THERAPY OF VASCULAR DISEASES
LECTURES
Selective factor Xa inhibition: role in acute coronary
syndromes
A. G. G. TURPIE (Canada)
Fondaparinux (Arixtra®) is a synthetic antithrombotic agent with specific anti-factor Xa activity. Its pharmacokinetic properties allow for a single daily injection without the need for monitoring. It was recently compared with enoxaparin for the prevention of venous thromboembolism (VTE) in major orthopedic surgery in 4 randomized doubleblind studies. The metanalysis of these studies showed a major benefit of fondaparinux over enoxaparin achieving an overall risk reduction of VTE of 55.2% without increasing the risk of clinically relevant bleeding [AGG Turpie et al. Arch Intern Med. 2002;162:18333-1840.
Aspirin (ASA), clopidogrel, and low-molecularweight heparins (LMWH) are indicated for the treatment of acute coronary syndromes (ACS). In non-ST-elevation ischemia (NSTEMI) or in unstable angina pectoris, guidelines now suggest in using ASA in addition to anti-ischemic therapy and LMWH. Clopidogrel is added, except in patients who are potential candidates for urgent coronary artery bypass grafting. For patients undergoing percutaneous coronary intervention, glycoprotein IIb/IIIA inhibitors are added. After invasive treatment, or if no invasive treatment is required, the combination of aspirin (ASA) and clopidogrel is recommended for long-term treatment of non-STEMI patients. Patients with acute STsegment elevation ischemia (STEMI), should receive thrombolysis if primary angioplasty is not indicated or available.
Fondaparinux was evaluated for treatment of acute non-STEMI patients in phase II PENTUA study. This study included 1147 patients who received either enoxaparin 1 mg/kg twice daily or fondaparinux once daily at the dosage of 12, 8, 4 or 2.5 mg for 9 days. Fondaparinux was found to be as effective for reducing thrombotic events and as safe for major bleeding events as enoxaparin. In the PENTALYSE study, 326 STEMI patients were included. They received ASA and thrombolysis by rtPA, in combination either with fondaparinux or UFH. Similar coronary patency rates were demonstrated in all groups at 90 minutes, but there was a strong trend in decreasing reocclusion in the fondaparinux group.
Two phase III trials are actually ongoing (OASIS 5 and 6), and are planned to include 16 000 non STEMI patients and 10 000 STEMI patients to evaluate fondaparinux as an alternative treatment to LMWH or UFH for ACS.
Heparins, oral anticoagulants, and ASA:
survival of the fittest
J. FAREED (USA)
The current management of thrombotic and cardiovascular disorders is largely dependent on the use of classic anticoagulants and antiplatelet agents such as heparin, warfarin, and aspirin. Although the cumulative usage of these drugs extends beyond 200 years for several indications, the mechanism of their actions and therapeutic spectrum is not fully explored. Several of the consensus groups have continued to endorse these drugs for the thrombotic and vascular indications. The last decade has also witnessed the development of several newer anticoagulants and antiplatelet drugs with claimed superiority over conventional drugs. Parenteral antithrombin agents such as hirudin, angiomax, and argatroban have been used with specific indications such as heparin-induced thrombocytopenia. Oral antithrombin agents such as ximelagratran were developed with claimed superiority over oral anticoagulant drugs for broad indications. Heparinomimetic agents, namely arixtra, which represents an indirect parenteral anti-Xa agent, have been used mainly for postorthopedic surgical indications. Synthetic parenteral anti-Xa agents have also been developed without clinical success. Oral anti-Xa agents are currently developed for several clinical indications, including extended management of thrombotic and cardiovascular disorders. While these drugs are useful in heparin and oral anticoagulant-compromised patients, almost all have a narrow therapeutic index and are monotherapeutic. Furthermore, their pharmacology is not completely understood. The development of glycoprotein IIb/IIIa inhibitors added a new dimension in parenteral antiplatelet therapy with profound impact on interventional cardiology. However, these drugs were not promising as oral agents. Furthermore, they have very narrow safetyefficacy windows. The ADP-receptor inhibitors such as ticlopidine and clopidogrel, represent drugs with antiplatelet effects which are different from aspirin. However, the efficacy of these agents is dependent on the simultinaeous use of aspirin. Moreover, ticlopidine exhibits serious adverse effects by suppressing PMM production. Long-term toxicity data is not available. Thrombosis is a polypathologic process requiring drugs with polypharmacologic actions. The newly developed drugs can only mimic the effects of conventional drugs in multiple therapeutic forms. Thus heparin, oral anticoagulants, and aspirin will further expand in optimized forms. The newer agents may be useful in heparin-compromised patients and targeted therapeutic approaches.
Response to variations in antiplatelet drugs:
clinical manifestations
H. K. BREDDIN (Germany)
Currently three types of antiplatelet drugs (APD) are in use:
– aspirin
– ADP-receptor antagonists and thienopyridines (ticlopidine and clopidogrel)
– glycoprotein IIb/IIIa receptor antagonists as Abciximab, eptifibatide, and integrilin.
Aspirin reduces stroke and coronary events by about 25% with the safe dose range being from 75 to 325 mg per day. however, in many cases low doses of aspirin, such 100 mg per day, may not be enough with 10% of nonresponders. Resistance to aspirin is currently discussed but still ill-defined. The inhibition of platelet function in different test systems shows large variations. Whether patients who do not respond to aspirin in this test have less clinical benefit has been thought likely, but by no means proven. A better standardization of tests is urgently needed before they are used in prospective studies.
Ticlopidine and clopidogrel are widely used, especially in patients with coronary heart disease. They effectively prevent acute reocclusions in patients undergoing PCI. These drugs can be monitored using platelet aggregation induced by APD. Also here non-responders have been described. How much inhibition of APD-inducted aggregation is needed to provide clinical efficacy? Due to poor standardization of the aggregation tests this can not be answered today. Does clopidogrel inhibit progression of peripherial arterial occlusive disease? This is not known because it has not yet been studied. Rules for such studies are urgently needed. Glicoproteins IIb/IIIa inhibitors (GP IIb/IIIa inhibitors) are potent drugs. Nowadays there are three groups of these drugs:
– humanized monoclonal antibodies (abciximab, YM 337)
– IV effective synthetic peptides and peptidomimetics (integrilin, tirafiban, lamifiban, DMP728)
– orally effective peptidomimetics (mainly “double prodrugs” – xemilofiban, sibrafiban, fradafiban) It is very likely that for their clinical effects a strong inhibition of the GP IIb/IIIa receptors is needed, possibly more than 95%. There is, however only one study with insufficient data on this important question. GP IIb/IIIa inhibitors are not mentored in clinical practice. It is that their clinical efficacy could be improved by simple monitoring tests. Orally available GP IIa/IIIb receptor antagonists have failed to show any clinical benefit. The reason for this is much discussed but virtually unknown.
Three practical conclusions:
– platelet function inhibitors should be used in combinations
– aspirin + clopidogrel is a promising combination, today mainly used in PCI
– aspirin + clopidrogrel are also promising for new studies in PAOD.
Chairpersons: S. A. MOUSA (USA), M. R. LARSEN (Denmark)
Serum transaminases do not increase after a 4-week
administration of fondaparinux.
