Wound healing assessment
Besançon, France
from Agache P, Humbert P, eds.
Measuring the Skin. Berlin :
Springer; 2004.
ABSTRACT
Evaluation of healing requires the qualitative and quantitative analysis of chronic ulcers and wounds. The assessment of ulcers has been commonly based on the measurement of the perimeter or the surface of the wound. Nevertheless, the measurement of the volume and the color of a chronic wound is also an important step in its follow-up over time. Quantitative methods which permit the wound healing rate assessment are essential for checking the response to treatments. Numerous techniques are available, ranging from the simple use of tracings to more sophisticated methods requiring the use of cameras, videos, and computers. The parameters most frequently used to measure a wound are the length of the principal axes (length and width of the wound), the projected surface area, and the perimeter. Various mathematical calculations have made it possible to establish a relationship between the surface area of a wound, and its perimeter, length, and width. The most commonly employed technique uses an acetate film to obtain a tracing of the wound perimeter. Computerassisted planimetry is a wound measurement method often used in clinical studies. The most simple method to assess the depth of a wound consists in using a sterile blunt-tipped rod which enables an assessment of the maximum depth of the wound. The use of an alginate mould enables the measurement of wound volume by weighing or water displacement. Stereophotogrammetry allows the measurement of the contours, surface area, and volume of a wound. It is based on determining the depth of the wound by viewing from two different angles. Ultrasound takes advantage of the difference in pathlength of an ultrasound wave reflecting at the bottom of the wound compared with the adjacent normal skin. This high-precision and simple method (because of the ability of silicone rubber to harden and be stored) uses profilometric analysis followed by computerized volume assessment. The first stage consists in making a negative imprint of the wound using silicone rubber. In vivo measurement using interferometry and fringe projection is a new method to measure in vivo the volume of ulcers. The three-dimensional reconstruction of profiles of the wound is based on a Fourier-transform method of fringe-pattern analysis. The system is made up of a Charged-Coupled Device (CCD) camera and a projection module. The resolution of the system depends on the fringe width and on the angle between the optical axis of the camera and the optical axis of the projector. The deformation of the fringes over the reference plan is proportional to the height separating the object and the reference plan. Thus, an appropriate algorithm allows the reconstruction of the three-dimensional profile from the projected fringes on the object, in this case the wound. Colorimetry or thered-yellow-black concept for this method consists in taking into account the color characteristics of an ulcer, which are a function of its clinical stage. Necrotic lesions are black, a fibrinous surface looks yellow, and granulation tissue is red. Nowadays, wound measurements or follow-up of healing require the use of quantitative methods, which are available and allow comparison of different treatments.
INTRODUCTION
The measurement of the surface area, volume, and color of a chronic wound is an important step in its follow-up over time. Numerous techniques are available, ranging from the simple use of tracings to more sophisticated methods requiring the use of cameras, videos, and computers. When they exist, the techniques usually employed in outpatient care units to record the woundstate over various time points are often inaccurate. Furthermore, studies of wound healing are often complicated by the few objective measurement methods which can be used in a noninvasive and ethical manner in man.1 However, quantitative methods that permit the wound healing rate assessment are essential for checking the response to treatments, either drug-containing dressings or systemic therapies.
Briefly, wound measurements are of value for three main reasons (Table I). The degree of precision required is related to the purpose of the measurement, and also the technique used.
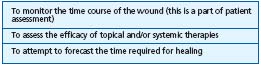
Table I. Objectives of wound measurements.
Wound assessment meets three main difficulties:
● The definition of wound perimeter. This is an entirely subjective estimate that depends on the observer, who decides what forms part of a wound or not. The most frequent source of error comes from the difficult delineation of the epidermis edge, owing to its thinness and translucency.
● The variable aspect of large, deep wounds, which depends on the position of the patient. Such wounds are capable of marked changes in appearance, which render measurements nonreproducible if the patient is not placed in exactly the same position each time the wound is measured.
● The convex shape of human limbs. Measurements frequently do not keep in view possible errors due to this factor.
Despite such problems, several measurement techniques may be employed to assess the surface or volume of wounds. Table II lists the principal ones.
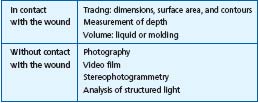
Table II. Wound measurement techniques.
WOUND PARAMETERS: PERIMETER AND SURFACE AREA
The parameters most frequently used to measure a wound are the length of the principal axes (length and width of the wound), the projected surface area, and the perimeter. Different mathematical calculations have made it possible to establish a relationship between the surface area of a wound, its perimeter, length, and width.
Direct measurement of wound dimensions with a ruler
Historically, the first parameters used were the outer dimensions of the wound: length (along the longest axis = L) and width (smaller axis perpendicular to L = W). These parameters are measured directly on the wound using a graduated instrument. The same instrument must always be used if the aim is to compare dimensions, and strict conditions of asepsis must prevail to prevent the transmission of microorganisms between patients. Although imprecise, this technique is the first objective approach to a wound (Figure 1a,b,c). It allows the calculation of the surface area (A), which of course is subject to some error, but this can be partly circumvented through the application of formulae for correcting surface area.2,3 Thus, according to Mayrovitz,3 A = 0.73 x L x W,4 in the case of a rectangular wound. The area of an elliptic wound may be calculated as follows: A = 0.763 x L x W4 or A = 0.785 x L x W.5 This technique is principally applicable when wounds are rather shallow and regularly shaped. Good training in such measurements improves their sensitivity.

