The plantar venous pump: Anatomy and physiological hypotheses
Jean-François UHL1,2
Claude GILLOT1
1- Laboratoire d’Anatomie
Unité de Recherche URDIA- EA 4566,
Université Paris Descartes – France
2- Centre de Chirurgie des Varices Paris
Défense, France
SUMMARY
An anatomical study of 200 (cadaveric) feet injected with latex demonstrated that Lejars’ concept of the venous sole of the foot is incorrect: the true plantar venous pump consists of the plantar veins, located deep between the plantar muscles and compressed by weight bearing during walking. The normal venous sole (Bourceret) is a thin network and its dilatation (Lejars) is pathological, attributed to severe distal venous stasis.
The blood reservoir of the foot, which moves upwards as the result of manual compression of the plantar venous pump or weight bearing during walking, is located in the plantar veins.
This is the reason why, in patients with venous disease, it is so important to make sure that the static anatomy of the foot is normal. In fact, the venous pump of the foot is the first step in venous return of blood during walking, just before the calf pump.
INTRODUCTION
Background
1861: Sucquet: observed taut channels in the thickness of the skin going from a pre-capillary arteriole to a post-capillary venule. This structure shunts the capillary blood and facilitates passage into the arteriovenous anastomoses. These channels are observed in areas of high pressure in the sole of the foot and the palm of the hand.
1885: Bourceret1 demonstrated a fine plexus of dermal and subdermal veins along the entire plantar surface of the foot. This venous network drains directly into the medial and lateral marginal veins, and into the medial and lateral plantar veins via fine perforators in fatty tissue.
1889: Braune2 observed an arch—the anterior part of the plantar venous network by the interdigital veins and which opens into the dorsal veins. He confirmed the existence of the fine plexus described by Bourceret.
1890: F. Lejars3 was the first to describe a venous pump activated by walking: the plantar venous pump. He described large superficial vessels which form a true plantar reservoir. But these large superficial veins were injected by an arterial approach under high pressure and, in fact, Lejars’ observation is a technical artifact.
1993: J. H. Scurr,4 using plethysmography, recorded changes in volume and estimated the quantity of blood ejected from the sole of the foot as 20-30 ml during contraction.
1993: Gardner and Fox5 proposed the hypothesis which states that it is the stretching of the medial and lateral plantar veins which, with each step, pushes the blood into the saphenous veins and the deep venous network and that the pump of the foot and that of the calf function sequentially.
MATERIAL AND METHODS
We used 200 non-selected, non-embalmed cadaveric subjects (with a high average age).
After exposing the medial marginal vein, a no. 19 butterfly venous catheter was inserted and directed towards the toes (countercurrent therefore to blood flow). The common femoral vein was approached and a tube was inserted to perform lavage-irrigation with soapy water, repeated several times, until a clear liquid was obtained. Then undiluted latex with neoprene was injected, which stained green (120 – 150 ml per limb), for 30 minutes. Dissection was started the next day.
RESULTS
I/ Demonstration of the plantar venous pump
The existence of a plantar venous pump is an unquestionable reality. It is confirmed every day by phlebologists who carry out what they erroneously refer to as “Lejars’ plantar compression maneuver”.
With the patient’s foot immobile, manual compression exerted on the plantar venous arch triggers frank acceleration of blood flow in the posterior tibial veins, revealed in the ankle by Doppler scanning. Therefore, this acceleration of deep blood flow is immediate, intense, and repeated. This is a deep blood reservoir, mobilized by manual pressure exerted on the sole of the foot, corresponding to the lateral (and medial) plantar veins included between two fleshy muscles.