No episodes of thrombocytopenia are seen after 4 weeks
of fondaparinux in major orthopedic surgery
M. R. LARSEN (Denmark)
Fondaparinux is a synthetic selective factor Xa inhibitor with a favorable profile:
– absolute bioavailability 100%
– linear dose-dependent pharmacokinetics
– long elimination half-life ~ 17 hours allowing once
– daily injection
– low interindividual variability allowing fixed dose and no monitoring
– distribution volume close to blood volume
– excreted unchanged in the urine – no metabolism
– selective binding to ATIII
Turpie et al proved the superior efficacy of fondaparinux after major orthopedic surgery in their comparative study (2002 – fondaparinux versus enoxiparin) with a similar safety profile. Increase in serum transaminases is known as an adverse event with a number of antithrombotic compounds. The variations in serum transaminases observed after major orthopedic surgery may be related to surgical context or to study drugs. HIT is a severe complication of heparin therapy mediated by antibodies to PF4 complex. The safety of prolonged administration of fondaparinux on liver enzymes, on blood platelet count, and the evolution of serum transaminases in the double-blind randomized PENTHIFRA-PLUS trial in which fondaparinux was administered up to 4 weeks after hip fracture surgery were studied. Serum transaminases (AlT, AST) were measured at randomization (7 days after surgery) and at the end of the study (4 weeks). Variation in serum transaminases during the study period were comparable between the two groups. Increase in serum transaminases was rare in the 1-week as well as 4-week fonadaparinux groups. Penthifra-Plus demonstrated that extending fondaparinux prophylaxis from 1 week to 4 weeks after hip fracture surgery reduced significantly by around 90% all venous thromboembolism events and symptomatic deep vein thrombosis and pulmonary embolism. Extended administration of 2.5 mg fondaparinux from 1 to 4 weeks did not increase clinically relevant bleeding or significant changes in liver enzymes in comparison with placebo. Increase in serum transaminases observed in the short-term trials was more likely related to surgical context rather than to fondaparinux therapy. There were no cases of heparin-induced thrombocytopenia with prolonged administration of 2.5 mg fondaparinux.
Inhibition of thrombin activatable fibrinolytic inhibitor by
heparin and defibritide
M. FLORIAN (USA)
Thrombin activatable fibrinolitic inhibitor (TAFI) is a carboxypeptidase capable of modulating fibrin, rendering it resistant to the action of plasmin. Polyelectrolytes such as heparins produce varying degrees of inhibition of the functional activity of TAFI, presumably due to their effects on thrombinthrombomodulin complex. The authors assessed the molecular weight dependence on the inhibition of TAFI by heparin and defibrotide.
In the summary the authors stated that heparins and LMWHs are capable of inhibiting the activation of TAFI. The degree of inhibitions depends on the molecular weight of the heparin fractions. Higher molecular weight fractions inhibit TAFI more effectively. Defibrotide and aptamers isolated from defibrotide are capable of inhibiting TAFI activation. Molecular weight of defibrotide fractions also influences the inhibition of TAFI. Heparin and LMWHs inhibit TAFI more effectively than does defibrotide.
These studies clearly demonstrate that both MW and MW composition of heparins and defibrotide contribute to the differential inhibition of TAFI which in turn may contribute to their therapeutic actions. The profibrinolytic effects of heparin may be a result of its ability to inhibit TAFI. Bleeding is a commonly seen adverse effect of heparins. Since the primary hemostatic plug is composed of platelets and fibrin strands, a molecularly transformed fibrin resistant to localized lysis may be more important in restoring hemostasis than the native fibrin molecules. TAFI is implicated in maintaining primary hemostatic plug at the site of vascular insult, where a residual amount of this enzyme is important. It is important to consider that an indiscriminant inhibition of TAFI functionality may lead to bleeding, whereas a balanced inhibition may add to the therapeutic efficacy and
Thrombin activatable fibrinolytic inhibitor (TAFI) modulation
by heparin: influence of endogenous variables
M. FLORIAN (USA)
The primary objective of this research was to determine the effect of various heparins on the functionality of TAFI as measured by using a specific synthetic substrate. Additionally, the relevance of the observed inhibition of TAFI with the antithrombin potency was also addressed.
The study design was as follows:
– to validate a newly developed chromogenic substrate method for the functional evaluation of TAFIa
– to determine the effect of various anticoagulants on the functional TAFI levels at expected clinical concentration
– to demonstrate the relevance of thrombin inhibitory actions and TAFI functionality
– to demonstrate any potential direct inhibitory actions by anticoagulant drugs on TAFIa.
Citrated plasma samples from 289 healthy persons and patients treated with heparin, antithrombin, and oral anticoagulants were collected. A chromogenic substrate-based method (Pefakit® TAFI, Pentapharm Ltd, Switzerland) was used to determine TAFI levels. Pefakit® TAFI (Pentapharm Ltd, Switzerland) utilizes a specific substrate which measures the generated TAFIa. In the current assay configuration, the effect of anticoagulant drugs on TAFI and TAFIa is measured. Various anticoagulant drugs produce different degrees of TAFI inhibition which is not proportional to their relative antithrombin actions. Hirudin, which is the strongest inhibitor of thrombin, produces relatively weaker effects on TAFI. Also anti Xa drugs have a relatively weak effect on TAFI. Molecular weight dependence is observed with heparin and LMWHs. The level of heparinization is directly proportional to the inhibition of TAFI activity, as observed at the prophylactic, therapeutic, and interventional levels. Oral anticoagulants in the therapeutic range (INR 2.0-2.5 ) did not have any effect on TAFIa. In conclusion the authors stated that using a chromogenic substrate-based method for TAFI functionality, the differential inhibitory effects of various anticoagulant drugs can be readily assessed. The differences in the inhibitory profile of TAFI may also contribute to the observed variations in heparinization responses among patients. Finally the authors presented the clinical implications:
– anticoagulant drugs such as heparins and antithrombin agents can produce varying degrees of modulation of the fibrinolytic process by downregulating TAFI functionality. This modulation of TAFI functionality by anticoagulant drugs may directly impact on their safety and efficacy. While an inefficient inhibition of TAFI mat result in a hypercoagulable state, excessive inhibition of TAFI can lead to bleeding.
