Unmet needs in the assessment of symptoms and signs related to chronic venous disease
Bydgoszcz, Poland
ABSTRACT
Chronic venous disease (CVD) is a disorder highly prevalent among populations of Western countries and with which both general practitioners and specialists have to deal. It induces pain, causes discomfort, significantly reduces the quality of life for the affected patient, and lacks specific and consensual instruments able to adequately assess its signs and symptoms.
This article presents these needs that are still unmet in clinical practice and that relate to the tools currently available for the assessment of the therapeutic efficacy of drugs on the disease symptoms and signs. Suggestions are presented regarding new endpoints and tools to be used in further clinical trials designed to assess the effect of therapies on CVD, in particular studies with MPFF at a dose of 500 mg.
INTRODUCTION
Chronic venous disease (CVD) is common among general populations1-5 and its prevalence is likely to increase with population ageing.6 For a long time, wide differences have been observed between the reported rates of prevalence, probably due to recruitment biases and to the use of a definition of CVD that has long remained nonuniform. The Clinical, Etiological, Anatomical, Pathophysiological (CEAP) classification, published in 19957 and updated in 2004,8 provides a descriptive clinical classification that describes CVD in all its aspects, using a coding system. Recent population-based surveys based on this classification report prevalence rates of CVD of 49% in Poland,9 71% in the US,10 77% in Italy,11 85% in Scotland,12 and 90% in Germany.13
Both general practitioners and specialists have to deal with CVD. Its treatments are usually evaluated on the basis of clinical outcomes, but such evaluation does not take into account the patients’ perception of the disease and the treatment impact on their quality of life (QOL), which is significantly altered by the disease. Specific tools capable of assessing the full spectrum of CVD, its signs and symptoms, impact on QOL, and treatment effects are the key for efficient management of the disease.
This article describes those instruments that are currently available to practitioners to assess the efficacy of therapy on symptoms and signs related to CVD. It highlights also what needs to be better assessed in terms of CVD symptoms and signs, the main need being a consensus about the tools to use so as to be able to compare treatment effects between studies, and to assess which have the best specificity regarding CVD.
Suggestions are made regarding new end points and instruments of assessment for further clinical trials assessing the therapeutic effects of venoactive drugs.
ASSESSING THE EFFICACY OF TREATMENT
ON CVD-RELATED SYMPTOMS
Symptoms are defined as what patients complain of. In a world epidemiological survey (the Vein Consult Program) which is to be set up under the aegis of the Union Internationale de Phlébologie Scientific Society during the year 2009, the symptoms that will be screened for are listed in Tables I and II. Symptoms can be self-assessed, using Patient-Related Outcome or Patient- Reported Outcome (PRO) tools,14,15 or reported by physicians. In the latter situation, questioning of the patient is crucial.
There are currently, three types of instruments for the assessment of CVD-related symptoms.
I. Ascribing symptoms to CVD
In fact, symptoms are not pathognomonic but may be suggestive of CVD, particularly if they are exacerbated by heat or dependent on the time of day, and relieved by leg rest and/or elevation. Simple questions can be asked by the practitioners to ascribe symptoms to CVD (Table II).
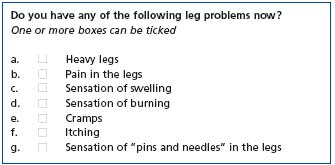
Table I. Symptoms screened for in the future VEIN CONSULT PROGRAM to be set up under the aegis of the scientific society UIP (Union Internationale de Phlébologie)
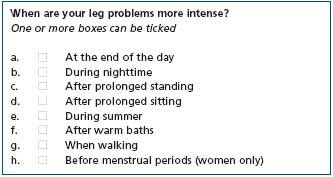
Table II. Ascription of symptoms to CVD, as screened for in the VEIN CONSULT PROGRAM to be set up under the aegis of the UIP (Union Internationale de Phlébologie)
The scoring system by Carpentier,16 presented in Table III, is a patient-administered diagnostic tool designed to ascribe leg symptoms to CVD. This system “might also help predict the usefulness of treatment in patients with CVD seeking medical help for their symptoms”. It combines four criteria: 1) sensation of heavy or swollen legs, 2) associated sensation of itching, restless legs, or phlebalgia, 3) sensation worsened by a hot environment or improved by a cold environment, and 4) sensation not worsened by walking. Scores range from 0 to 4. With a threshold level of >3, this scoring system had a high specificity (0.95) and a fair sensitivity (0.75) for CVD (Table III).
