superficial veins than deep vein thrombosis making it less serious; however, SVT is complicated by pulmonary embolism in at least one-third of cases.2,3
Thrombosis is probably a better name for the entity than thrombophlebitis as infection is rarely involved; as a consequence and contrary to common belief, in most patients antibiotics are not necessary. The typical clinical context (Table I) is that of lower limb varicose veins. In many cases, the likelihood of thrombosis developing is increased by immobilization, for example in patients with heart failure, and in chronic conditions due to pulmonary or malignant disease or postsurgery. Upper limb venous thrombosis is now recognized to be occurring more and more frequently following an increase in the use of procedures that cause trauma to the arm veins. Alterations in coagulation status also increase the risk of thrombosis developing.
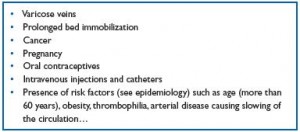
Table I. Most frequent causes of acute superficial thrombosis.
PREVALENCE AND RISK OF SVT
The exact incidence of SVT in not known. It is estimated to be two to three times more frequent than deep vein thrombosis. In many cases, SVT is a mild condition that resolves spontaneously. As a consequence the patient does not seek medical assistance or treatment, and it can be assumed that the prevalence is much higher than actually documented. There is therefore a need for new studies on the prevalence and complications of SVT. It is estimated that 20%-33% of SVT cases, almost one-third, are complicated by asymptomatic pulmonary embolism, while 2%-13% are associated with life-threatening symptomatic pulmonary embolism.4-6 Although these data require further confirmation and documentation, they indicate that SVT is far from a benign entity.
DIAGNOSIS
The diagnosis of SVT is primarily clinical, based on the presence of redness and tenderness along the vein, which is often transformed into an easily identifiable palpable cord. There is often some local or regional edema of the surrounding tissues. In most cases there is no edema of the whole leg as long as the deep venous system is not involved, although there are exceptions to this rule. When SVT is extensive, it is often very painful. During recovery, the inflammation and thrombus often resolve. Recanalization usually occurs after a few months. In cases where there is no recanalization, this may lead to a hardening of the tissues often accompanied by pigmentation.
Ultrasound color flow examination is mandatory to determine the precise location and extent of the SVT. During the healing phase it is also useful for documenting the degree of recanalization. The status of the deep venous system should also be evaluated, and the distance of the SVT to junctions measured. When there is an acute greater saphenous vein thrombosis, ultrasound shows a characteristic increased cross sectional diameter with homogenous echolucent intraluminal material and lack of compressibility.7 It is recommended that both legs be examined in all patients.
MANAGEMENT
In all patients, but particularly in cases of nonvaricose SVT, a full clinical examination is necessary and attention should be focused on specific causes. Thrombophilia and cancer need to be excluded as SVT can be among the first signs of another, as yet undiagnosed disease. In a retrospective analysis of 140 consecutive patients, an association of SVT and malignancy was found in 18 (12.9%) patients.8
In the acute phase of SVT, several options for treatment are available, although there are not many strong recommendations, based on proven information, on the best action to take.9 The most important message that physicians should be aware of is that SVT is not a benign disease.
The following steps should be considered in the treatment of acute SVT:
• Compression
• Mobilization
• Pharmacological treatment
There is a general consensus that compression is helpful in relieving symptoms and may contribute to healing of the thrombotic process.10 Fixed compression, used as the only treatment, has been shown to improve duplex findings in 81% of patients.11 Both bandages and graduated elastic compression stockings can be used; in extensive cases, both types of compression may be applied. It is recommended that the compression bandage should exceed the thrombosed section by at least 10 cm. Compression should be applied for at least 2 weeks, but in varicose patients, it should be continued as a chronic treatment.
The concept of mobilisation has changed the treatment of SVT entirely. A long-held belief was that patients in the acute phase of thrombosis should rest and avoid any movement of the leg. The reasoning was understandable and largely consisted of helping the thrombus to stabilize and avoid the danger of having loose material embolized into the circulation. Current views differ quite fundamentally. It is now considered that bed rest favors the progression of thrombus formation, largely in the direction of the deep venous system. The general consensus is therefore that patients should walk regularly and avoid prolonged periods in bed, seated, or even standing.
Although there are no well-controlled studies proving the validity of this approach, clinical experience shows beneficial effects including a clear improvement in patient quality of life that resembles the favorable effects of training in patients with peripheral arterial disease and even coronary ischemia.
