The causes of edema in chronic venous
Paris, France
SUMMARY
The edema associated with chronic venous insufficiency (CVI) is the most common type of edema (90%). Like all types of edema, it is defined by an increase in interstitial fluid volume. It differs from other types of edema in terms of its association with microangiopathy of an initially functional and then organic nature, a consequence of the venous stasis which injures the endothelium, impairs endothelial function, and induces severe hemorheological abnormalities. The repercussions at the tissue level are linked to the instigation of inflammatory processes involving numerous chemical mediators, resulting in fibrosis, capillary rarefaction, and hypoxia.
The edema of chronic venous insufficiency is the first sign of microangiopathy. This is why, for very good reason, it is classified as Grade 3 in the CEAP classification, which is made up of 7 grades of increasing severity. Volumetry, a simple investigation, has become a routine screening test for this condition.
INTRODUCTION
Edema is defined as an increase in interstitial fluid volume. It causes an objective clinical symptom frequently encountered in chronic venous insufficiency1 (CVI) and corresponds to Grade 3 in the CEAP2 classification (1995) which classifies CVI into 7 grades of increasing severity. It causes disability both in the form of symptoms (pain, heaviness, cramps) and in the form of its esthetic impact, and is one of the factors which diminishes patients’ quality of life.3 It represents 90% of all etiologies of edema. Treatments, whether physical (in the form of compression) or pharmacological, focus on reducing this edema,4 which is easily measured using a routine investigation.5
While most types of edema (cardiac, renal) do not cause pain or ulceration because they only involve functional microangiopathy (impairment of capillary permeability), the type of edema associated with CVI is characterized by its painful nature and its tendency to result in trophic complications because of its association with ischemic organic microangiopathy.
THE MAIN FEATURES OF THE PROBLEM
The type of edema associated with CVI is characterized by an increase in the volume of subcutaneous interstitial fluid in the lower limbs associated with hemodynamic problems caused by venous stasis. Starling’s law establishes an equilibrium across the endothelial wall with hydrostatic pressure and oncotic pressure for the intravascular compartment and interstitial pressure for the extravascular compartment.
Mechanism of organic microangiopathy
The hydrostatic forces in the heel and foot range between almost zero in the supine position (a few millimetres of mercury) to 100 mm Hg in the standing position, with this pressure dropping significantly on exertion. The venous circulation in the lower limbs is therefore subject to these considerable variations in pressure which “batter” the upstream venous microcirculation. It is the excessive nature of these constraints and the lack of pressure reduction on exertion caused by the venous reflux of CVI (known as “stasis”) which creates the initiating stimulus for microangiopathy and CVI. What follows is simply the establishment of a vicious circle: stasis ➔ impaired capillary permeability ➔ functional microangiopathy compensated by the lymphatic system ➔ decompensated functional microangiopathy (edema) ➔ venular hemorheological abnormalities (endothelium, leucocytes, mediators) ➔ organic microangiopathy with capillary rarefaction (becoming glomerular), hypopigmentation and fibrosis ➔tissue ischemia (white atrophy), hypoxia ➔ opening of arteriovenous shunts ➔ aggravation of stasis and closing of vicious circle.
The type of edema associated with CVI is by no means a sign of the onset of CVI since it reflects the saturation and overflow of the compensatory lymphatic system (silent phase). The severity is not related to the edema itself but to the microangiopathy with which the edema is associated.
THE CAUSES OF EDEMA IN CHRONIC VENOUS
INSUFFICIENCY
Macrocirculatory causes
CVI is characterized by venous reflux, the consequences of which constitute stasis. Venous obstruction may also be present, but it is inconstant and often marginal. Varicose veins, venous compliance problems, and deep vein and perforator abnormalities form the basis of CVI, but edema may be absent in compensated varicose disease (Grades 1 and 2 in the CEAP classification). These abnormalities are easily identified by measurement of ambulatory venous pressure.1,6
Microcirculatory causes
– Capillary hyperpermeability
Capillary hyperpermeability is a direct consequence of stasis caused by an imbalance in Starling’s law in favour of excessive fluid output (water, electrolytes, dissolved substances, proteins). Under normal conditions, there is an excess daily output of around 4 L of dissolved substances. This is the normal capillary output which is usually compensated by lymphatic resorption of an equivalent volume. The type of edema associated with CVI is an extreme symptom of this physiological phenomenon. This mechanism shows how the interactions between the venous and lymphatic systems are closely linked.
Starling’s law: a reminder
Starling’s law governing capillary exchanges is:
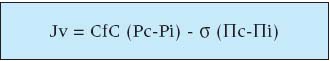
Jv = Exchange
CfC = Coefficient of filtration
Pc = Capillary pressure
Pi = Interstitial pressure
ó = Oncotic coefficient
Πc = Capillary oncotic pressure
Πc = Interstitial oncotic pressure
This increase in capillary permeability is easily identifiable under fluorescence capillaroscopy by measurement of the pericapillary halo (interstitial fluid) which doubles in size from 80 μ in CVI.7 As long as the lymphatic system absorbs this excess, the disease remains compensated and there is no edema.