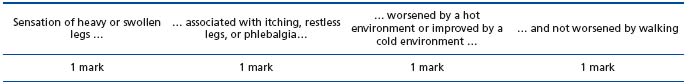
Score ≥3: symptoms are of venous origin Score <1: symptoms are not of venous origin
Table III. The scoring system for venous symptoms. Adapted from Carpentier PH et al16
The VEINES-Sym, developed by DL Lamping,17 is a 10- item self-administered questionnaire that includes questions on the frequency of 9 CVD-related symptoms (heavy legs, aching legs, swelling, night cramps, heat or burning sensation, restless legs, throbbing, itching, and tingling sensation), and the intensity of leg pain. The scores range from 0 to 10, with higher values indicating better outcomes.
The Phleboscore® developed by P. Blanchemaison18 is an 11-item self-administered questionnaire which helps predict the risk of developing CVD. It includes questions about risk factors (gender, age, sedentary life, weight excess, number of pregnancies, working conditions, family history, sporting activities), as well as questions about the frequency of symptoms (heavy legs, sensation of swelling) and the circumstances in which symptoms worsen (heat, birth pill, long-haul travel). The scores range from 0 to 31. A score >12 identifies patients at risk of CVD, while a score >23 pinpoints a need for venous investigation.
II. Tools adapted to patient-reported outcome
The tools used to assess PRO consist mainly of quality of life (QOL) scales that may be either generic or diseasespecific.15
The 13-item Aberdeen Varicose Veins Questionnaire19 (AVVQ) is a disease-specific approach to measuring the patient’s perception of outcome for varicose veins. This questionnaire addresses all features of varicose vein disease: physical symptoms and social issues, pain, ankle edema, ulcers, compression therapy use, and the effect of varicose veins on daily activities, in addition to the effect of varicose veins from a cosmetic standpoint. In studies conducted to test the validity and the reliability of this instrument, the Aberdeen Questionnaire was shown to have good levels of validity and test-retest reliability and to be the most responsive to changes in health status.19,20 A recent Dutch study conducted to test the translated version of the questionnaire obtained interesting results with very satisfactory levels of feasibility (0.6% of missing answers and 0.2% of non-unique answers), internal consistency (Cronbach’s alpha =0.76 indicating a high level of concordance between the questions); test-retest reliability (Spearman’s r=0.87, showing a significant strong association between test and retest scores), and discriminative validity since AVVQ score was able to differentiate between subgroups of patients with different severity of venous disease according to the CEAP classification (Mann-Whitney U test, P<0.01).20 The 20-item ChronIc Venous disease quality of lIfe Questionnaire (CIVIQ) gives a global score, plus a score for each of the 4 areas in which QOL is likely to be affected: physical, psychological, social, and pain. CIVIQ has been extensively used, as reported in numerous studies22-41 among which some included large samples of patients.22-26 Launois initially developed with rigorous methods a practical, scientifically rigorous patientreported outcome measure CIVIQ in a clinical trial of 934 patients and an epidemiologic survey of 26 681 patients.22 Lurie used it to compare two surgical procedures (stripping vs Closure“).24 Jantet tested it in the RELIEF study (Reflux assEssment and quaLity of life improvEment with micronized Flavonoids), in 3948 C0 to C4 patients.23 Guex et al used the CIVIQ questionnaire in a study aimed at describing the health status of 1045 female patients suffering from CVD, and to assess the care impact,25 and Neglén used it before and after intervention, along with the CEAP classification in an 8-year study on venous outflow stenting performed in 982 chronic non-malignant obstructive lesions of the femoroiliocaval vein.26 CIVIQ has been extensively used in many CVD-related conditions.27-42 CIVIQ is validated in 13 languages including Canadian English, English for Singapore, British English, American English, French Canadian, French for France, German for Austria, Greek, Italian, Polish, Portuguese for Portugal, and Spanish for Spain and for the USA.