Anticoagulation remains the pharmacological treatment of choice. Treatment will differ according to the length of the thrombosis, which should be determined by ultrasonic examination, performed by well-trained technicians with plenty of experience. As a general rule, the following steps are advised.
If the length of the thrombosis is 5 cm or less, treatment is with nonsteroidal anti-inflammatory drugs (NSAIDs). These can be given locally or systemically12 and reduce pain and most likely perivenous inflammation. In a large, double-blind study comparing NSAIDs, low molecular weight heparin (LMWH) and placebo in 427 patients with documented acute superficial vein thrombosis, NSAIDs (in this case Tenoxicam) significantly reduced the risk of thrombosis extension at the level of the superficial vein at day 12, with no major bleeding.13 However, there was no change in the incidence of deep venous thrombosis. NSAID should not be given in addition to anticoagulants.12 In contrast to arterial thrombosis, there is no proven argument in favor of antiplatelet drugs for this indication.12
If the length of the thrombosis is up to 10 cm (as judged by ultrasound examination), regular anticoagulant therapy is indicated, including LMWH, unfractionated heparin (UFH), and vitamin K antagonists. LMWH can be given as either a prophylactic or therapeutic dose.14 In the above-mentioned double-blind study,13 LMWH also significantly improved the course of SVT. The Cochrane Database Review Group confirmed a positive effect compared with placebo after analysis of 24 studies in 2469 patients, but underlined the rather poor methodological quality of several studies.9 The Cochrane group suggested using an intermediate dose of LMWH for at least 1 month.9 During the early days, this treatment also helps in bridging toward use of oral antivitamin K drugs. An international normalized ratio (INR) of 2.5 should be aimed for.
In cases of extensive thrombosis (longer than 10 cm), especially when several other risk factors are present, there is grade B recommendation, evidence level 2,15 to start fondaparinux, largely based on the findings of the Calisto study.16 Calisto was a double-blind, multicenter study where fondaparinux (2.5 mg/day) and placebo were compared in 3002 patients. The primary efficacy outcome was a composite of death, symptomatic deep vein thrombosis and extension/recurrence of SVT. The outcome at Day 47 was 0.9% in the fondaparinux-treated patients and 5.9% in the placebo group (P<0.001). The efficacy of fondaparinux was also demonstrated in every component of the composite outcome except for death, which was extremely low in the whole study. These results are quite convincing even if there may be some discussion on the cost-effectiveness.17
Clinical experience and a few clinical papers have reported an improvement in local signs and symptoms after applying topical drugs such as diclofenac, ibuprofen and other gels. Their effect is often well accepted and appreciated by patients, although local irritation or allergy can occur. However, none of these studies has convincingly demonstrated a decrease in the incidence of deep vein thrombosis or extension of the SVT.
There is a great expectation that newer classes of anticoagulant drugs will be tested for this indication. To date, the limited information available concerns deep vein thrombosis.
Surgery is rarely indicated for acute SVT. Excision of the involved vein can be performed when symptoms persist after 2 or more weeks of intensive medical treatment (see above). If there are concerns for further extension of the thrombosis, ligation of the vein and eventually excision can be considered, although there is not much support for this type of treatment and almost no well controlled, randomized studies.
Compression and mobilization remain the basic aspects of treatment in the chronic phase, controlling conditions for the patient both at home and at work. Standing immobile for long periods of time is generally accepted to be a provoking factor for venous insufficiency. Ad hoc advice should be given, involving both the physician and manager at the work place. Some drugs have been proven in well-controlled studies to relieve symptoms and heal skin lesions.18 Further research will continue to develop new drugs to treat this important and highly prevalent entity.
In contrast to the acute phase, there are ample indications for surgical treatment in the chronic phase, including stripping and ligation. For smaller vein segments, foam sclerotherapy is likely to be safe and beneficial when performed with ultrasound guidance. However, in all cases, it is important to respect the advice on mobilisation and compression as detailed above. A focus on epidemiology will help determine which patients are at risk and require more intensive management, with clear guidance on mobilization and eventually compression.19,20
CONCLUSIONS
SVT has been considered by many in the medical world to be an innocent entity without significant consequences. However, a recent review of previously published data has pointed toward a high prevalence of pulmonary emboli associated with this condition. It should also be recognized that in most cases SVT leads to some degree of venous insufficiency, not only causing symptoms and incapacity to work, but also creating the background for stasis, new episodes of thrombosis, and skin changes including venous ulcers.
