Update on treatment methods for telangiectasia
University of Health Sciences, Bursa Yuksek
Ihtisas Training and Research Hospital,
Department of Cardiovascular Surgery,
Turkey
Abstract
Telangiectasias make up a heterogeneous group of diseases that can affect various parts of the body in humans. Although generally limited to the face, telangiectasia can cover different parts of the body in various collagen tissue diseases. The appropriate treatment options for telangiectasias are sclerotherapy, laser therapy, thermocoagulation, and microphlebectomy. The purpose of sclerotherapy is to cause endothelial damage by injecting a sclerosing agent into the vascular bed. Agents such as polidocanol, sodium tetradecyl sulfate, hypertonic saline, and glycerin are used for this treatment. Intense pulsed light is a noncoherent light source and is an important laser in the treatment of telangiectasia with wavelengths in the 500-nm to 1200-nm range. With thermocoagulation, also known as the radiofrequency energy method, high-frequency waves (4 MHz) are transmitted from the skin to the venous structures via a thin needle, and thermal ablation is provided. In microphlebectomy, venous networks are destroyed by needle puncture through a tiny skin incision. Scarring rarely occurs because the skin incisions are made very small. The efficacy of each of these treatment options seems similar. Choosing the treatment method most suitable for each patient will increase the success rates.
Introduction
Telangiectasias make up a heterogeneous group of diseases that can affect various parts of the body in humans. Although generally limited to the face, they can cover different parts of the body in various collagen tissue diseases. The telangiectasias we have studied usually occur as the result of chronic venous diseases of the lower extremities. These structures occur due to intradermal dilatation of the subpapillary venous plexus, where the vein wall thickens asymmetrically and contains collagen and muscular structures. More rarely, they may contain elastic fibers.1 The prevalence of telangiectasias in the general population varies between 60% and 86%, and varicose veins are also present in some individuals.2 Although the prominent complaints in these patients are related to cosmetic concerns, complaints such as pain and burning are also reported.3 The appropriate treatment options for these patients are sclerotherapy, laser therapy, thermocoagulation, and microphlebectomy. Here, we present the clinical results of various treatments for telangiectasias.
Sclerotherapy
The purpose of this application is to cause endothelial damage by injecting a sclerosing agent into the vascular bed. Agents such as polidocanol (POL), sodiumtetradecyl sulfate (STS), hypertonic saline, and glycerin are used for this treatment. Among these, POL is widely used today in different ratios and applied as foam or directly as a liquid. These foam and liquid treatments of POL were compared in a meta-analysis by Bi et al, which includes 8 randomized controlled trials and analyzes the efficacy and complications of these 2 methods. In this meta-analysis, the primary outcome was treatment efficiency, whereas secondary outcomes were postprocedural complications. The efficacy rate was analyzed in 7 studies involving 771 patients, and foam sclerotherapy was found to be more effective (odds ratio [OR], 5.64; P<0.0001; 95% confidence interval [CI], 3.93–8.10). Postprocedural pain was evaluated in an analysis of 1001 patients in 7 studies, and the pain was significantly more common in patients who received foam (OR, 1.52; P=0.030; 95% CI, 1.04–2.21). In an analysis that included 959 patients in a total of 7 studies, no significant difference was found in terms of postprocedural local inflammation rates (P=0.896; 95% CI, -0.03 to 0.03). Postoperative thrombophlebitis evaluation in 709 patients in 5 studies in total showed no significant difference between groups (P=0.900; 95% CI, -0.02 to 0.02). Finally, a hyperpigmentation assessment was performed for 871 patients, which included 6 studies, and no significant difference was found between groups (P=0.336; 95% CI, -0.05 to 0.14). In this current meta-analysis, the authors emphasized that although foam sclerotherapy causes complications more frequently, its effectiveness was quite high.4