II/ Anatomical description of the veins in the foot
A-Superficial venous network
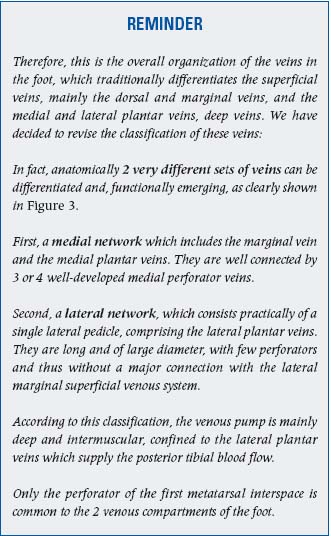
1-Veins in the sole of the foot
The superficial veins in the sole of the foot form a fine network which drains into the marginal veins via small, valve-bearing veins. These valves prevent the passage of blood into the superficial area. In the event of total or partial absence of valves in these superficial plantar veins, moderate dilation of the plantar venous network is observed (the so-called “Bourceret sole” Figure 1A). In contrast, in the event of abnormal reflux, major dilation of this network occurs, leading to “Lejars’ plantar venous sole” (Figure 1B). This venous dilation is produced by severe venous stasis, most often by a superficial and/or deep vein reflux.

Figure 1. 1A: Non-valvular veins of the cutaneous network
visible in the totality of the sole of the foot.
Reflux by the small terminal collector veins (red lakes): Bourceret
venous sole, plexus of small veins, 1 to 2 mm in diameter.
1B: A case of plantar superficial reflux, abnormal.
Reflux with major dilation of the plantar cutaneous veins.
2-Marginal veins
The superficial venous network also comprises medial and lateral marginal veins. The medial marginal vein arises from the perforator of the first metatarsal interspace and continues, giving rise to the great saphenous vein. This vein forms a functional unit with the medial plantar veins which we will discuss later. The lateral marginal vein also arises from the perforator of the first metatarsal interspace and ends in the short saphenous vein.
3-The interdigital veins drain into Braune’s arch from the dorsal veins
B-The deep venous network of the foot
This network comprises two layers of veins as seen in this frontal section (Figure 2).
1- The deep “bony” veins, located in contact with the tarsal bones in the concavity of the bony arch, which drain cancellous bone.
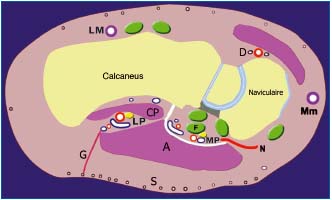
Figure 2. Medial longitudinal section of the foot showing the
muscle topography of the large plantar veins.
LP: lateral plantar veins, intermuscular, located in the slit which
separates the fleshy body of the plantar quadratrus (PQ) from that
of the abductor hallucis (A): effective muscular action
MP: medial plantar veins: fibrous and tendinous relations: tendonlong
flexor of the hallux (F) and deep fascia of the abductor muscle:
rigid structure with no great direct action on the veins.
N: navicular perforator, G: perforator in fatty tissue, Mm: medial
marginal vein, LM: lateral marginal veinw
2- The network of large collecting veins, the musculotendinous veins (Figure 3).
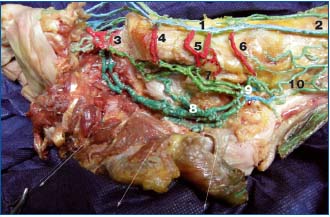
Figure 3. The two venous systems of the foot (the first metatarsal
is partially resected). The medial system: the plantar and marginal
veins communicating by many perforators. The lateral system, the
lateral plantar veins, a true venous pump in the foot. 1=the medial
marginal vein, 2=the great saphenous vein, 3=the perforator of the
1st metatarsal interspace, 4=the cuboidal perforator, 5=the
navicular perforator, 6=the malleolar perforator, 7=the medial
plantar veins (light green) have low capacities and communicate
via the medial perforators, 8=the lateral plantar veins (dark
green), with their large diameter and length form a true blood
reservoir in the plantar venous pump, 9=the calcaneal plexus,
10=the posterior tibial veins.
This network comprises the medial and lateral plantar pedicles, which join together posteriorly to form the calcaneal confluent of the plantar veins.