The Charing Cross Venous Ulceration Questionnaire was developed to provide a valid QOL measure for patients with venous ulcers and to assess the effects of the many treatments available for venous ulcers.15,42 A study aimed at testing the validity of this questionnaire showed a high correlation with all eight domains of the gold standard SF-36 general health measure (r>0.55, P<0.001). The factor analysis identified four important health factors: social function, domestic activities, cosmesis, and emotional status. This study also demonstrated its good reliability (internal consistency: Cronbach’s alpha=0.93), test-retest reliability (r=0.84), and good responsiveness (significant reduction in the score on the ulcer question – naire as ulcers healed at 6 and 11 weeks; P<0.05).42
The VEnous INsufficiency Epidemiological and Economic Study (VEINES), an international, prospective cohort study conducted in 166 general practices and 116 specialist clinics in Belgium, France, Italy, and Canada, has developed the VEINES-QOL/Sym to evaluate QOL and symptoms across the range of conditions (eg, telangiectasias, varicose veins, edema, skin changes, leg ulcers) in lower limb CVD.17 It consists of 35 items distributed in 2 categories to generate 2 summary scores: the VEINES-QOL questionnaire comprises 25 items that estimate the effect of disease on QOL, and the 10-item VEINES symptom questionnaire (VEINES-Sym) measures symptoms. The focus of this instrument is on physical disconfort as opposed to psychological and social aspects. This measure of QOL and symptoms is available in four languages (English, French for Belgium and France, Italian, and Canadian French). It has been used in only 3 studies of Kahn et al to assess the health-related QOL of large samples of CVD patients with and without prior venous thromboembolism,43 and patients with deep venous thrombosis.44-46
All these four disease-specific assessment tools were used in conjunction with the 36-item Medical Outcome Study Health Survey Short Form (MOS SF-36), a generic health-related QOL instrument of which the validity, reproducibility, and responsiveness to changes over time have been well demonstrated.47,48 It is the most widely used and validated generic QOL instrument, whatever the medical field. The SF-36 has been developed over time with questions in the following two categories: physical health (assessed as the patient’s level of functioning) and mental health (assessed as an indication of well-being). These two groups have been broken down into 8 areas that include evaluation of physical and social functioning, role limitations due to physical or emotional problems, mental health, pain, vitality, and health perception. When complete, the survey generates a score ranging from 0 to 100, with higher scores indicating best general health perception. The SF-36 has proven to be a good fit for generic QOL assessment in patients with CVD.20,49-52
III. Tools available to physicians to measure symptoms
Among the various instruments that are available to physicians to measure symptoms such as pain, assessing the consumption of analgesic drugs may be valuable but only if assessed by the practitioner. Such a criterion is unreliable when assessed by the outpatient and reported during history taking only: no instrument has been validated for the measurement of outpatients’ consumption of analgesic medication.53,54
Practitioners may use visual analogue scales (VAS) – such as the 10-cm VAS – for measuring CVD-related pain.37 This type of scale provides patients with easy and rapid way to express the intensity of their pain and has been validated55-57 and used in numerous applications. Regarding CVD, since pain related to this disease is mostly below 4 cm, the adequacy of this measurement may be questioned; the amplitude of pain may not be large enough in CVD to assess the therapeutic effects using such means.
The numerical rating scales are usually graded from 0 to 5, or 0 to 4, or 0 to 10. These scales that measure pain during the medical visit and in a retrospective manner58 are often used in the evaluation of treatment in CVD.59-61
ASSESSING THE EFFICACY OF TREATMENT
ON CVD-RELATED SIGNS
Disease-related signs are visible or palpable; they are usually reported by the physician, not by the patient.
I. The CEAP classification, a universally adopted classification of CVD signs
The CEAP classification7,8 has become a universal method of classification of venous disease. This classification can be used by the clinician in keeping office records of diagnostic information. Adoption of this single classification worldwide based on correct diagnosis has facilitated meaningful communication about the disease and served as a basis for a more scientific analysis of management alternatives.
II. The adjuncts to the CEAP as tools for physicians
Some limitation exists regarding the use of the CEAP classification in the evaluation of patients with CVD. The CEAP classification is descriptive, but cannot be used for venous severity scoring because many of its components are static and do not change in response to treatment. A disease severity scoring scheme needs to be quantifiable, with gradable elements that can change in response to treatment.62 Therefore, a venous severity scoring system (VSSS) has been proposed by the American Venous Forum (AVF) ad hoc committee on outcomes, consisting of three scores: the Venous Clinical Severity Score (VCSS), which includes 10 hallmarks of venous disease that are likely to show the greatest change in response to therapy and are scored on a scale of severity graded 0-3, and the Venous Segmental Disease Score (VSDS), which uses the anatomic and pathophysiological classifications in the CEAP system to generate a grade based on venous reflux or obstruction, and the Venous Disability Score (VDS), which refers to ability to work with or without a “support device”.62
Among the various comments and recommendations presented by B. Eklöf63 at the San Diego Consensus meeting of 2003 regarding the use of these tools (the CEAP classification and the VSSS), the following points for which consensus was reached should are worthy of particular attention:
• The CEAP classification is a descriptive instrument to categorize patients into different groups of severity of CVD;
• The VSSS is a useful complement to the CEAP classification, and should be used for research;
• The use of all CEAP components should be encouraged. However, use of only the clinical component (C) at the time of the initial evaluation is appropriate, and the E, A, and P components can be added as the diagnostic evaluation progresses.
Although reportedly easy to use, in the view of angiologists the VSSS is more likely to be of value in severe CVD.64 The descriptive CEAP and the VSSS, particularly the VCSS, are valid but imperfect instruments for evaluation of the early stages of CVD and treatment outcome. It seems that the time has come to revise the VCSS to allow proper reporting of common patient symptoms.