Studies comparing the efficacy of different sclerosing agents are found in the literature. In a prospective randomized study by Bukina et al, hypertonic glucose (HG) and STS were compared (81 patients in the STS group, 78 patients in the HG group). Efficacy evaluation was performed with vessel-clearing scoring on day 14, 28, 42, and 56 after the procedure. In the evaluation, HG treatment was found to be superior to STS at all time points (P<0.01, for all time points). Also, at the end of follow-up, more pigmentation was observed in the STS group than in the HG group (38.3% vs 2.6%, P<0.001). The authors concluded that a 0.2% STS solution was aggressive for the treatment of telangiectasia. They also found that pigmentation occurred more frequently in patients with large telangiectasia (0.8-1 mm) (52.9% vs 27.7%; P=0.021). The authors emphasized that both agents were safe, and no major adverse events were observed in any patient, but HG treatment was more effective.5
Notably, studies conducted in the early 1970s showed that hypertonic solutions did not cause the desired level of endothelial damage to the vessel wall6; however, other studies reported in the literature do show HG solution to be a sclerosing agent.7
Another recent study by Bertanha et al compared treatment with POL plus glucose (0.2% POL and 70% HG, 51 patients) versus glucose alone (70% HG, 47 patients). Post-application evaluations were carried out immediately after the procedure, 7 days after the procedure, and in the second month after the procedure. Combined therapy was found to be more effective in the target area (82.2% vs 63.9%; P<0.001). No major adverse events were reported in either group. When all patients were evaluated, pigmentation was the most common side effect, but larger pigmentation areas have occurred in patients using combined agents (median 0 cm vs 0.5 cm, respectively; P=0.033).8
In a study by Hoss et al, POL treatment was analyzed as sclerotherapy with 1:2 POL to air ratio versus 1:4. At the end of this prospective, randomized controlled study in which 30 patients were included, both methods were found to be effective and similar in terms of complications.9 In another study, STS 0.25% and POL 0.75% were compared in the treatment of lower-extremity telangiectasia. In this study, which included 21 patients, both agents showed similar clinical improvement. When evaluated in terms of complications, it was determined that STS treatment was more painful during the procedure and caused more skin necrosis. However, more pigmentation was observed at the injection sites in POL treatment.10
Laser therapy
The first laser used in the photothermolysis of vascular lesions is the flashlamp-pumped pulsed dye laser (PDL). The wave duration of this laser is 450 μs and small and medium vessels are targeted. It was first used with a wavelength of 577 nm, and the vascular specificity of the laser was increased by making the wavelength 585 nm.11,12 The energy density of the PDL varies between 3 and 10 J/cm2 and the spot size varies between 2 and 10 mm, and these values can be adjusted according to the age of the patient and the lesion area. Purpura is the most common side effect of PDL treatment, and it occurs between 2 and 14 days after treatment. Hyperpigmentation, atrophic scar, hypopigmentation, and hypertrophic scar are complications that may occur in the late period. Because PDL energy can be absorbed by melanin, people with dark skin have less of an effect and a higher risk of complications. Therefore, laser treatment should be planned according to the skin characteristics of the patients (Table I13and Figure 114).
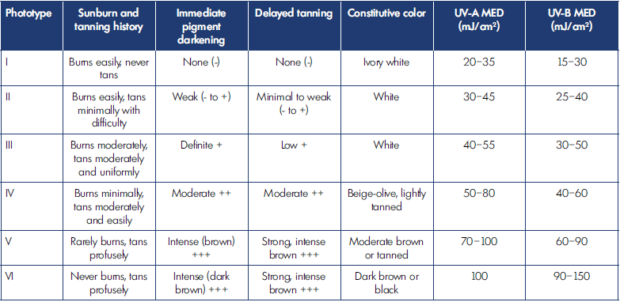
Table I. Fitzpatrick skin phototypes.
Based on reference 13: Pathak MA. J Invest Dermatol. 2004;122:20-21. doi:10.1046/j.1523-1747.2003.22248.x.

Figure 1. Fitzpatrick skin phototype images.
After reference 14: Hindustan Times. Google is searching for
a new method to classify skin tones to curb bias in products. Updated August 21, 2022. https://tech.hindustantimes.com/tech/news/google-is-searching-for-a-new-method-to-classifyskin-tones-to-curb-bias-in-products-71624068839041.html © 2022, Tech Hindustan Times.
The effectiveness of treatment with PDL-585 in a 29-yearold White woman (Fitzpatrick skin type I) has been reported, evaluating treatment success via optic consonance tomography (OCT) imaging. In this case, treatment was applied at 5.5 J/ cm2 with a spot size of 10 mm and 0.5 ms pulse duration. After the treatment, OCT vindicated dropped vascular inflow.15 A clinical report published by Bernstein et al, describes the use of a laser platform that incorporates a new 524-nm laser, pumped by a marketable hair junking laser treatment, in the treatment of spider veins and facial greenishness. In this report, a new 524-nm vascular laser was designed using a 755- nm hair removal laser as a pumping source. It was used to treat facial rosiness and leg telangiectasias in 24 subjects.