Generic versions of commercially available
low-molecular-weight heparin (LMWHs): product individuality
in therapeutic implications
J. MADDINENI (USA)
Enoxaparin represents one of the most widely prescribed LMWHs, with approval for several applications. This drug is made by using benzylation followed by alkaline depolymerization of porcine mucosal heparin. One of the patents covering this drug has already expired, whereas the second patent will expire in December 2004. Therefore, this LMWH will be without patent coverage after this time. Being aware of this, several manufactures of LMWHs have produced generic versions of enoxiparin with claimed equivalence in accordance with the available specifications. Though the generic products may have a similar molecular weight and anti-Xa potency, their biochemical and pharmacologic behavior may not be the same, and may require further characterization. For the approval of generic versions of enoxaparin, four different products have been submitted. To utilize standardized analytical and biochemical methods which have been employed to demonstrate differences among LMWHs and to validate the generic equivalence or nonequivalence in various available generic versions the authors compared three generic versions of enoxaparin: two from India and one from Brazil, with the commercial form from the US. The comparison of the molecular profile of the three generic versions and the commercial product did not show any significant differences in terms of MWs but had different oligosaccharide distributions. The heparinase-I digestion profile of two Indian products and the commercial product were identical; however, the Brazilian product showed a strong resistance to the depolymerization effects by heparinase -1. The commercial product and the Indian generic version were digested to deca- and dodecasaccharides. The USP anticoagulant activities of each of these agents were comparable. Similarly, the anticoagulant activities as measured by PT, aPTT, Heptest, and TT were comparable in all these agents except for the Brazilian product. The anti-Xa and IIa actions of different products were similar; however, the Brazilian product was somewhat weaker. However, the calculated anti-Xa/IIa ratio of the Brazilian product was comparable to that of the other products. These studies clearly suggest that the molecular and biological activities of the generic versions can be adjusted to mimic the branded product. However, these adjustments may not be sufficient for bioequivalence. The authors concluded that some generic versions of enoxaparin have been introduced in many countries around the world. These products exhibit similar molecular and anti-Xa/IIa activities. These agents have not been evaluated for the specific attributions, which are unique for enoxaparin. This has clinical implications:
1. Enoxaparin represents a low-molecular-weight heparin with wide clinical indications, including arterial, venous, and cardiovascular use.
2. The dosage range varies widely, and this drug is administered with other anticoagulant and antithrombotic agents.
3. The generic version of enoxaparin must exhibit all physiochemical and biological attributes to mimic the clinical performance of the branded product.
CARDIOVASCULAR EFFECTS OF STATINS
Chairpersons: S. NOVO (Italy), R. PAOLETTI (Italy)
New evidences on CV event reduction with statins in type 2
diabetic patients
H. COLHOUN (Ireland)
The risk of CV death remains high in diabetic patients compared with nondiabetic patients with the same cholesterol levels. Several studies (CARE, 4 S, Heart Protection Study) have demonstrated that adding statins to existing treatments reduces the risk of cardiovascular events by about 22% to 25% in secondary prevention for a wide range of high-risk patients, irrespective of their initial cholesterol concentrations. The place of lipid-lowering for primary prevention of CV events is, however, more controversial. The ASCOTT-Lipid Lowering Arm study included 10 305 hypertensive patients with nonfasting total cholesterol concentrations of 6.5 mmol/L or less, with at least three cardiovascular risk factors. They were given atorvastatin 10 mg or placebo. Nonfatal and fatal coronary heart disease risk was reduced by 36% in the atorvastatin group compared with the placebo group. The statistical analysis of the subgroup of diabetic patients was lacking power. The Heart Protection Study documented the beneficial effect of simvastatin in reducing all-cause mortality among 5963 diabetic patients but there is still a paucity of large prospective randomized outcome trials designed only for diabetic patients. However, some guidelines (Europe) now routinely recommend lipid-lowering treatment for all type 2 diabetic patients while others recommend treating only patients with an increased LDL-c concentrations and an increased risk of coronary heart disease. The Collaborative Atorvastatin Diabetes Study (CARDS) is still ongoing. This study will evaluate the effectiveness of atorvastatin in type II diabetic patients for primary prevention of cardiovascular events. A total of 2838 patients have been included and randomely assigned to receive either atorvastatin 10 mg daily or placebo. They all have at inclusion LDL-c < 4.14 mmol/L and hypertension (79% of the patients), retinopathy (30%), microalbuminuria (11%), or current smoking (23%). None of the patients have a history of cardiovascular disease, coronary heart disease, or peripheral arteriopathy. The results of this study and the results of other ongoing studies such as Fenofibrate Intervention and Event Lowering in Diabetics will define the place and the safety of lipid-lowering strategy in primary prevention of cardiovascular events in diabetic patients.
The antiatherothrombotic effects of statins: the ATROCAP
study results
M. CORTELLARO (Italy)
Thrombogenicity of the atherosclerotic plaque is dependent on the imbalance between tissue factor (TF) and tissue factor pathway inhibitor (TFPI). Statins are able to inhibit the expression of TF, but their effects on plaque thrombogenicity have never been reported in humans. Patients (n=59) eligible for bilateral carotid endarterectomy (CEA) were included in the study. After the first CEA, they were randomly assigned to atorvastatin 20 mg daily or placebo till the second CEA, 4 to 6 months later. Histological and immunohistochemical analyses of the endarterectomy specimens were performed with particular reference to the distribution of TF and TFPI. TF, TFPI antigens and TF activity and compared between the two endarterectomy specimens. Plaques removed at the second CEA in the atorvastatin group had a lower inflammatory cell infiltrate and a reduction in TF activity, TF and TFPI antigens compared with plaques of the placebo group. These results indicate that atovarstatin decreases the inflammatory activity of the atheromatic plaque and may reduce the risk of plaque thrombogenicity.
Cortellaro M, Cofrancesco E, Arbustini E, et al. Atorvastatin and thrombogenicity of the carotid atherosclerotic plaque: the ATROCAP study. Thromb Haemost. 2002;88:41-47.
Lipid-lowering and non-lipid-lowering effects of statins in
cerebrovascular diseases prevention
P. RUBBA (Italy)
Clinical trials on secondary prevention of coronary heart disease showed a reduction in cerebrovascular events among patients undergoing long-term treatment by statins. While it is generally accepted that the clinical beneficial effect associated with statin treatment is due to the lipid-lowering effect, the possibility that statins have additional protective effects on the arterial system cannot be excluded;
– Carotid plaque stabilization:
Carotid plaque stabilization can be evaluated by high-resolution B mode ultrasound which assesses intima-media thicknesss (IMT) of the common carotid artery and of the carotid bifurcation. First, maximum IMT (measured at baseline) evaluates the lesion severity and the mean maximum IMT (measured during the follow-up) evaluates the lesion extension. Pravastatin has been shown to decrease the mean maximum IMT while the first maximum IMT remained unchanged, suggesting that pravastatin is able to inhibit the formation of new lesions in asymptomatic moderately hypercholesterolemic patients.1 Moreover, marked LDL reduction (<100 mg/dL) with a high potent statin treatment provides superior efficacy for atherosclerosis regression, measured by carotid IMT, at 1 year.2
– Enlargement of carotid lumen:
Maintained lipid-lowering therapy with simvastatin has also been demonstrated to be associated with significant regression of established atherosclerotic lesions. Lesions were assessed by high-resolution noninvasive magnetic resonance imaging.3 Vessel wall thickness and vessel wall area decreased during lipid-lowering therapy while lumen area increased slightly.