Another element appears to be lacking in the evaluation of CVD patients based on the CEAP and VSSS systems only: the patient’s perception of anxiety or psychological apprehension.65 A study that used both systems to evaluate venous disease in patients undergoing primary ambulatory surgery for varicose veins noted that despite careful patient selection, psychological distress could not be prevented or predicted; 11% of the patients experienced distress and anxiety, and a significant difference was observed regarding the complication rate in the recovery room (p=0.04) between patients with or without anxiety.65 Thus, taking emotional factors into consideration in outpatient surgical practice appears to be essential.
III. The assessment of treatment efficacy on edema and venous ulcer
Some tools assess leg edema by measuring either leg circumference or volume (volumetry).66 Leg circumference can be assessed using a tape measure or the Leg-O-Meter, an inexpensive and reproducible method validated in the RELIEF study23 and the VEINES study.68 Its limitation is that the circumference is not always correlated with leg volume measurement.66 The leg volume can be assessed simply and reproducibly by water displacement volumetry, optoelectronic methods, CT scanning, MRI, and dual X-ray absorptiometry. Assessing the volume is preferable, but the methods of assessment have not all been validated and lack sensitivity in CVD.
Numerous techniques are available for the assessment of venous ulcer, ranging from the simple use of tracings to more sophisticated methods requiring cameras, videos, and computers.68 The parameters most frequently used to measure a wound are the length of the principal axes (length and width of the wound), the projected surface area, and the perimeter.68
ASSESSMENT OF TREATMENT EFFICACY IN CVD:
A NEED FOR CONSENSUS ABOUT TOOLS TO BE USED
I. Regarding the tools used to assess symptoms
This is the most problematic issue since symptoms are subjective by definition. Moreover, pain in CVD is diffuse, unpleasant, with a high negative impact on QOL. This is seen in the many symptoms reported (sensation of swelling, of burning, of leg heaviness, etc.) and in the fact that the wording used to describe the complaints is vague. This may be due to the underlying mechanisms of venous pain.69
In general, what is still needed is:
• the validation of Carpentier’s scoring system (Table III);16
• the inclusion of questions regarding the circumstances of appearance of symptoms as part of the usual patient questioning; this will be done (with a more comprehensive Q) in the VEIN-Consult programme (Tables I and II);
• the Phleboscore18 is an interesting way of warning patients about the risk factors, but it has never been validated;
• it is acknowledged that both generic and specific QOL scales should be used: the generic SF-12 (or 36) is a validated tool that could be adopted, while for specific scales, the CIVIQ that has been extensively used in CVD is the most often used scale up to now, with 13 languages validated;15
• quantitative and semi-quantitative scales were included in the comprehensive document of the ANAES,53 but much remains to be done to choose the most adapted scale. The VAS has been the most extensively validated tool in different diseases, but rare are the CVD patients whose scores exceed 5 cm.
II. Tools used to assess signs
The CEAP has been a great leap in the classification of venous signs. It allows the description of patients at the entry in a study, and the comparison of patients’ profiles between studies. Despite the progress the CEAP represents, it has weaknesses, such as:
• a certain difficulty in distinguishing between C1 and C2 patients as shown by the epidemiological studies in which the prevalence of the disease at these stages varies greatly from one paper to another;
• it is not clearly stated in the CEAP whether the edema of C3 patients is a permanent edema (as a preliminary stage towards skin changes and CVD complications) or if a reversible edema that occurs at the end of the day and disappears after rest can be included in the C3 stage.
• Although corona phlebectatica (corona) is a clinical sign associated with chronic venous disease, it is not yet included in the CEAP classification. Corona is defined as fan-shaped intradermal telangiectasias in the medial and sometimes lateral portions of the ankle and foot. It has been shown that corona strongly correlates with the clinical severity and hemodynamic disturbances of the disease.70 The inclusion of corona in the C3 class should probably improve the reliability of the CEAP clinical classes.
III. Methods of assessment
In addition to the limitations related to the methods of assessment of leg edema (see above), there is a lack of consensus regarding the definition of wound healing in assessing the treatment of leg ulcers: should we consider healing as a simple wound re-epithelization or as skin re-epithelization + return to daily activities?71,72 Standards for the measurement of wound healing are needed.
USING CURRENT AND NEW TOOLS IN FURTHER
CLINICAL TRIALS ASSESSING THE EFFECTS OF
MPFF at a dose of 500 mg ON SYMPTOMS AND SIGNS
One of the main objectives of any new clinical trial with MPFF at a dose of 500 mg is to assess the benefits of this treatment at the early stages of CVD: C0, C1 and C3. Taking into account the following suggestions should improve the assessment of treatment outcome.
• Quantifying symptoms:
– which symptoms? The most frequently encountered ones such as pain, heaviness, and sensation of swelling, separately;
– use of rating scales such as VAS, and simple verbal scales + assessment of the influence of symptoms on QOL using the SF-12 or CIVIQ questionnaire.