This laser could be set up safely and effectively for treating vascularity on the face and legs.16 Thus, laser treatments can be applied clinically in various combinations; this area is open to development.
Intense pulsed light (IPL) is a noncoherent light source and is an important laser in the treatment of telangiectasia with wavelengths in the 500- to 1200-nm range. In this device, each pulse is between 2 and 25 ms, and the delay between pulses varies between 10 and 500 ms. The device gives single, double, or triple light pulses. This condition is also known as “additive healing” and provides an advantage in the treatment of deep vascular lesions.17
The neodymium-doped yttrium aluminum garnet (Nd:YAG) laser is a laser device with a wavelength of 1064 nm and a pulse duration of up to 200 ms, which can be used in the treatment of veins up to 3 mm in diameter in the lower extremities.18 Compared with the PDL-595, this laser is more effective in the treatment of veins between 1 and 3 mm, but it is more painful. A device was also developed by combining PDL-595 and Nd:YAG 1064 from these laser devices (Cynergy with Multiplex, Cynosure, Westford, MA). In this application, the PDL laser is used as a “preheat” device to warm the blood to 70 ˚C. This event converts oxyhemoglobin to methemoglobin. Thus, the absorption of the Nd:YAG laser also increases 4 to 7 times.19
In a recent study, the early effectiveness and safety of an innovative combination of 532-nm and 808-nm transdermal diode laser cure in the treatment of 0.1- to 1-mm telangiectasia were investigated. In this study, which included 94 female cases, these were treated by 3 cycles with a 532-nm laser combined with a contemporaneous 808-nm beat. In these processes, the out-time between the cycles was 10 ms. The esthetic outgrowth was scored by the running physician in a range from 0 (no change) to 10 (100 exposure), and the pain was scored from 0 (no pain) to 10 (most painful experience ever). In inpatient follow-ups, depigmentation was observed in 3 out of 94 cases (3.2), hyperpigmentation in 14 (4.2), flash erythema in 14 (14.9), flash edema in 11 (11.7), and matting in 1 (1.1). The mean esthetic outgrowth was scored as 7.9 by the physician, and cases reported a mean periprocedural pain of 3.4. At the end of the study, the authors stated that contemporaneous operation of 532-nm and 808-nm laser emigration is safe and effective in 0.1- to 1-mm telangiectasia treatment.20
Thermocoagulation
In this treatment method, also known as the radiofrequency energy method, high-frequency waves (4 MHz) are transmitted from the skin to the venous structures via a thin needle, and thermal ablation is provided. This device is the TS-3000, and it includes a needle suitable for the classic surgical electrocautery tip, thus treatment can be performed in this way. It was developed as a special device specifically for the application of this treatment.21,22
The efficacy and side effects of the treatment were investigated in 145 patients (223 extremities), using the TS-3000 device.21 In this study, thermocoagulation was applied to 0.3- to 0.6-mm diameter venous structures. Clinical outcomes were evaluated at 3, 6, and 12 months. At the end of the 1-year follow-up, treatment efficacy was 75.7%, pigmentation was 14.9%, and residual telangiectasia was approximately 15%. In addition to these findings, the absence of skin necrosis during follow-up was considered a positive effect.
In another study, thermal ablation was applied to 30 patients by replacing the cautery tip with a “Given Needle” (US Patent No. US 7,125,406; US 7,628,790) (Figure 2), using standard surgical electrocautery. Here, the device is set to cutting mode, and the wattage is set to 2 MHz (wattage will vary depending on the calibration of the generator). Afterward, ablation was performed by passing the needle through the skin and contacting the subcutaneous venous tissue. Clearance rates of 75% to 100% were observed in 14 cases, 50% in 7 cases, 25% to 50% in 5 cases, and 0% to 25% in 4 cases. Complications included, most commonly, skin erythema (15 cases) and bruising (13 cases), both of which resolved in 2 to 3 weeks with no permanent sequelae, and needle-stick pain (14 cases), which resolved within 3 days. No serious complications such as major vessel thrombosis, serious antipathetic responses, pigmentation problems, ulceration, scar formation, or prolonged pain at the treatment point were observed.22
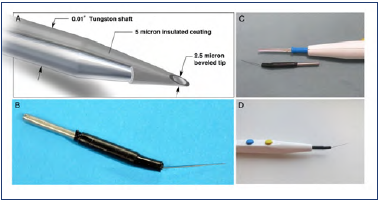
Figure 2. (A) Structures of Given Needle. (B) Given Needle (C) Comparison of the Given Needle and a standard handle type. (D) The Given Needle inserted into a standard handle. After reference 22: Mujadzic et al. Aesthet Surg J. 2015;35(7):NP221-NP2219. © 2015 The American Society for Aesthetic Plastic Surgery, Inc.