– Reduction of stroke, transient ischemic attacks, and vascular bruits:
The Prospective Pravastatin Pooling Project pooled three large placebo-controlled randomized trials and included 19 768 patients with 102 559 person-years of follow-up. Pravastatin 40 mg daily, in secondary prevention, reduced stroke rates (fatal and non fatal) by 20%. The benefit was observed mostly for ischemic strokes as there was no statistical difference for hemorrhagic or strokes of unknown cause.4 The Heart Protection Study also provided evidence of stroke prevention through simvastatin treatment in individuals at high risk of atherosclerotic cardiovascular disease, independently of the presence of coronary disease.5 The MIRACL study determined that intensive cholesterol lowering with atorvastatin over 16 weeks in patients with acute coronary syndromes reduced the overall stroke rate by half and did not cause hemorrhagic stroke.6 More recently, the ASCOT-LLA study showed that stroke rate can be reduced in hypertensive normolipidemic patients, without any evidence of coronary heart disease. Patients of the study received atorvastatin 10 mg/d or placebo. A 27% reduction of stroke incidence was observed during the 3 year-followup period.7
In conclusion, statins have a protective effect on the arterial system at different levels: carotid plaque stabilization, enlargement of carotid lumen, fewer vascular bruits and TIAs, and prevention of stroke in high-risk patients.
REFERENCES
2- Taylor AJ, Kent SM, Flaherty PJ, Coyle LC, Markwood TT, Vernalis MN. ARBITER: Arterial Biology for the Investigation of the treament effects of Reducing Cholesterol: a randomized trial comparing the effects of atorvastatin and pravastatin on carotid intima medial thickness. Circulation. 2002;106:2055-2060.
3- Corti R, Fuster V, Fayad ZA, et al. Lipid lowering by simvastatin induces regression of human atherosclerotic lesions: two years follow up by high resolution non invasive magnetic resonance imaging. Circulation. 2002;106:2884-2887.
4- Byington RP, Davis BR, Plehn JF, et al. Reduction of stroke events with pravastatin: the Prospective Pravastatin Pooling (PPP) Project. Circulation. 2001;103:387-392.
5- Heart protection study collaborative group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20 536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002;360:7-22.
6- Waters DD, Schwartz GG, Olsson AG, et al. Effects of atorvastatin on stroke in patients with unstable angina or non-Q-wave myocardial infarction: a Myocardial Ischemia Reduction with Agressive Cholesterol Lowering (MIRACL) substudy. Circulation. 2002;106:1690-1695.
7- Sever PS, Dahlof B, Poulter NR, et al. Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lowerthan- average cholesterol concentrations, in the anglo-Scandinavian Cardiac Outcomes Trial-Lipid Lowering Arm (ASCOTT-LLA): a multicentre randomised controlled study. Lancet. 2003;361:1149-1158.
Is it possible to stop the progression of atherosclerosis?
The REVERSAL Trial
G. DE FERRARI (Italy)
Glagov’s remodeling hypothesis of atherosclerosis indicated that the arterial lumen is reduced at the end stage of the process. At earlier stages, there is a production of atheroma on one part of the vassel, then extension occurs until eventually it becomes circumferential with a reduced arterial lumen. Intravascular ultrasound (IVUS) provides a complete evaluation of the vessel circumference, the vessel wall, and the lumen area. Atheroma area and total atheroma volume can be calculated on a target vessel. IVUS can visualize atheroma in cases of diffuse symmetrical disease with nonsignificant stenosis on arteries, which is one of the limitations of angiography. In the REVERSAL trial, 654 patients requiring coronary angiography were included. They were randomly assigned to receive atorvastatin 80 mg/d (agressive treatment) or pravastatin 40 mg/d (moderate treatment) during 18 months of follow up. Atorvastatin significantly decreased total cholesterol, LDL-C, and triglycerides more than pravastatin. Total atheroma volume decreased in the atorvastatin group while it increased in the pravastatin group. It was possible to calculate that a 50% reduction of LDL-C was associated with an absence of atherosclerosis progression, measured by IVUS. This was correlated with a significant reduction of major cardiovascular events after 30 months of follow-up in the atorvastatin group compared with the pravastatine group (Relative risk=16).
ORAL COMMUNICATIONS
Microcirculation reactivity ischemia and pharmacological
reperfusion
C. ALLEGRA (Italy)
Microcirculation is a terminal part of the systemic circulation and connecting system between arteries, venous macrovessels, and tissues. It is called “exchange circulation” since it is the site of hemo-tissue exchanges. The microcirculatory unit consists of a terminal arteriola, a meta-arteriola, the capillary network, the initial venula, arterovenous anastomoses, lymphatic capillaries, and nervous fibers, all held in matrix of connective tissue. The local blood perfusion is regulated through two main ways: 1) the metabolic pathway, conditioned by changes in tissue PO2 and PCO2 which uses endothelium-derived relaxing factor (EDRF) or nitrous oxide (NO) and adenosine as vasoactive mediators; 2) the myogenic pathway, conditioned by changes in pressure of flow. A third mechanism invoked is arteriolar vasomotion. It consists of rhythmic arteriolar dilatations and constrictions at frequently of 1 to 20 to 30 cycles per minute, inversely proportional to the diameter of the terminal arteriole. The cyclical changes in arteriolar diameter are accounted for by a presence of a sphincter-type endarterial thickening, acting as a pacemaker. Vasomotion is thought to be responsible for: 1) redistribution of the blood flow in the capillary network; 2) changes in capillary blood viscosity, in the oncotic-hydrostatic pressure ratio. In turn the variations of frequency of arteriolar vasoconstriction and vasodilatation seem to be determined by changes in interstitial pressure and PO2, through adenosine-balanced feedback between EDRF and endothelin. Capillary hemodynamics result from arteriolar vasomotion and rheological changes according to stochastic laws. Capillary endothelium lies on the basement membrane and lacks underlying muscle cells. It sets up a continuous barrier which allows diffusion of fluids and muscles though direct and indirect mechanisms of selective transport. Most capillaries have oxygen pressure in the range 20 to 30 mm Hg – it should be apparent that this is not the primary mechanism for tissue oxygenation. The large O2 consumption of the arteriolar wall and primary the endothelium is due to biological activity of these cells and the synthesis and secretion of rennin, prostaglandins, prostacyclins, interleukins, clearance of proteins, lipids, and lipoproteins and mechanical work in contracting against blood pressure. So vessels wall oxygen gradients – and therefore microvessel wall metabolism – increase with vasoconstriction. When oxygen availability has run out, the endothelial damage is not reversible, and consequently thrombosis, decrease in capillary perfusion and density, with tissue damage, occur.
Short and repeated ischemia results in resistance to serious ischemia, increasing ATP and adenosine release by the tissue. Both ATP and adenosine stop white cell activation, and RBC aggregation, they improve fibrinolysis, vessel dilatation, and protect capillaries from reperfusion injury. The restoration of normal vasomotion is requested by greater supply of ATP and decreasing consumption of O2 by arteriolar endothelial cells. Consequently much more O2 is available for ischemic tissues. In practice ischemic preconditioning is interesting to explain:
– the improvement of walking distance after repeated exercise
– the action of some vasoactive drugs
– the target of antiischemiac therapy in the exchange vessels.
Autologous skin grafting in treatment of lower-leg
cutaneous lesions
R. BRAMBILLA, P. MAGGIONI, S. SORDO, G. CIUFFO, S. MANGIAROTTI, E. STELLINO (Italy)
The authors describes a series of 127 patients with lower-leg cutaneous ulcers. There are arterial, venous, and other ulcers whose origins are not clear. After preparing the lesion correctly the treatment was performed with autologous skin grafting obtained with non-woven scaffold (Hyalograft) or with a microperforated lamina of HYAFF (Laserskin). The results are excellent with healing of the ulcer in 110 patients. The patients still have the ulcer close 6 months after complete clinical closure. The authors do not explain whether they have performed any special treatment depending of the origin of the ulcers. This could prove to be another useful treatment for this difficult pathology.