• New approach to symptom assessment:
– Since pain of venous origin is often multifaceted and is frequently associated with other unpleasant sensations like swelling, heaviness, burning, etc., which are often difficult to describe and usually expressed with a vague terminology, it is likely that such unpleasantness belongs to the range of symptoms of nociception. Therefore, the use of a composite score that would include pain, heaviness, and sensation of swelling would be desirable;
– Given the high negative impact unpleasantness and symptoms may have on patients’ daily lives, and the fear for the future that patients express when they report their anxiety, the use of a complementary psychological screening tool to measure the improvement of CVD-related anxiety disorders would be an interesting complement to the QOL scales. In this view, the Hospital Anxiety and Depression Scale (HADS) that has been extensively validated in many illnesses and is used in routine care in many countries73 could be helpful;
– both the CIVIQ and the HADS are likely to provide the best answer to the difficulty of assessing subjective symptoms.
• Reporting signs:
– telangiectasias: educating primary care investigators using slides and clear-cut definitions;
– edema: by distinguishing edema of venous origin from nonvenous edema (pitting edema);74
– edema assessment by associating leg circumference measures and volume measurement as in the method of the truncated cone.75
CONCLUSION
As a common disease with which both general practitioners and specialist doctors have to deal, CVD and outcomes of CVD treatment should be better assessed, especially at early stages of the disease. As stated by the AVF, “the cornerstone for management of CVD is a proper diagnosis and accurate classification of the underlying venous problem, which creates the base for correctly directed treatment”. Taking emotional factors into consideration in the patient’s management has been shown to be essential also, given the significant impact of this disease on the patient’s QOL. Numerous instruments and tools are available to practitioners both to assess signs and symptoms of the disease and to assess the patients’ perception of their health-related QOL, but none is fully satisfactory and some remain to be validated. Much is yet to be done to improve the management of this disease by a more proper use of the existing diagnostic and assessment means and by taking account of the full spectrum of the disease including its impact on the patient’s QOL.
REFERENCES
2. Evans CJ, Fowkes FGR, Rucley CV, Lee AJ. Prevalence of varicose veins and chronic venous insufficiency in men and women in the general population: Edinburgh Vein Study. J Epidemiol Community Health 1999;53:149-153.
3. Fowkes FGR, Evans CJ, Lee AJ. Prevalence and risk factors of chronic venous insufficiency. Angiology 2001;52(suppl 1): S5-S15.
4. McLafferty RB, Lohr JM, Caprini JA, Passman MA, Padberg FT, Rooke TW, Bush RL, Zakaria AA, et al. Results of the national pilot screening program for venous disease by the American Venous Forum. J Vasc Surg 2007;45(1):142-148.
5. Schoevaerdts JC, Staelens I. Programme for detecting chronic venous insufficiency in Belgium. Phlebology 2007;22(4):171-178.
6. Heit JA, Rooke TW, Silverstein MD, Mohr DN, Lohse CM, Petterson TM, et al. Trends in the incidence of venous stasis syndrome and venous ulcer: a 25-year population-based survey. J Vasc Surg 2001;33:1022-1027.
7. Porter JM, Moneta GL. International Consensus Committee on Chronic Venous Disease: Reporting standards on venous disease: an update. J Vasc Surg 1995;21:635-645.
8. Eklöf B, Rutherford RB, Bergan JJ, et al. Revision of the CEAP classification for chronic venous disorders: consensus statement. J Vasc Surg 2004;40:1248-1252.
9. Jawien A, Grzela T, Ochwat A. Prevalence of chronic venous insufficiency (CVI) in men and women in Poland: multicenter cross-sectional study in 40 095 patients. Phlebology 2003;18:110-122.
10. McLafferty RB, Passman MA, Caprini JA, Rooke TW, Markwell SA, Lohr JM, Meissner MH, Eklöf BG, et al. Increasing awareness about venous disease: The American Venous Forum expands the National Venous Screening Program. J Vasc Surg 2008;48(2):394-9.
11. Chiesa R, Marone EM, Limoni C, Volonte M, Schaefer E, Petrini O. Chronic venous insufficiency in Italy: the 24-cities cohort study. Eur J Vasc Endovasc Surg 2005;30 :422-429.
12. Evans CJ, Fowkes FGR, Ruckley CV, Lee AJ. Prevalence of varicose veins and chronic venous insufficiency in men and women in the general population. Edinburgh Vein Study. J Epidemiol Community Health 1999;53:149-153.
13. Rabe E, Pannier-Fischer F, Bromen K, et al. Bonner Venenstudie der Deutschen Gesellschaft für Phlebologie. Phlebologie 2003;32:1-14.