Microphlebectomy
Phlebectomy was first described by Aulus Cornelius Celsus. In this method, venous networks are destroyed by needle puncture through a tiny skin incision. Scarring rarely occurs because the skin incisions are made very small. Long-term results are excellent when done in the right indication. Complication development is very rare.23
Comparative literature review of different telangiectasia treatment modalities
Various studies have investigated the effectiveness of different techniques used in the treatment of telangiectasia. The efficacy of long-pulsed 1064-nm (LP1064) and 755-nm (LP755) laser treatments in the treatment of telangiectasia was investigated by Nguyen et al, in which 22 patients with skin type IV were included, and the treatment areas were determined as 2×2- cm areas. In this study, after a 1-month follow-up, the clearance rates for the 2 types of spotlights were not significantly different (71.87 and 71.69, respectively; P=0.99). At the 3-month follow-up, the effectualness was constant, and no recurrence happened. Pain reported with both styles was moderate and significantly lower for LP755. The authors concluded that LP1064 and LP755 laser treatments were comparatively effective and safe for telangiectasia and reticular modes of Fitzpatrick skin type IV cases.24
Munia et al compared sclerotherapy and laser treatments in their prospective study. In this study, 75% glucose solution was used as a sclerosing agent, and Nd:YAG 1064-nm laser was used as a laser device. In this report, in which 30 female patients were included, the treated legs were randomly assigned to the laser and sclerotherapy groups. Pre- and postprocedure photos of all patients were also taken, and these photos were evaluated independently by 2 investigators. In the procedural evaluation of pain, the treatment in the laser group was found to be significantly painful (P<0.001). Effectiveness in terms of appearance was similar in both groups. The authors concluded that both treatments were effective but emphasized that sclerotherapy is a less painful and inexpensive treatment method compared with laser treatment.25
Tepavcevic et al studied the effectiveness of 3 different treatment styles in the treatment of lower-extremity telangiectasia. In the study, which included 30 female cases, persons with skin characteristics ranging from Fitzpatrick I to IV were included. In this study, sclerotherapy (1 mL of 0.5 Aethoxysklerol, 30- gauge needle), laser (Nd:YAG 1064-nm laser wavelength, fluence 110–150 J/cm2, pulse duration 20–40 ms, 3–6-mm spot size; the gel was used for skin contact and after treatment; ice was packed on the skin), and radiosurge coagulation (Ellman Surgitron, blood vessel electrode, coagulation impulse 2 units) treatments were compared. At the end of the 3-month follow-up, sclerotherapy was found to be significantly better than other styles in terms of treatment success (P<0.01) and pain complaints were also significantly lower for sclerotherapy treatment (P<0.01). At the conclusion of this study, the authors emphasized that sclerotherapy is the most comfortable treatment system.26
Parlar et al compared sclerotherapy (POL 0.5%) and Nd:YAG laser (1064-nm long-beat) treatments for lower-extremity telangiectasia in their prospective randomized study. The treated leg was determined randomly, and treatments were applied in 2 sessions at 6-week intervals. Treatment success was evaluated at 6 weeks and 6 months, with 2 independent investigators basing scoring in the range of 0 (no effect) to 6 (100 cleared) on evaluations of pictures. This study found that sclerotherapy brought more rapid improvement, although at the last follow-up visit, blinded assessment showed no difference in clearance between the 2 groups (P=0.84). Still, pain complaints were less common in the sclerotherapy group. The authors concluded that the 1064-nm long-pulsed Nd:YAG laser was associated with more pain, suggesting suitability of this treatment for those with needle phobia, allergy to sclerosants, and in the presence of small veins with telangiectatic matting.27