THERAPY
LECTURES
Compression therapy: a powerful but underestimated treatment modality
H. PARTSCH (Austria)
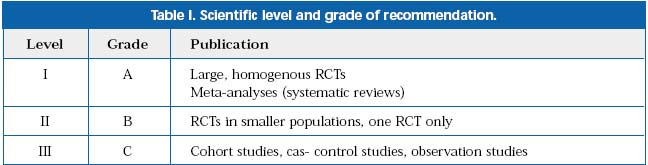
Clear proof of effectiveness of different compression devices endorsed by evidence-based medicine (EBM) will be a prerequisite for reimbursement by health budgets in the near future. Unfortunately, until now randomized controlled trials (RCT) of compression which have demonstrated clinical effects in different setting are very rare or nonexistant. Based on the initiative of the UIP, the available RCTs and systematic reviews reporting outcomes after compression therapy in the different settings of phlebology and lymphology were evaluated by an international group of experts (San Diego, August, 2003). Recommendations were graded A, B or C according to the scientific levels of evidence (Table I).
Positive effects of compression therapy endorsed by EBM criteria (grade A) were found only in two settings: venous ulcers (bandages, not stockings); prevention of thrombosis and postthrombotic syndrome (stocking, not bandages). Grade B recommendations were based on studies of subjective symptoms in small and large varicose veins, postoperative or postsclerotherapy care of varicose veins, acute DVT, and lymphedema. There were no data about compression treatment for patients with CEAP class C4a (stasis dermatitis and pigmentation) and with superficial phlebitis. The most impressive effect of compression reduction of edema (CEAP C3) has not yet been investigated adequately. Future investigations devoted to the efficiency of compression therapy are necessary for planning in conformity with the following demands:
• A priori calculation of sample size, large population (multicenter)
• Objective outcome parameters, eg, ulcers healing
• Pairs of baseline- characteristics (stratification)
• Objective definition of compression pressure and material
• Blinded assessment of outcome
• Publication also of studies with negative results.
EVOLUTION OF DVT
Chairpersons: C. ALLEGRA (Italy), P. GLOVICZKI (USA)
With the participation of C. MOFFAT (UK), E. RABE (Germany),
P. L. ANTIGNANI (Italy), H. PARTSCH (Austria), C. ALLEGRA (Italy),
P. GLOVICZKI (USA)
State of the art in elastic compression
C. MOFFAT (UK)
Two main types of the compression therapy for venous ulcers were presented. Passive compression, is produced by inelastic bandages which counteract the increase in muscle volume resulting from muscle contraction. Active compression is provided by elastic materials. It is independent of muscle activity. There are three types of this material: short-stretch (extension < 70%), medium-stretch (extension 70% to 140%) and long stretch (extension >140%). The treatment of venous ulcers includes:
1. Compression
• Multilayer ( elastic or nonelastic)
• Reduced compression
• Medical stocking
• Intermittent pneumatic compression (IPC)
2. Medical and surgical treatment
3. Appropriate dressing
4. Education of the patients.
The treatment options are different for mobile and immobile (fixed ankle) patients. The first line of the therapy for mobile patients includes multilayer compression (elastic or nonelastic) and then medical stockings as a second line. For immobile patients, first-line therapy includes elastic multilayer compression bandage and combination multilayer elastic bandages with IPC as a second line. Industrial multi-layer bandages including elastic and nonelastic properties (eg, Profore®) have obviously advantages.
Compression therapy in CVD- epidemiological data from the
Bonn Vein Study
E. RABE (Germany)
Atotal of 3072 respondents from the general population of the Bonn and rural townships were included in an epidemiological study (October 2000 to March 2002). The aims of the study were:
1. Estimation of the prevalence of CVI in urban and rural population
2. Investigation of the complaints and type of therapy
3. Identification of risk factors for chronic venous diseases.
A special questionnaire, clinical examination, and duplex scanning were used. Distribution of the respondents according to CEAP classification is presented in Figure 1.
Most responders had a previous history of venous or lymphatic disorders. Signs of deep venous thrombosis and pulmonary embolism were found in 2.9% and 0.9% cases. 1.1% of the patients had leg ulcers. Reflux in the superficial or deep venous system was discovered in 28% of cases. In 0.9% male and 1,2% of females, there were clinical and ultrasound signs of the postthrombotic syndrome. Different types of treatment were used. Compression stockings were used by 14.6% of the responders.
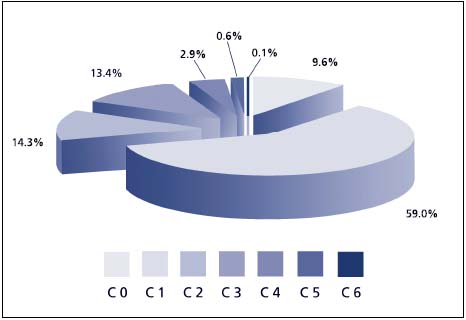
Figure 1. Distribution of the Bonn study respondents according CEAP classification
(N=3072)
Monitoring in DVT evaluation
P. ANTIGNANI (Italy)
One thousand two hundred and thirty-eight patients with suspected DVT were investigated with color-flow duplex scan. DVT was found in 354 cases (28,5%). Localization of the thrombosis and its relation with pulmonary embolism is shown in Table I.
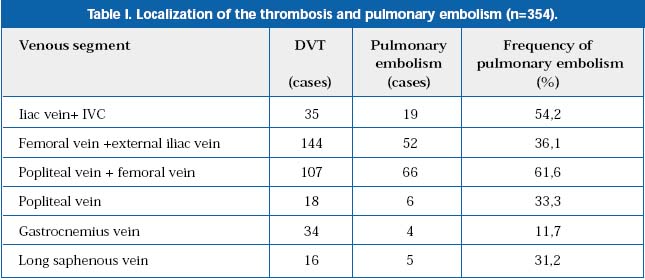
Free-floating thrombi were found in 40 cases (11.2%). Twenty-five patients (60.2%) of this group had pulmonary embolism. Very often calf DVT will extend to involve proximal veins and subsequently cause pulmonary embolism and severe post-thrombotic syndrome. Proximal DVTs resolved very slowly in spite of anticoagulant and compression therapy. Ten percent of patients with symptomatic DVT developed severe post-thrombotic syndrome within 5 years. Also, they have a high risk of recurrent DVT. Superficial femoral vein remained occluded in 15% to 20% cases after DVT. Good collaterals protect from severe venous insufficiency. Seventy-five percent of venous segments which were occluded initially were restored during the subsequent 8 to 12 years. Complete resolution of the thrombus is very rare, and can be found only in 30% of cases. Complete and fast lysis of the thrombus during the first 90 days can restore the lumen of the vein without valve damage and prevent CVI in the future.