14. Acquadro C, Berzon R, Dubois D, Kline Leidy N, Marquis P, Revicki D, Rothman M; for the PRO Harmonization Group. Incorporating the Patient’s Perspective into Drug Development and Communication: An Ad Hoc Task Force Report on the Patient-Reported Outcomes (PRO) Harmonization Group Meeting at the Food and Drug Administration, Feb 16, 2001. Value in Health 2003;5:522-531.
15. Vasquez MA, Munschauer CE. Venous Clinical Severity Score and Quality-of- Life Assessment Tools: Application to Vein Practice. Phlebology 2008;23(6):259-275.
16. Carpentier PH, Poulain C, Fabry R, et al. Ascribing leg symptoms to chronic venous disorders: the construction of a diagnostic score. J Vasc Surg 2007;46:991-996.
17. Lamping DL, Schroter S, Kurz X, Kahn SR, Abenhaim L. Evaluation of outcomes in chronic venous disorders of the leg: Development of a scientifically rigorous, patient-reported measure of symptoms and quality of life. J Vasc Surg 2003;37:410-419.
18. Blanchemaison P. Evaluation pratique du risque veineux: le Phléboscore®. Act Vasc Int 2000;81:12-16.
19. Garratt AM, Ruta DA, Abdalla MI, Russell IT. Responsiveness of the SF-36 and a condition-specific measure of health for patients with varicose veins. Qual Life Res 1996;5(2):223-234.
20. Smith JJ, Garratt AM, Guest M, Greenhalgh RM, Davies AH. Evaluating and improving healthrelated quality of life in patients with varicose veins. J Vasc Surg 1999;30(4):710-719.
21. Klem TM, Sybrandy JE, Wittens CH, Bot ML. Reliability and Validity of the Dutch Translated Aberdeen Varicose Vein Questionnaire. Eur J Vasc Endovasc Surg 2008; december (Epub).
22. Launois R, Reboul-Marty J, Henry B. Construction and validation of a quality of life questionnaire in chronic lower limb venous insufficiency (CIVIQ). Qual Life Res 1996;5(6):539- 554.
23. Jantet G. Chronic venous insufficiency: worldwide results of the RELIEF study. Reflux assEssment and quaLity of lIfe improvEment with micronized Flavonoids. Angiology javascript:AL_get(this, ‘jour’, ‘Angiology.’);2002;53(3):245-256.
24. Lurie F, Creton D, Eklof B, Kabnick LS, Kistner RL, Pichot O, Sessa C, Schuller- Petrovic S. Prospective randomised study of endovenous radiofrequency obliteration (closure) versus ligation and vein stripping (EVOLVeS): twoyear follow-up. Eur J Vasc Endovasc Surg 2005;29(1):67-73.
25. Guex JJ, Myon E, Didier L, Nguyen Le C, Taieb C. Chronic venous disease: health status of a population and care impact on this health status through quality of life questionnaires. Int Angiol 2005; 24(3):258-264.
26. Neglén P, Hollis KC, Olivier J, Raju S. Stenting of the venous outflow in chronic venous disease: long-term stent-related outcome, clinical, and hemodynamic result. J Vasc Surg 2007;46(5):979-990.
27. Kalteis M, Berger I, Messie-Werndl S, Pistrich R, Schimetta W, Pölz W, Hieller F. High ligation combined with stripping and endovenous laser ablation of the great saphenous vein: early results of a randomized controlled study. J Vasc Surg 2008;47(4):822-829.
28. Pokrovsky AV, Saveljev VS, Kirienko AI, Bogachev VY, Zolotukhin IA, Sapelkin SV, Shvalb PG, Zhukov BN, Vozlubleny SI, Sabelnikov VV, Voskanian YE, Katelnitsky II, Burleva EP, Tolstikhin VY. Surgical correction of varicose vein disease under micronized diosmin protection (results of the Russian multicenter controlled trial DEFANS). Angiol Sosud Khir 2007;13(2):47-55.
29. Martínez-Zapata MJ, Moreno RM, Gich I, Urrútia G, Bonfill X, Chronic Venous Insufficiency Study Group. A randomized, double-blind multicentre clinical trial comparing the efficacy of calcium dobesilate with placebo in the treatment of chronic venous disease. Eur J Vasc Endovasc Surg 2008;35(3):358-365.
30. Gavrilenko AV, Sandrikov VA, Vakhratian PE, Dutikova EF, Fateeva IE. Role of valvular insufficiency of the femoral vein in clinical course and relapse of lower limb varicosity. Angiol Sosud Khir 2006;12(3):61-66.
31. Lorenz D, Gäbel W, Redtenbacher M, Weissenhofer W, Minzlaff M, Stengel D. Randomized clinical trial comparing bipolar coagulating and standard great saphenous stripping for symptomatic varicose veins. Br J Surg 2007;94(4):434-440.