Since then, the efficacity of laser (Nd:YAG laser with a wavelength of 1064 nm, StarLux 500; Palomar Technologies, Carlsbad, CA, USA) and sclerotherapy in the treatment of lower-extremity telangiectasia has been further studied by Ianosi et al. In this study, sclerotherapy cases were divided into hypertonic saline (20% saline and 2% lignocaine) and POL (0.5%) groups, and treatment efficacity was assessed for 244 (488 legs) female cases over a 6-month period. There were 169 legs in the POL group, 154 in the hypertonic saline group, and 165 in the laser group. Photos of all cases were made before and after the procedure. This evaluation assigned scores between 0 (no change) and 6 (100 cleared) points. From this study, the authors concluded that for telangiectasias under 1 mm, periphery laser was more effective (risk ratio [RR], 9.72; P<0.0001) than hypertonic saline, as was POL (RR, 2.70; P=0.003); for telangiectasias over 1 mm, periphery laser and POL were more effective (RR, 2.70; P=0.003 and RR, 1.44; P=0.00756; respectively); for telangiectasias under 1 mm, laser treatment was superior to POL treatment; for telangiectasias over 1 mm, the hazard regression model showed a hazard ratio of 3.97 (P=0.047) for laser and 4.96 (P=0.486) for POL vs hypertonic saline treatment. The authors concluded that laser treatment is effective in lower telangiectasias and that sclerotherapy with POL becomes more effective as the periphery increases.28
In another recent study, laser (Nd:YAG laser, LAS- StarLux 500), POL-1 (1% polidocanol) and POL-0.5 (0.5% polidocanol) were investigated, including 132 cases (264 branches) with treatments performed by the same physician. The authors concluded that laser treatment was effective in telangiectasias below 1 mm, and both POL treatments were more effective in larger vascular structures.29
Conclusion
Telangiectasias can be treated with various methods. The efficacy of treatment seems to be similar across the different options. Choosing a treatment according to suitability for the individual patient will increase the success rates.
REFERENCES
1. Kern P. Pathophysiology of telangiectasias of the lower legs and its therapeutic implication: a systematic review. Phlebology. 2018;33(4):225-233.
2. Ruckley CV, Evans CJ, Allan PL, et al. Telangiectasia in the Edinburgh Vein Study: epidemiology and association with trunk varices and symptoms. Eur J Vasc Endovasc Surg. 2008;36:719-724.
3. Aydın U, Engin M, Turk T, Ata Y. The effectiveness of different treatment methods in isolated telangiectasia and reticular vein treatment: a single-center prospective randomized study. Phlebology. 2022;37(1):26-32.
4. Bi M, Li D, Chen Z, Wang Y, Ren J, Zhang W. Foam sclerotherapy compared with liquid sclerotherapy for the treatment of lower extremity varicose veins: a protocol for systematic review and meta analysis. Medicine (Baltimore). 2020;99(22):e20332.
5. Bukina OV, Sinitsyn AA, Pelevin AV. Sclerotherapy of telangiectasias: a prospective, randomized, comparative clinical trial of hypertonic glucose versus sodium tetradecyl sulfate. Vasc Med. 2021;26(3):297-301.
6. Imhoff E, Stemmer R. Classification and mechanism of action of sclerosing agents. Phlebologie. 1969;22:143.
7. Bukina OV, Sinitsyn AA. Hypertonic glucose in the treatment of telangiectatic matting: a pilot study. Flebologiya. 2019;13:314.
8. Bertanha M, Yoshida WB, Bueno de Camargo PA, et al. Polidocanol Plus Glucose Versus Glucose Alone for the Treatment of Telangiectasias: triple blind, randomised controlled trial (PG3T). Eur J Vasc Endovasc Surg. 2021;61(1):128-135.
9. Hoss E, Kollipara R, Boen M, Alhaddad M, Goldman MP. Comparison of the safety and efficacy of foam sclerotherapy with 1:2 polidocanol to air ratio versus 1:4 ratio for the treatment of reticular veins of the lower extremities. Dermatol Surg. 2020;46(12):1715-1720.
10. Ramadan WM, El-Hosy KH, Shaaban DM, Hasssan AM, El-Sharkawy MM. Clinical comparison of sodium tetradecyl sulfate 0.25% versus polidocanol 0.75% in sclerotherapy of lower extremity telangiectasia. Gulf J Dermatol Venereol. 2011;18(2):33-40.