Compression therapy reduces symptoms and signs of acute
deep vein thrombosis and post-thrombotic syndrome
H. PARTSCH (Austria)
Fifty three patients with proximal DVT were randomized into 3 groups:
A. Inelastic compression bandages and walking (18 cases)
B.Thigh-length compression stockings (Sigvaris 503) and walking (18 cases)
C. Bed rest for 9 days without compression (17 cases).
All patients received low-molecular-weight heparin (Dalteparin sc, 200 IU/kg/24 h). Disease-orientated parameters (recurrence, pulmonary embolism, bleeding, death, post-thrombotic syndrome) and patient-oriented parameters (QOL, walking ability, pain, edema) were estimated.
In the acute stage of DVT pain and swelling were significantly improved in the groups A and B vs group C. There was no significant difference in cases of pulmonary embolism between the mobile and bedrest groups. CVI symptoms in A and B groups were significantly lower in comparison with group C during 2 years’ follow-up. Thus, immediate ambulation of patients with DVT with good compression on low-molecular-weight heparin provides faster reduction of the symptoms of DVT without serious risk of pulmonary embolism, and reduces the severity of the post-thrombotic syndrome.
LECTURES
Innovation and challenges. The vascular surgeon at the
crossroads
J. FERNANDES E FERNANDES (Portugal)
Innovation has certain requirements (comparison with established technique which is the gold standard, placebo effect, risk versus benefit, costeffectiveness), limitations (adequate information for patient and relatives; pressure from industry and public; individual needs) and regulations (informed consent).
The introduction of endovascular therapy created a hybrid vascular specialist with surgical and interventional skills, working in a vascular center instead of a surgical unit.
Several vascular problems can be resolved with either surgery or less invasive endovascular interventions:
– treatment of carotid lesions
– treatment of lower-limb ischemia
– treatment of abdominal aortic aneurysm
Decisions will depend on the results of properly designed randomized trials.
In the meantime, we have to invest in wellorganized training in vascular science (competence in vascular surgery and medicine).
Minimally invasive treatment of varicose veins
J. BERGAN (USA)
Elimination of reflux in the long saphenous vein (LSV) and perforators with removal of the varicose veins are the basic principles of modern treatment of primary varicoses. Inversion stripping of the LSV provides good long-term results. Unfortunately, crossectomy produces a high risk of neovascularization in the groin region. The neovascularization rate can be as high as 50% during the 5-year follow-up. Radiofrequency coagulation (RFC) and endovenous laser treatment (EVLT) are the new methods of eliminating reflux without crossectomy. RFC provides abolition of reflux and varicose veins in 95.7% of cases during 2 years’ follow-up versus 87% after stripping and 58% after crossectomy. EVLT has a similar rating. The LSV was closed in 94% to 100% of cases during a 3-year follow-up. Blood flow through the superficial epigastric vein and circumflex iliac vein protect the stump of the LSV against thrombosis. Obesity (BMI> 30), anticoagulation treatment, and unsatisfactory technique are the principal causes of a recurrence of reflux and varicoses after RFC and EVLT. Foam sclerotherapy is the method of a choice in the treatment of varicose veins. The foam technique has serious advantages in comparison with liquid sclerotherapy. These are: low concentration, low volume, and high efficacy. The main indications for foam sclerotherapy are saphenous trunk varices, severe CVI, venous angiomas, arteriovenous malformation, and neovascularization after operation. Careful ultrasonic investigation with mapping of all sites of reflux and varicose veins is necessary for the achievement of good results.
Is carotid intervention
grafting necessary?
N. ANGELIDES (Cyprus)
The incidence of neurological vascular events after coronary bypass grafting is from 0.6% to 15%. There are different etiologies of these vascular events but the carotid lesion seems to be the principal etiology. There is no doubt that carotid endarterectomy for symptomatic carotid stenosis must be performed before coronary bypass surgery in patients with stable angina or simultaneously in patients with unstable angina. However there is a lack of evidence, in terms of controlled trials, in patients who need coronary revascularization and present asymptomatic carotid disease. The ACST recommends carotid endarterectomy in healthy men and women under 75 years. The 5-year reduction of neurological vascular events of this group is 6%. The author of this lecture presents one study whose aim is to determine the prevalence of carotid stenosis in coronary surgery patients and determine the timing of carotid and coronary surgery. They review 1250 consecutive carotid duplex studies in asymptomatic patients before coronary surgery. The overall incidence of severe carotid stenosis was 7.36% with this distribution:
– Unilateral stenosis (e 70%) 4.32% cases
– Unilateral stenosis (e 70%) and contralateral occlusion 0.64%
– Bilateral stenosis (e 80% in both sides) 2.4%.
This incidence increases with age and is not different between patients with stable and stable angina. The author states three possibilities in relation to timing for treating these patients:
– Staged surgery, carotid surgery before coronary surgery, in 74 patients
– Simultaneous surgery in 5 patients
– Reverse surgery, coronary surgery prior to carotid surgery, in 13 patients.
The overall neurological morbidity was 6.2%. The final conclusion was not to recommend reverse surgery, and to wait for more results of the carotid stenting before deciding on his indications in this group of patients.
The timing of carotid and coronary surgery in asymptomatic patients continues to provoke an interesting discussion. In the study the small number of patients presented and the distribution do not allow us to make definitive conclusions. For the majority of authors in the literature the mortality and morbidity in the reverse surgery do not favour this option. Nowadays, the principal discussion is the choice between simultaneous or staged surgery. Probably the best solution, until the appearance of specific trials with a sufficient number of patients, it is decided on the timing of surgery depending of the cardiac state. Patients with stable angina must be operated on in stages and patients with unstable angina simultaneously.
STENTS: ADVANCES AND CONTROVERSIES IN
INTERVENTIONAL THERAPY
Chairmen: B. GORENEK (Turkey), Y. HASIN (Israel)
Carotid artery stenting with wallstents:
stent inhealing, and arterial remodeling
H. EHRINGER (Austria)
Duplex ultrasonographic information on inhealing of carotid stents is limited.
This prospective study followed the inhealing of 121 carotid Wallstents (112 patients) by colour duplex sonography at day 1 and at 1, 3, 6, 12, and 24 months.
The layer between stent and perfused lumen (SPL) was evaluated in respect of thickness (mm) and echogenicity. The stent diameter was measured in the proximal, middle, and distal stent area. The ratio PSV ICA/PSV CCA served as a hemodynamic index of the degree of the stenosis.
Inhealing of stent was characterized by three phases:
(1) acute unstable phase: at day 1 the inner stent surface was covered by a thick echolucent layer interpreted as a fibrin layer (median 0.70 mm). This layer disappeared at 1 month and rarely resulted in stent occlusion.
(2) moderately unstable phase: from 1 to 6 months the SPL layer is characterized by an increasing echogenecity and a median thickening of 1.00 mm at 12 months. The substrate is an ingrowing neointima (negative remodeling). This phase results in restenosis in 3% to 4% of cases (especially diabetic patients). The diameter of the self-expandable stent is increasing up to 2 years (positive remodeling) and results in a balance of remodeling from 6 to 12 months.
(3) stable phase: from the second year on without further changes in the SPL layer.