32. Intsertov MA. Assessment of the efficacy of surgical management of lower limb varicosity from the viewpoint of patients’ quality of life as dependent on their psychological status. Angiol Sosud Khir 2005;11(3):60-63.
33. Veverková L, Kalac J, Jedlicka V, Wechsler J. Analysis of surgical procedures on the vena saphena magna in the Czech Republic and an effect of Detralex during its stripping. Rozhl Chir 2005;84(8):410-412, 414- 416.
34. Lozano FS, Launois R; Reflux Assessment and Quality of Life Improvement with Micronized Flavonoids (RELIEF) Spanish group. Quality of life (Spain and France): validation of the chronic venous insufficiency questionnaire (CIVIQ). Methods Find Exp Clin Pharmacol 2002;24(7):425-9.
35. Chassany O, Le-Jeunne P, Duracinsky M, Schwalm MS, Mathieu M. Discrepancies between patientreported outcomes and clinician-reported outcomes in chronic venous disease, irritable bowel syndrome, and peripheral arterial occlusive disease. Value Health 2006;9(1):39-46.
36. Andreozzi GM, Cordova R, Scomparin MA, Martini R, D’Eri A, Andreozzi F; Quality of Life Working Group on Vascular Medicine of SIAPAV. Effects of elastic stocking on quality of life of patients with chronic venous insufficiency. An Italian pilot study on Triveneto Region. Int Angiol 2005;24(4):325-329.
37. Ramelet AA. MPFF at a dose of 500 mg: symptoms and edema clinical update. Angiology 2005;56 Suppl 1:S25-32.
38. Andreozzi GM, Cordova RM, Scomparin A, Martini R, D’Eri A, Andreozzi F; Quality of Life Working Group on Vascular Medicine of SIAPAV. Quality of life in chronic venous insufficiency. An Italian pilot study of the Triveneto Region. Int Angiol 2005;24(3):272-7.
39. Przybylska M, Majewski W. Varicose veins of lower limbs is a very common medical problem in developed countries and also in Poland. Pol Merkur Lekarski 2005;18(108):657-662.
40. Erevnidou K, Launois R, Katsamouris A, Lionis C. Translation and validation of a quality of life questionnaire for chronic lower limb venous insufficiency into greek. Int Angiol 2004;23(4):394-399.
41. Vayssairat M, Ziani E, Houot B. Placebo controlled efficacy of class 1 elastic stockings in chronic venous insufficiency of the lower limbs. J Mal Vasc 2000;25(4):256-262.
42. Smith JJ, Guest MG, Greenhalgh RM, Davies AH. Measuring the quality of life in patients with venous ulcers. J Vasc Surg 2000; 1(4):642-649.
43. Kahn SR, M’Lan CE, Lamping DL, Kurz X, Bérard A, Abenhaim L; The Veines Study Group. The influence of venous thromboembolism on quality of life and severity of chronic venous disease. J Thromb Haemost 2004;2(12):2146-2151.
44. Kahn SR, Ducruet T, Lamping DL, Arsenault L, Miron MJ, Roussin A, Desmarais S, et al. Prospective evaluation of health-related quality of life in patients with deep venous thrombosis. Arch Intern Med 2005;165(10):1173-1178.
45. Kahn SR, Lamping DL, Ducruet T, Arsenault L, Miron MJ, Roussin A, Desmarais S, et al. VETO Study investigators: VEINES-QOL/Sym questionnaire was a reliable and valid disease-specific quality of life measure for deep venous thrombosis. J Clin Epidemiol 2006;59(10):1049-1056.
46. Kahn SR, Shbaklo H, Lamping DL, Holcroft CA, Shrier I, Miron MJ, Roussin A, et al. Determinants of health-related quality of life during the 2 years following deep vein thrombosis. J Thromb Haemost 2008;6(7):1105-1112.
47. Stewart AL, Greenfield S, Hays RD, et al. Functional status and well-being of patients with chronic conditions. JAMA 1989;262:907-913.
48. Ware JE, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36). I. Conceptual framework and item selection. Med Care 1992;30: 473- 483.
49. Franks PJ, McCullagh L, Moffatt CJ. Assessing quality of life in patients with chronic leg ulceration using the Medical Outcomes Short Form-36 questionnaire. Ostomy Wound Manage 2003;49(2):26-37.
50. Garratt AM, Ruta DA, Abdalla MI, Buckingham JK, Russell IT. The SF36 health survey questionnaire: an outcome measure suitable for routine use within the NHS. BMJ 1993;306(6890):1440-1444.
51. Ruta DA, Abdalla MI, Garratt AM, Coutts A, Russell IT. SF 36 health survey questionnaire: I. Reliability in two patient based studies. Qual Health Care 1994;3(4):180-185.
52. Garratt AM, Ruta DA, Abdalla MI, Russell IT. SF 36 health survey questionnaire. II. Responsiveness to changes in health status in four common clinical conditions. Qual Health Care 1994;3(4):186-192.