– Hemorheological abnormalities
Hemorheological abnormalities are also the direct consequence of the stasis which perturbs the endothelium and its relations with the components of the blood.
a) Leukocytes
Since the studies conducted by Coleridge-Smith,8 we know that leukocytes play a preponderant role in this disorder (review in ref 9). Neutrophils and monocytes are activated by venous hypertension with perturbation of certain selectins, integrins and immunoglobulins.10 In CVI, these leukocytes, which are usually able to move around on the endothelial surface under the influence of an L-selectin which can be measured in the plasma,11 develop a greater tendency to stick to the endothelium under the influence of an integrin which usually facilitates their perivascular migration. They then remain prisoners within the local microcirculation, and this trapping activates certain physiological inflammatory processes.
b) Red blood cells
Under conditions of stasis, the red blood cells in the capillaries which have become glomerular aggregate12 and cause capillary thrombosis which is clearly visible in biopsies.
c) Plasma
Patients with CVI show raised fibrinogen levels and therefore plasmatic hyperviscosity which accentuates the stasis. Certain hemostatic mechanisms are also perturbed, one example being the reduction in physiological fibrinolysis.
d) Platelets
Patients with CVI show increased monocyte-platelet aggregation.13
– Morphological changes in the capillaries
The capillaries react to these constraints. Capillaroscopy shows a reduction in the number of capillaries per square millimetre, capillary thrombosis, abnormal neogenesis (glomerular capillaries7,14) and very uneven distribution with almost no capillaries in some areas (white atrophy).
Impact on tissue
The impact of these disorders on the tissue bring into play multiple chemical mediators related to inflammatory processes (hypopigmentation), resulting in a type of fibrosis called lipodermatosclerosis. The trapping of leukocytes is accompanied by the production of free radicals with their well-known harmful effects which generate edema. In addition, the volume of the edema causes mechanical separation of the capillary from the cell it is feeding, and thus aggravates cellular hypoxia. This multifactorial hypoxia in turn causes vasodilation with opening of shunts which serve to aggravate the existing stasis.
Most of the factors described above interfere with each other, link into complex microangiopathy, and are the direct or indirect causes of the CVI-related edema. We do not have any simple biological markers to quantify this venous stasis which generates edema, but metalloproteinase- 9 may be one path worth exploring.15
CONCLUSION
The precise causes of the type of edema associated with CVI are now well known. They are part of a greater entity involving hemodynamic abnormalities linked to venous disease which gradually induces complex cutaneous microangiopathy.
These perturbations are usually curable with appropriate venous treatments which have proven their efficacy in both medical and economic terms.16
REFERENCES
2. Porter JM, Moneta GL and an International Consensus Committee on Chronic Venous Disease. Reporting standards in venous disease: an update. J Vasc Surg. 1995;21:635-645.
3. Launois R, Reboul-Marty J, Henry B. Construction and validation of a quality of life questionnaire in chronic lower limb venous insufficiency (CIVIQ). Qual Life Res. 1996;5:539-554.
4. Collège des Enseignants de Médecine Vasculaire. VALMI. 2003.
5. Vayssairat M, Maurel A, Gouny P, Baudot N, Gaitz JP, Nussaume O. La volumétrie: une méthode précise de quantification en phlébologie. J Mal Vasc. 1994;19:108-110.
6. Taheri SA, Pendergast D, Lazar E, Pollack LH, Shores RM, McDonald B, Taheri P. Continuous ambulatory venous pressure for diagnosis of venous insufficiency. Am J Surg. 1985;150:203-206.
7. Bollinger A, Fagrell B. Clinical Capillaroscopy. Hogrefe: Huber Publishers; 1990:93-106.
8. Coleridge Smith PD, Thomas P, Scurr JH, Dormandy JA. Causes of venous ulceration: a new hypothesis. BMJ. 1988;296:1726-1727.
9. Carpentier PH. Rôle des leucocytes dans la pathogénie des troubles trophiques veineux. J Mal Vasc. 1998;23:274-276.
10. Saharay M, Shields DA, Porter JB, Scurr JH, Colerdige Smith PD. Leucocyte activity in volunteers in response to experimental venous hypertension. Phlebology. 1997;12:122-126.
11. Saharay M, Shields DA, Porter JB, Scurr JH, Colerdige Smith PD. Leucocyte activity in the microcirculation of the leg in patients with chronic venous disease. J Vasc Surg. 1997;25:265-273.
12. Le Devehat C, Vimeux M, Bertrand A. Insuffisance veineuse et hémorhéologie. Influence de la stase veineuse sur l’agrégation et la désagrégation érythrocytaire. J Mal Vasc. 1989;14:307-311.
13. Peyton BD, Rohrer MJ, Furman MI, et al. Patients with venous stasis ulceration have increased monocyte-platelet aggregation. J Vasc Surg. 1998;27:1109-1116.
14. Fagrell B. Vital microscopy and the pathophysiology of deep venous insufficiency. Int Angiol. 1995;14(suppl):18-22.
15. Jacob MP, Cazaubon M, Scemama A, Prié D, Blanchet F, Guillin MC, Michel JB. Plasma matrix Metalloproteinase-9 as a marker of blood stasis in varicose veins. Circulation. 2002;106:535-538.
16. Korn P, Patel ST, Heller JA, Deitch JS, Krishnasastry KV, Bush HL, Kent KC. Why insurers should reimburse for compression stockings in patients with chronic venous stasis. J Vasc Surg. 2002;35:950-957.