Essential pillars in the treatment of acute SVT are compression, mobilization, and anticoagulation. Several studies, published in high-quality journals, have shown the beneficial effects of both old and newer anticoagulant drugs. After relief of the symptoms and signs associated with the acute phase, great care should be taken in the chronic phase, where venous insufficiency can develop and lead to symptoms, work incapacity, and skin changes. An understanding of the epidemiology of SVT is useful to determine which patients are at increased risk. The information provided in this review will hopefully focus readers’ attention on the often widely underestimated relationship that exists between the peripheral vascular system and the heart.21
REFERENCES
1. Kalodiki E, Stvrtinova V, Allegra C, et al. Superficial vein thrombosis: a consensus statement. Int Angiol. 2012;31:203-216.
2. Partsch H, Mostbeck A. Lungenembolien bei oberflächlicher Thrombophlebitis? Acta Med Austr.1979;6:159.
3. Verlato F, Zucchetta P, Prandoni P, et al. An unexpectedly high rate of pulmonary embolism in patients with superficial thrombophlebitis of the thigh. J Vasc Surg. 1999;30:1113-1115.
4. Wichers IM, Di Nisio M, Buhler HR, et al. Treatment of superficial vein thrombosis to prevent deep vein thrombosis and pulmonary embolism: a systematic review. Haematologica. 2005;90:672-677.
5. van Langevelde K, Lijfering WM, Rosendaal FR, Cannegieter SC. Increased risk of venous thrombosis in persons with clinically diagnosed superficial vein thrombosis: results from the MEGA study. Blood. 2011;118:4239-4241.
6. Decousus H, Quéré I, Presles E, et al. Superficial venous thrombosis and venous thromboembolism: a large, prospective epidemiologic study. Ann Intern Med. 2010;152:218-224.
7. Mozes G, Kalra M, Carmo M, et al. Extension of saphenous thrombus into the femoral vein: a potential complication of new endovenous ablation techniques. J Vasc Surg. 2005;41:130-135.
8. Mouton WG, Kienle Y, Muggli B, et al. Tumors associated with superficial thrombophlebitis. Vasa. 2009;38:167- 170.
9. Di Nisio M, Wichers IM, Middeldorp S. Treatment for superficial thrombophlebitis of the leg. Cochrane Database Syst Rev. 2007:CD004982.
10. Nicolaides AN, Allegra C, Bergan J, et al. Management of chronic venous disorders of the lower limbs: guidelines according to scientific evidence. Int Angiol. 2008;27:1-59.
11. Mayer W, Partsch H. Superficial thrombophlebitis: a harmless disorder? Scope Phlebol Lymphol. 1999;2:36-38.
12. Kearon C, Akl EA, Comerota AJ, et al. Antithrombotic therapy for VTE disease: Antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-based Clinical Practice Guidelines. Chest. 2012;141:e419S- 494S.
13. Exoxaparin study group. A pilot randomized double-blind comparison of a low-molecular-weight heparin, a nonsteroidal anti-inflammatory agent, and placebo in the treatment of superficial vein thrombosis. Arch Intern Med. 2003;163:1657-1663.
14. Kolodiki E, Nicolaides AN. Superficial thrombophlebitis and low-molecular– weight heparins. Angiology. 2002;53:659-663.
15. Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328:1490.
16. Decousus H, Prandoni P, Mismetti P, et al. Fondaparinux for the treatment of superficial-vein thrombosis in the legs. N Engl J Med. 2010;363:1222-1232.
17. Blondon M, Righini M, Bounameaux H, et al. Fondaparinux for isolated superficial-vein thrombosis of the legs: a cost-effectiveness analysis. Chest. 2012;141:321-329.
18. Coleridge-Smith P, Lok C, Ramelet A-A. Venous leg ulcer: A Meta-analysis of adjunctive therapy with micronized purified Flavonoid Fraction. Eur J Vasc Endovasc Surg. 2005;30:198-208.
19. Fowkes FG, Evans CJ, Lee AJ. Prevalence and risk factors of chronic venous insufficiency. Angiology. 2001;52:S5-S15.
20. Evans CJ, Fowkes FG, Ruckley CV, et al. Prevalence of varicose veins and chronic venous insufficiency in men and women in the general population: Edinburgh vein study. J Epidemiol Community Health. 1999;53:149-153.
21. Clement DL, Belch JJ. Vascular disease public education: the mandate is international. Int Angiol. 2004;23:1-4.