53. ANAES. Evaluation et suivi de la douleur chronique chez l’adulte en médecine ambulatoire. February 1999. available on www.unaformec.org
54. Boureau F. Les méthodes d’évaluation des analgésiques chez l’homme. In : Giroud JP, Mathé G, Meyniel G (eds). Pharmacologie clinique. Bases de la thérapeutique. Paris : Expansion Scientifique Française, 1988:801-12.
55. Ogon M, Krismer M, Söllner W, Kantner-Rumplmair W, Lampe A. Chronic low back pain measurement with visual analogue scales in different settings. Pain 1996;64:139-147.
56. Price DD, Bush FM, Long S, Harkins SW. A comparison of pain measurement characteristics of mechanical visual analogue and simple numerical rating scales. Pain 1994;56:217-226.
57. Jensen MP, Karoly P. Self-report scales and procedures for assessing pain in adults. In: Turk DC, Melzack R, eds. Handbook of pain assessment. New York: The Guilford Press; 1992. p. 135- 151.
58. Jensen MP, Turner LR, Turner JA, Romano JM. The use of multiple-item scales for pain intensity measurement in chronic pain patients. Pain 1996;67:35-40.
59. Gonçalves ML, de Gouveia Santos VL, de Mattos Pimenta CA, Suzuki E, Komegae KM. Pain in chronic leg ulcers. J Wound Ostomy Continence Nurs 2004;31(5):275-283.
60. Petruzzellis V, Troccoli T, Candiani C, Guarisco R, Lospalluti M, Belcaro G, Dugall M. Oxerutins (Venoruton): efficacy in chronic venous insufficiency:a double-blind, randomized, controlled study. Angiology 2002;53(3):257-263.
61. Carpentier PH, Mathieu M. Evaluation of clinical efficacy of a venotonic drug: lessons of a therapeutic trial with hemisynthesis diosmin in “heavy legs syndrome”. J Mal Vasc 1998;23(2):106- 112.
62. Rutherford RB, Padberg FT Jr, Comerota AJ, Kistner RL, Meissner MH, Moneta GL; American Venous Forum’s Ad Hoc Committee on Venous Outcomes Assessment. Venous severity scoring: An adjunct to venous outcome assessment. J Vasc Surg 2000;31:1307- 1312.
63. Eklöf B. The CEAP Classification: Update Based on Recent Pacific and Caribbean Consensus Meetings. San Diego Consensus Meeting, 2003. Available on http://www.phlebology.org/meetings/ 2003abstracts.html
64. Perrin M, Dedieu F, Jessent V, Blanc MP. Evaluation of the new severity scoring system in chronic venous disease of the lower limbs: an observational study conducted by French angiologists. Phlebolymphology 2006;13:6-16.
65. Scavée V, Pirlet I, Terryn E, Nardella E, Michel I, Haxhe JP. Varicose veins in ambulatory surgery: patients’ perception. Acta Chir Belg 2007;107(2):166-172.
66. Perrin M, Guex JJ. Edema and leg volume: methods of assessment. Angiology 2000;51:9-12.
67. Berard A, Kurz X, Zucharelli F, et al and the VEINES group. Reliability study of the Leg-O-Meter, an improved tape measure device, in patients with chronic venous insufficiency of the leg. Angiology 1998;49:169-173.
68. Humbert P, Meaune S, Gharbi T. Wound healing assessment. Phlebolymphology 2004;47: 312-319.
69. Danziger N. Pathophysiology of pain in venous disease. Phlebolymphology 2008;15:107-114.
70. Uhl JF, Cornu-Thénard A, Carpentier PH, Widmer MT, Partsch H,Antignani PL. Clinical and hemodynamic significance of corona phlebectatica in chronic venous disorders. J Vasc Surg 2005; 42:1163-1168.
71. Lazarus GS, Cooper DM, Knighton DR et al. Definitions and guidelines for assessment of wounds and evaluation of healing. Arch Dermatol 1994;130:489-493.
72. Gorin DR, LaMorte W W, Barry M, Scott T, Menzoian JO. Is complete wound healing a valid endpoint for clinical trials of venous stasis ulcer treatment. Vasc Surg 1997;31:163-169.
73. Herrmann C. International experiences with the Hospital Anxiety and Depression Scale. A review of validation data and clinical results. J Psychosom Res 1997;42:17-41.
74. Priollet P. Venous edema of the lower limb. Phlebolymphology 2006;13:181- 185.
75. Labs KH, Degischer s, Gamba G, Jaeger KA. Effectiveness and safety of calcium dobesilate in treating chronic venous insufficiency: randomized, doubleblind, placebo-controlled trial. Phlebology 2004;19:123-130.