Carotid stenting: indications and patient selection
G. BIASI (Italy)
The choice of performing a carotid endarterectomy or a carotid stenting should be based on evidencebased medicine (surgery). Several ongoing trials have been designed for this. We should rather speak of MBIE (medicine based on interpretation of evidence) because we have to deal with potential biases (selection of amplitude of samples, period of observation, type and number of centers included, years before data are available).
The decision of treating a stenotic lesion with carotid stenting depends on the preoperative ultrasound evaluation of the plaque: presence of ulceration, the site of intraplaque hemorrhage, the site and extension of the plaque and especially the GSM (ICAROS study: GSM > 25: 3.09% complications; GSM < 25: 12.90% complications).
According to the author’s experience, the key points for performing carotid stenting are:
– local anesthesia
– intervention in the operation theater
– puncturing the groin
– no predilatation
– always use brain protection devices
– poststent deployment dilatation
– completion intracerebral angiography.
PTA/stent is the first option for proximal aortoiliac stenosing
disease
G. BIASI (Italy)
In the treatment of aorto-iliac stenosing disease there has been a trend toward replacing the endarterectomy by grafting, and now there is a tendency towards endovascular procedures.
Several studies have demonstrated the benefit of stenting over PTA with improvement in technical success and long-term patency rates. Indications depend on anatomical location, extension, and degree of the lesion.
In his lecture the author presented his own experience in a group of 114 procedures (claudicants: 73%; critical limb ischemia 27%) with a median abkle-brachial index (ABI) of 0.43. Angiography shows single-level disease in 26% and multilevel disease in 74% of cases.
The author performed 6 PTAs without and 108 PTAs with stenting, the technical success rate being 94.8%.
Cumulative 5-year results show a primary patency of 90%, a restenosis rate of 12%, and an occlusion rate of 7.9%.
In selected cases an endovascular approach must be the first option, with routine stenting being mandatory in order to have similar results to conventional surgery.
Developments in drug eluting coronary stenting:
is it the final step?
V. AYTEKIN (Turkey)
After the first surgical revascularization procedure in 1968, intracoronary balloon angioplasty was reported in 1977 and the second important step, stent implantation, started in 1993. The third important step is the introduction of drug eluting stents (2000) for the problem of restenosis. Restenosis is caused by elastic recoil (mechanical phase), thrombosis (thrombogenic phase), neointimal proliferation (smooth muscle cells in media and intima) and negative remodeling (remodeling phase). Treatment of the restenotic lesions with PTA, atherectomy, laser, cutting balloons, etc are not succesfull, but initial results with drug eluting stents are very promising. Drug eluting stents have other specific characteristics: larger surface area and minimal gaps between strudges when you compare them with the classic stents. Different categories of drugs have been tested: anti-inflammatory drugs (corticosteroids, gene therapy with supression of monocytes), immunosupressants (sirolimus, everolimus, taccolimus, ABT-578), antiproliferating drugs (paclitaxel, angiopeptin, 17-â-estradiol), antithrombotic agents and prohealing agents (EPC captine coating). Future directions show that biodegradable polymers and biodegradable stents may provide additional benefit. Multilayered polymers and stents with laser-cut holes may combine the effects of different kind of drugs on the same stent.
TREATMENT FOR CAROTID DISEASE
INTERNATIONAL UNION OF ANGIOLOGY AND ITALIAN SOCIETY
OF VASCULAR AND ENDOVASCULAR SURGERY
President: G. R. PISTOLESE (Italy)
Chairpersons: D. PALOMBO (Italy), C. PRATESI (Italy)
This session offered an in-depth review of carotid disease focusing on indications, preoperative studies, surgery (CEA), and endovascular (CAS) treatment.
Professor Bertoglio, from Imperia, has summarized the established indications based on the ECST and NASCET trials for symptomatic patients, and the ACAS and recently published ACST results for the asymptomatic patients. Subsequently, he reviewed controversial aspects in different areas: preoperative imaging studies, type of anesthesia, surgical technique, and monitoring use during surgery. The introduction of developments in carotid stenting adds a challenge to the decision-making process but as he said, his personal experience on 221 CEA with a mortality and major stroke rate of 2.7% and 48 CAS with a mortality and major stroke rate of 10% makes him prefer the surgerical procedure. The tendency to operate on the majority of patients (92%) by using duplex scanning and avoid angiographic preoperative studies in carotid disease was presented by professor Gossetti from Rome. He has described the use of a combination of B-Mode ultrasound and duplex scan to determine the degree of stenosis. He has pointed out the necessity to explore the value of transcranial Doppler studies to asses the intracranial circulation and imaging of cerebral tissue by means of CT scan or MR.
Professor Settembrini from Milan, presented a summary of early and late results of CEA advocating the need for intraoperative quality control in order to minimize postoperative restenosis. This control could be done by means of angiography or preferably colour Doppler. The echo color Doppler allows one to differentiate between normal, moderate (residual plaque of less than 50% or peak systolic velocity (PSV) between 125 and 180 m/s) and severe (flaps, residual stenosis of more than 50% or PSV>180 m/s) which require surgical revision.
Before presenting the indications of carotid stenting, professor Cao pointed out that the main goal of any treatment was to prevent stroke disability. He presented his experience from 2001 to 2003 on 673 CEA and 254 CAS, in which he used different type of filters and stents (Carotid Wallstent ® 89%, Aculink ® 1.5%, and Precise ® 7.5%). The complications in terms of mortality and stroke are 3.7% in CAS and 0.9% in CEA. After the introduction he divided CAS indications on anatomic grounds, such as recurrent stenosis, distal carotid lesions, or postradiation lesions, and medical indications such as severe cardiac or pulmonary disease. In order to avoid CAS complications correct patient selection is crucial, taking into consideration the presence of soft plaque, calcification, tortuosity, aortic arch disease, or advanced age in asymptomatic patients. Regarding the eternal controversy about who performs the endovascular treatment, he remarked on the need for surgical availability in case of needing to convert to open repair, which in his experience, has occurred in 10 patients.
ANEURYSMS
Chairpersons: G. DERIU (Italy), and P. GLOVICZKI (USA)
This interesting session was introduced by Professor Norgren, who gave an overview of the different causes which have been related to aneurysm formation such as atherosclerosis, degeneration of arterial wall, inflammatory process, infectious process, and genetics. His personal belief is that there is a genetic base in which different factors take part. For this reason he feels that in the not-too-distant future the treatment of AAA could be done on a genetic basis.
Prof Gloviczki presented the experience at the Mayo Clinic where repair of AAAs represents 15% of the vascular surgical practice, with an average of 250 cases repaired each year. Endovascular (EVAR) treatment is performed with increasing frequency (41% in 2003 and 51% in 2004 January to March). Minilaparotomy and laparoscopic approaches are performed in selected patients. A recent comparative analysis of 355 elective infrarenal AAA (Open repair (OR)=261 and EVAR=94) revealed that 30-day mortality was not different (OR=1.2%, EVAR=0%). Cardiac and pulmonary complications were less frequent after EVAR, although there were more high-risk patients in this group. Graft-related complications were significantly more frequent after EVAR (13% vs 4%) and primary and secondary patency rates at 1 year were lower following EVAR. According to current guidelines at Mayo Clinic, OR is recommended to all good-risk patients with nonruptured AAA, and for all unstable patients who have ruptured AAAs. EVAR is offered to high-risk patients with suitable anatomy for stent grafts. He pointed out that the need for rigorous follow-up with imaging studies, late device-related failure, late reinterventions, aneurysm rupture, and high costs of the device remain legitimate concerns of EVAR procedures. Laparoscopic and robotic techniques for AAA repair and repair using mini-laparotomy deserve further evaluation.