– The medial (or internal) plantar pedicle is short, about 5 cm in length, and relatively rectilinear. It occupies only the posterior part of the sole of the foot, behind the tendon of the lateral fibular vein. It comprises two veins and in some cases is plexiform:
– it extends along the medial border of the foot and receives the perforators of the medial marginal vein.
– laterally, it receives blood from the adjacent muscles: the abductor hallucis, the flexor digitorum brevis and the plantar quadratus muscle.
These two veins are small and project on tendons and so are ineffective for the plantar venous pump.
The lateral (or external) plantar pedicle is longer (12 cm), curved, and larger because it is located between the two muscle layers of the sole of the foot, and thus is compressed during contraction. It arises opposite the 1st metatarsal interspace from the venous arch of the 1st interspace.
It emerges laterally, and then is rectilinear and empties into the calcaneal confluent vein where it joins with the medial plantar veins. This plexus joins the posterior tibial veins. The plantar pedicle generally is formed of two veins that parallel the artery but sometimes only one collecting vein exists along part of its pathway. Along their pathway, the lateral plantar veins sometimes present fusiform dilations, the plantar sinuses, comparable to those of the medial head of the gastrocnemius muscle and the soleus muscle. This is evidence in support of a venous pump.
The lateral plantar pedicle receives perforators from the lateral marginal vein, perforators in fatty tissue, the inter-metatarsal veins (in particular from the 1st and 4th metatarsal interspaces), the calcaneal veins and the veins in the adjacent large plantar muscles.
3-The calcaneal confluent of the plantar veins lies in the calcaneal groove. It is formed by the medial and lateral plantar veins and appears as a fine venous plexus which condenses to form the posterior tibial veins.
The calcaneal confluent of the plantar veins (Figure 3) is semi-plexiform, multi-valvular, and connects to the great saphenous vein by the tibial malleolar perforator vein (sometimes the navicular). This calcaneal confluent lies at the distal end of the plantar muscle pump. It distributes blood both into the posterior tibial and into the great saphenous vein via the malleolar and navicular perforators.
The terminal valves of the medial and lateral plantar veins are competent in normal subjects.
C-The perforator veins
4.1-The perforator of the 1st metatarsal interspace , generally of large diameter, is a relay because it is connected to the venous arch from the 1st interspace, which is the starting point of all venous networks in the foot, superficial and deep. The anterior tibial veins, the lateral plantar pedicle, and the medial plantar pedicle arise from it. This arch is situated in relation to the superficial dorsal arch which joins the medial marginal vein and the lateral marginal vein.
4.2-The medial marginal perforator veins (Figures 3 and 4) open into the medial marginal vein and provide the three-root origin of the great saphenous vein. They differentiate into plantar and dorsal veins.
4.2.1 There are three plantar perforators (Figure 4):
– the malleolar (or talus): close to the malleolus, it joins the confluent of the plantar veins
– the navicular: it is close to the tubercle of the scaphoid bone
– the cuneiform: it crosses the 1st cuneiform bone
4.2.2 The dorsal medial perforator veins (shown in yellow )
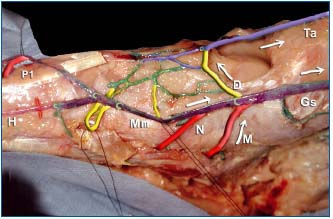
Figure 4. Dorsal and plantar medial perforators, connected to the
medial marginal (Mm) vein at the origin of the great saphenous
(Gs) vein.
Note the three-root origin of the great saphenous vein: it arises
from the medial marginal vein Mm, the dorsal communicator
which opens into the anterior tibial veins aT, and the malleolar
communicating vein connected to the calcaneal plexus.
Note the large diameter of the communicating vein of the 1st
metatarsal interspace P1. Note also the abrupt change in diameter
of the dorsal vein of the foot after receiving the dorsal perforator
vein D, thus becomes the anterior tibial vein.
-Mm: Medial marginal (or internal) vein
-Gs: Great saphenous vein.