11. Anderson RR, Parrish JA. Selective photothermolysis: precise microsurgery by selective absorption of pulsed radiation. Science. 1983;220:524-527.
12. Alster TS, Wilson F. Treatment of port-wine stains with the flashlamp-pumped pulsed dye laser. Ann Plast Surg. 1994;32:478- 484.
13. Pathak MA. In memory of Thomas Bernhard Fitzpatrick. J Invest Dermatol. 2004;122:20-21. doi:10.1046/j.1523- 1747.2003.22248.x.
14. Hindustan Times. Google is searching for a new method to classify skin tones to curb bias in products. Updated August 21, 2022. https://tech.hindustantimes.com/ tech/news/google-is-searching-for-a-newmethod- to-classify-skin-tones-to-curb-biasin- products-71624068839041.html
15. Rajabi-Estarabadi A, Zheng C, Williams N, Smith SC, Nouri K, Kirsner RS. Successful treatment of lower extremity telangiectasias using 585-nm pulsed-dye laser at low fluence combined with optical coherence tomography: a case report. J Drugs Dermatol. 2019;18(11):1180-1182.
16. Bernstein EF, Bhawalkar JD, Shang X, et al. A laser platform incorporating a novel 524 nm laser pumped by a commercial hair removal laser effectively treats facial redness and lower-extremity spider veins. Lasers Surg Med. 2022;54(1):82-88.
17. Tanzi EL, Lupton JR, Alster TS. Lasers in dermatology: four decades of progress. J Am Acad Dermatol. 2003;49(1):1-31.
18. Lupton JR, Alster TS, Romero P. Clinical comparison of sclerotherapy versus longpulsed Nd:YAG laser treatment for lower extremity telangiectases. Dermatol Surg. 2002;28:694-697.
19. Karsai S, Roos S, Raulin C. Treatment of facial telangiectasia using a dualwavelength laser system (595 and 1,064 nm): a randomized controlled trial with blinded response evaluation. Dermatol Surg. 2008;34:702-708.
20. Crippa A, Menegatti E, Zini F, et al. Safety and short-term efficacy of telangiectasia treatment by means of an innovative combination of 532 and 808 nm transdermal diode laser. Phlebology. 2019;34(10):715-720.
21. Burleva EP, Ektova MV, Belentsov SM, Chukin SA, Makarov SE, Veselov BA. Treatment of lower extremity telangiectasias by thermocoagulation method using TS-3000 apparatus. Article in Russian. Ambulatornaya khirurgiya. 2018;(1-2):72- 79.
22. Mujadzic M, Ritter EF, Given KS. A novel approach for the treatment of spider veins. Aesthet Surg J. 2015;35(7):NP221-NP2219.
23. Ramelet AA. Phlebectomy. Technique, indications and complications. Int Angiol. 2002;21:46-51.
24. Nguyen HTN, Firas AN, Van TT. Longpulsed 1064-nm and 755-nm lasers for C1 leg veins on skin type IV patients: a side-by-side comparison. Lasers Med Sci. 2021;36(4):829-835.
25. Munia MA, Wolosker N, Munia CG, Chao WS, Puech-Leao P. Comparison of laser versus sclerotherapy in the treatment of lower extremity telangiectases: a prospective study. Dermatol Surg. 2012;38(4):635-639.
26. Tepavcevic B, Matic P, Radak D. Comparison of sclerotherapy, laser, and radiowave coagulation in treatment of lower extremity telangiectasias. J Cosmet Laser Ther. 2012;14(5):239-242.
27. Parlar B, Blazek C, Cazzaniga S, et al. Treatment of lower extremity telangiectasias in women by foam sclerotherapy vs. Nd:YAG laser: a prospective, comparative, randomized, open-label trial. J Eur Acad Dermatol Venereol. 2015;29(3):549-54.
28. Ianosi G, Ianosi S, Calbureanu- Popescu MX, Tutunaru C, Calina D, Neagoe D. Comparative study in leg telangiectasias treatment with Nd:YAG laser and sclerotherapy. Exp Ther Med. 2019;17(2):1106-1112.
29. IanoȘi NG, Neagoe CD, Tutunaru CV, et al. Single blind, randomised study regarding the treatment of the telangiectasia of the lower limbs (C1EAP) using polidocanol 0.5%, 1%, and Nd:YAG laser. Curr Health Sci J. 2020;46(2):141-149.