Prof Gerard from France presented his experience on the follow-up of abdominal aorta endoprosthesis with echocolor Doppler. The latter is a good tool to determine and analyse the type of endoleak and to determine the aortic diameter. CT scan could be used in large AAA follow-up and when an increase in aortic diameter is detected it is further investigated by duplex.
The session concluded with the presentation by Prof Riambau from Barcelona, who presented his personal experience on the endovascular treatment of thoracic aneurysms. He pointed out its feasibility, safety and efficacy, offering clear advantages compared with open surgery. Current limitations on the endograft technology should be solved with future technical developments.
LECTURES
Small abdominal aortic aneurysm repair:
should availability of endografts influence our decision?
P. KALMAN (USA)
Optimal management of a small abdominal aortic aneurysm (AAA) is controversial: early surgery or surveillance? The definition of a small aortic aneurysm has changed. Szilagy et al (1966) stated that an increased risk of rupture starts at 6 cm. The only tools available at that time were physical examination, plain X-ray, and autopsy. Darling et al (1977) performed 24 000 autopsies and found 473 aneurysms with a rupture degree of 24%. They concluded that even small aneurysms <4 cm can rupture, and should be repaired. In the 1980s and 1990s, retrospective studies showed that the risk of rupture for aneurysms <5 cm in diameter was small.
Prospective, randomized trials were available in 1998 (UK small aneurysm trial) and 2002 (ADAM study) and the conclusion of both studies was that late survival for patients with AAA <5.5 cm was the same whether patients underwent early surgery or continued surveillance.
Selection of patients for AAA repair depends on:
(1) risk of rupture (size of AAA, documented expansion, tenderness, comorbidities such as hypertension, pulmonary disease, smoking, familial predisposition)
(2) elective operative risk: operative mortality rates are falling (impact of hospital volume, surgeon volume and training)
(3) life expectancy: repair is justified if the predicted survival is good
(4) follow-up: if a patient cannot be followed, then an operation is allowed
(5) patient references: Open repair remains the gold standard, and seems highly effective in preventing rupture. The remaining questions of EVAR are: durability, reason for high reintervention rate (20% to 40%), and length of follow-up.
There is no available clinical study, but using a Markov decision analysis model, it was demonstrated that endovascular surgery does not significantly change the size threshold for elective AAA repair.
ORAL COMMUNICATIONS
Surveillance after carotid surgery: it is worthwhile?
R. PULLI (Italy)
Carotid endarterectomy has been demonstrated to be effective in stroke prevention, both in moderate and severe symptomatic carotid artery stenoses and in severe asymptomatic ones. The level of benefit of CEA in stroke prevention lies both in maintaining low perioperative mortality / neurological morbidity rates and in achieving satisfactory long-term results with a low incidence of carotid-related stroke and of significant restenosis/ occlusion. For these reasons, and also considering that contralateral carotid artery atherosclerotic involvement is a common finding in patients undergoing CEA, a postoperative surveillance program of both operated and contralateral internal carotid artery with duplex scanning has been proposed to be mandatory. However, there is no consensus regarding the real cost-effectiveness of such a surveillance program, due to the poor knowledge on incidence, causes, and natural history of carotid restenosis and of disease in the contralateral carotid artery; moreover, even if carotid duplex ultrasound is universally accepted as the method of choice in postoperative surveillance, the ideal frequency and duration of postoperative controls are still controversial. The rate of asymptomatic stent restenosis ranges between 1% and 8% in published series, with a significative correlation between severe restenosis and ipsilateral neurological events during follow-up and a risk of restenosis progression from a lower value to severe degree approaching 20% 5 years after intervention. Athersclerotic involvement of the contralateral internal carotid artery is common – nearly one third of operated patients suffer from contralateral significative ICA stenosis. The risk of contralateral stroke is higher in the presence of stenosis increase – the annual rate of stenosis progression is reported to be up to 10% for patients with >50% stenosis and 4% for those with >75% ones.
Carotid angioplasty and stenting under cerebral protection:
the dark side
M. HENRY, I. HENRY, A. POLYDOROU, A.D. POLYDOROU, E. LE BORGNE, M. HUGEL (France)
Carotid artery stenting (CAS) is a technique which is being increasingly used. The author indicated the high incidence of embolic phenomenon during CAS, the majority of them being asymptomatic. Today there is a consensus about the routine use of protection devices when CAS is performed. However, there are not, in the authors’ opinion, any protective devices which offer absolute protection. Some are difficult to use, others do not close the distal internal carotid artery correctly or complicate the procedure.
In the authors’ opinion it is necessary to know the different protection devices which are on the market. All of them have advantages and disadvantages. Depending on the case, it would be preferable to use one or another. Probably, reverse flow, described by Parodi will help reduce the ischemic events during CAS.
Renal angioplasty and stenting under distal protection:
the way for the future?
M. HENRY, I. HENRY, A. POLYDOROU, A.D. POLYDOROU, E. LE BORGNE, M. HUGEL (France)
The incidence of renal embolism after renal artery angioplasty and stenting (RAAS) is difficult to determine. In many series, renal function deteriorated after RAAS in 20% to 40% of cases. This limits the immediate benefits of this technique.
The author presented his results in 69 cases of RAAS using occlusion balloon or filters to protect renal mass. The results were very good with this technique. The renal function did not deteriorate after the procedure in any case. During the followup only two patients deteriorated.
It seems logical to think that if it is necessary to use a protection device during carotid angioplasty it will be necessary use some protection device during RAAS also to preserve renal mass. The question is: which is the best protection device?
Endolaser multidiode 980 treatment of varicose saphenous
veins: personal experience on 50 cases
G. DOMPÈ, V. PELLICCIARI, A. CHIERICHINI (Italy)
This is a descriptive study of a group of patients with varicose saphenous veins which have been treated with endolaser. The author compares his results with a group of patients who has been treated with conventional surgery, open crossectomy, and stripping. Although the author compares both groups they are not comparable for several reasons. For example, in the group with surgical treatment the saphenous vein size is bigger than in the nonsurgical group.
The results in the nonsurgical group are better than in the surgical group, but they could be better if the surgical group was operated on with a technique less aggressive than the stripping technique, such as the CHIVA technique.
Endovenous laser treatment of varicose veins compared
with traditional surgery
S. KASPAR, K. HAVLICEK (Czech Republic)
In this work the authors compare two groups of patients with varicose saphenous veins, treated with endolaser therapy alone and endolaser with open crossectomy. The results in both groups related to saphenous reflux are similar, but the authors recommend endolaser therapy to avoid the complications of conventional surgery. However, to obtain good results it is necessary to do an appropiate preoperative duplex ultrasound scan and meticulous endolaser management.