H: Dorsal vein of the hallux
Ta: anterior tibial veins
The dorsal perforator veins are shown in yellow:
-D= Dorsal perforator vein which communicates anteriorly with
the anterior tibial veins (Ta).
The plantar perforator veins are shown in red: anteriorly to
posteriorly
-P1=Perforator of the first metatarsal interspace
-N navicular -M malleolar or the talus
The dorsal perforator vein (D) communicates in front with the anterior tibial veins (Ta).
4.3-The lateral marginal perforator veins (Figure 5): there are two—the calcaneal and the cuboidal which join the lateral marginal vein. They cross the lateral fibular tendons (inter-tendinous and subtendinous perforator).
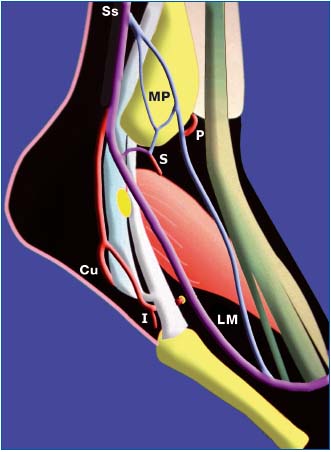
Figure 5. The lateral perforator veins of the foot. Origin of the
main portion of the short saphenous vein (Ss)
– the lateral marginal (LM) vein is not a constant finding, but
often is large.
– the lateral malleolar plexus MP, on the contrary, is a constant
finding. It gives rise to perforator veins:
P= premalleolar S= submalleolar.
– A common C vessel of the lateral perforators of the foot exists, a
true third root of the short saphenous vein;
it crosses the fibular long flexor tendons: the intertendinous (I),
and cuboidal (Cu) perforator veins
COMMENTS
A/ Review of the steps in lower limb venous return4-14
– At rest, the venous pump is not active, as we shall subsequently see, therefore the system is necessary and sufficient in itself to provide specific continuity of venous return.
– When a subject goes from the seated to the standing position, under the influence of gravity, the weight of the column of blood exerts a pressure of about 80 mm of mercury.
– After a certain number of steps (ie, about 10 – 25 m), ankle pressure falls to 30 mm of mercury. This decrease is related to mobilization of the volume of blood, due to activation of the different venous pumps in the lower limb during walking.
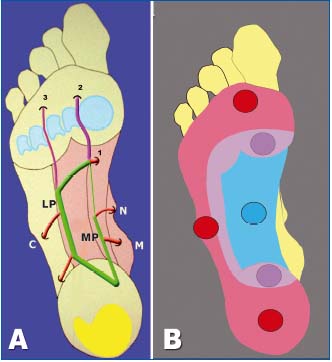
Figure 6. A: Projection of the plantar venous axes.
The plantar compression maneuver shows that while ejection is
very effective in the plantar arch on which the venous axes project,
normally it is zero in the weight-bearing area. This is also evidence
that contradicts Lejars’ theory.
The principal perforators: C =cuboidal, N =navicular,
M =malleolar
1°E=perforator of the 1st metatarsal interspace 3°E=perforator of
the 3rd interspace
B: relations with the weight-bearing area.
Red circular patch = weight-bearing area on the ground.
Blue circular patch= manual compression area of the plantar
veins.
A well-known mechanism in the calf and in the thigh, where the intramuscular veins of the triceps and of the quadriceps act as a blood reservoir, in particular, those of the soleus muscle and the medial head of the gastrocnemius muscle, and those of the vastus lateralis muscle.
Contraction ejects the volume of blood and muscle relaxation allows filling of this reservoir.
A series of valves channels the blood propelled to the root of the limb and prevents any reflux.
B/ Where is the plantar venous pump located?
In fact, different lines of evidence confirm that the plantar venous pump is located deep, intermuscularly:
– The plantar venous axes are connected directly to the posterior tibial veins, which are extensions of them.
– The direction of the valves indicates that blood flows from the deeper part to the superficial part.
– The volume of blood ejected by the pump is 20 to 30 ml, which corresponds to the capacity of the lateral and medial plantar veins. These veins are primarily inter-muscular, thus pointing to the intervention of a motor apparatus for venous ejection during walking, which adds to the pressure exerted by the foot on the ground.
The anatomical description of the lateral plantar veins shows the 3 components of this pump which determine its functioning: (Figure 7)
1- Anteriorly, the suctioning pole, directed towards the toes. There are many supply pathways: the highly vascularized toes, the highly developed metatarsal muscles, the large metatarsal perforator vein (arising from the superficial network of the medial marginal vein)
2- The middle portion comprises the body of the reservoir of the pump, whose average volume is 15 to 25 ml. It is enhanced at this level by bony and muscular veins, the medial and lateral perforators. Weight bearing and the action of walking produce a massage effect on the plantar vascular area.
3- Posteriorly, the calcaneal confluent, which corresponds to the ejection pole, empties with full diameter into the posterior tibial veins. This is confirmed in everyday phlebological practice by the high elevation of posterior tibial blood flow after manual compression of the plantar surface, confirmed by many authors.4,8-10
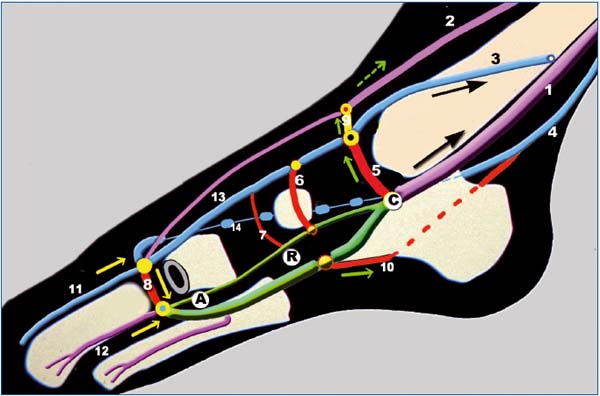
Figure 7. Hypotheses on functioning of the venous pump in the foot
The pump (shown in green) comprising the plantar veins is polarized and contains 3 parts going from front to back: A suction pole (A), a reservoir (R), and an ejection pole (C) the calcaneal confluent.
Anteriorly, the distal pole (directed towards the toes) or aspiration A: blood enters the pump during raising of the foot in plantar flexion by relaxation of the plantar muscles.
The pump is supplied by the highly vascularized toes and the highly developed metatarsal muscles. The pump is supplied with superficial blood carried by the communicator vein of the 1st interspace (8).
The body of the pump or reservoir R is enhanced by the bony and muscular veins, but also by superficial blood by the medial and lateral perforator veins of the foot (in red).
The distal or ejection pole is represented by the calcaneal confluent C.
Blood is supplied to the posterior tibial veins (1), but also the great saphenous vein (3), by the malleolar perforator vein (5), and to the anterior tibial veins (2) by the dorsal perforator vein (9).
1: Posterior tibial veins 2: Anterior tibial veins
3: Great saphenous vein 4: Short saphenous vein
5: Malleolar perforator vein 6: Navicular vein
7: Cuneiform perforator vein 8: Perforator vein of 1st metatarsal interspace
9: Dorsal perforator vein 10: Calcaneal perforator vein
11: Dorsal vein of the hallux, very larg 12: Intermetatarsal vein
13: Medial marginal vein 14: Lateral marginal vein
Three phases can be described during walking:
1- The weight-bearing phase: contact of the foot on the ground produces direct compression of the reservoir in the sole of the foot between weight-bearing areas.
2- The impulse phase: Weight bearing on the forefoot with flexion of the toes which fix the foot on the ground, resulting in compression of the pump in the musculotendinous plane by muscle contraction;
3- The suspension phase of the foot, lifted off the ground, allows filling of the pump.
During walking, the pump reloads cyclically when the foot is lifted up and empties when weight bearing is applied.
As just described, the plantar venous pump is the only one effective up to the calf, where its action is taken over by the calf pump of the soleus muscle. Its dual action, on both the deep and the superficial saphenous vein circulation, underlines the unimpeded circulation of blood between the two vascular compartments. In fact, the perforator veins of the foot have an important specific anatomical feature, that of not having any effective valves.
CONCLUSIONS
The blood reservoir, mobilized by manual pressure on the sole of the foot and emptied during weight bearing during walking, is not a superficial one in “Lejars’ sole”, but rather is deep. It corresponds to the lateral plantar veins between the two fleshy muscles and is compressed at each step of walking.
These anatomical data explain why it is important to check for normal static posture of the foot in a patient with chronic venous disease, to ensure proper emptying of the plantar venous pump during walking.
Similarly, the utility of stimulation of the plantar venous pump in the prevention of post-surgical deep vein thrombosis should be emphasized15-17 in high-risk patients. This can be done by manual massage going upwards, by intermittent pneumatic compression, or by simple elastic compression starting at the root of the toes.
This venous pump of the human foot is the first step in venous return from the lower extremity to the heart. The calf pumping mechanism, produced by contraction of the soleus muscle and of the gastrocnemius muscle, then takes over.4,5,14
This work was granted the Prize for the ‘best abstract’ at the XVIth World Meeting of the Union Internationale de Phlébologie, Principality of Monaco, 31 August-4 September 2009.
REFERENCES
1. Bourceret. Circulation locale. Procédé d’injection des veines. Note présentée à l’académie des sciences, 1885.
2. Braune W, Muller P. Das Venensystem des Menschlichen Körpers II Lieferung, 1889.
3. Lejars F, Les veines de la plante du pied. Archives de physiologie. 5° série, 1890.
4. Scurr JH, Coleridge Smith PC. La pompe musculaire du pied importance physiologique et clinique. Phlébologie. 1993;46:209-216.
5. Gardner AM, Fox RH. Peripheral venous physiology. In: Gardner AM, Fox RH, editors. The return of the blood to the heart London: John Libbey; 1993:61-87.
6. Barcroft H, Dornhorst AC. Demonstration of the muscle pump in the human leg. J Physiol. 1948:39-48.
7. Ludbrook J. The musculovenous pumps of the human lower limb. Am Heart J. 1966;71:635-641.
8. Gardner AM, Fox RH. The venous pump of the human foot: preliminary report. The impulse system reduces deep-vein thrombosis and swelling. Bristo Med Chir J. 1983;98:109-112.
9. Fox RH, Gardner AMN. Video phlebography in the investigation of venous physiology and disease. In: Negus D, Jantet G, editors. Phlebology ‘85. London: John Libbey, 1986:68-71.
10. Pho RWH, Binns M. Anatomy of the venous foot pump. Injury. 1988;19(6):443-445.
11. Pho RWH, Binns M. Plantar venous pump. Injury. 1990;21(2):129-130.
12. Lassau N. Epouse Vandenbusche. La semelle veineuse plantaire de Lejars. Thèse Paris-VII, 1991.
13. Gillot Véronique. Appareil locomoteur et pompe veineuse plantaire: un exemple de couplage anatomique et fonctionnel. Thèse Paris-VII, 1993.
14. Raju S, Fredericks R, Lishman P, Neglen P, Morano J. Observations on the calf venous pump mechanism: determinants of postexercise pressure. J Vasc Surg. 1993;17:459- 469.
15. Fordyce MJF, Ling RSM. A venous foot pump reduces thrombosis after total hip replacement. J Bone Joint Surg. 1992;74B:45-49.
16. Bradley JG, Krugener GH, Jager HJ. The effectiveness of intermittent plantar venous compression in prevention of deep venous thrombosis after total hip arthroplasty. J Arthroplasty. 1993;8:57-61.
17. Gillet JL. Thrombose des veines plantaires. Phlébologie. 2004;57(1): 87-90.