Figure 1a. The ulcer.

Figure 1b. Fringe projection on ulcer.
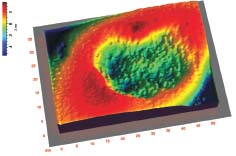
Figure 1c. 3-D reconstruction of ulcer.
Transparent tracings
The most commonly employed technique, delineation of perimeter on transparent material, uses an acetate film to obtain a tracing of the wound perimeter, drawn using a fine marker pen. The paper may be a plain transparent film or may already be calibrated in millimetres. As a general rule, it is better to use a double sheet of transparent material; the tracing is drawn on the upper sheet and the lower sheet, which is in direct contact with the wound and may be soiled by exudate, can be discarded. Flexigrid® opsite (Smith and Nephew) is an adhesive, polyurethane film, which is protective and cross-ruled and can serve as a tracing to follow up the treatment of superficial wounds. The principal limitation to this technique is the difficulty encountered by the observer in determining the perimeter of the wound with enough precision.6 A too thick line is also a source of error.
This is a rapid method (less than a minute is required to complete the tracing of a wound), which is inexpensive and requires minimal training.
Use of scale paper
The next stage consists in analyzing the tracing. As above, the two main diameters, the perimeter and the surface area, can be measured. To measure the surface area the simplest way consists in placing the tracing on a sheet of graph paper and counting the number of 1-mm squares within the area.7,8 This is a tiresome and lengthy method (10 minutes for a 70 cm2 wound). When the wound outline does not perfectly meet the cross-ruling, the area can be deduced using the formula: [N + Nc/2] x surface area of a square, where N is the number of squares fully contained and Nc the number crossing the outline. A more rapid method consists in cutting out the tracing or copying it on a card with a regular thickness, then weighing it on a high-precision scale.6 Additional errors are possible when the drawing is reproduced and the card or film cut out. The use of a scanner that copies the shape of the tracing and enters the data into a computer, or the use of a flat or camera scanner, obviates such drawbacks. A program then allows a rapid and accurate analysis of the tracings, especially calculating its area, and can also measure the area of islands of newly formed epidermis that might have been recognized within the wound and traced.9 This technique is the most widely employed in clinical studies aimed at validating products for wound treatment.
Computer-assisted planimetric measurement
Computer-assisted planimetry is a wound measurement method often used in clinical studies. The perimeter of the wound is delineated by the clinician using a pen linked to a computer. There is a close correlation between the surface area of a wound measured by planimetry and the following parameters: length, width, perimeter, and the product of length by width.10,11 However, this correlation diminishes in the case of very large wounds. In addition, these parameters would be predictive of the healing after 24 weeks. They may be taken either directly on the wound or indirectly from a tracing made on a transparent substrate (tracing paper, plastic film, or mylar),12 or from a photograph taken in a standardized way.
All such measurements enable a calculation of the healing rate, and more particularly of the epithelialization. The latter appeared to be constant in certain studies,13 reaching about 1 to 2 mm per week. Furthermore, this rate would be independent of the size of the wound.
Standardized photography
It is possible to measure wound parameters from a standardized photograph. The method has been compared with the conventional tracing method, and the results obtained do not differ significantly.14 This procedure avoids an important disadvantage of the above methods, direct contact with the wound, which may be painful and a source of contamination. However, as an indirect procedure, it has a number of drawbacks. In order to know the scale of the image, a graduated ruler must be placed alongside the wound. It is often difficult to compensate for the concave or convex nature of the wound. The photograph must be taken exactly perpendicular to the wound. A deviation of only 20° from the perpendicular axis will cause a reduction in the wound surface area of about 10%.15 Indeed, photography must take place under clearly defined conditions in terms of disposition and lighting, and these conditions must be reproducible.16
Various options are available when analyzing a photograph: computer-assisted image analysis is highly preferable to the old-fashioned projection of the photo onto paper and the secondary tracing of wound contours. Interestingly, the information obtained from photographs permits the assessment of wound parameters other than dimensional ones: aspect of the wound bed; changes in color; presence of necrosis, fibrin, or granulation tissue; and epithelialization. Standardization of the technique is essential: choice of focal distance, adjustment of speed and diaphragm, lighting, distance from the wound, angle of shot. One group of authors17 used a Polaroid camera with accessories that allowed them to take photos at a constant angle and distance from the wound, thus enabling comparisons between photos. New Polaroid® systems are particularly well suited to the measurement of wounds. Health Cam System® allows the alignment of two lights, so that photographs are taken in a reproducible and comparable manner. Gridfilm® allows for the superimposition over the wound of a grid, which enables its direct measurement. In most cases, a graduated scale is placed alongside the wound and later enables an easy measurement of its dimensions whatever the magnification of the photo. In the semimanual recording technique the contour of the wound is followed by a digital pen. The signal thus emitted, whose motion has previously been calibrated, is processed by microcomputer. Another technique consists in superimposing the contour traced by the operative using a mouse, over the digital image of the wound, this being visualized directly on the computer screen (image patterning process).18
In practice, a direct data recording from a photograph is difficult to obtain, except in the case of a wound with a simple, geometric shape and a well-defined perimeter. The use of calibrated photographs may be of value when studies are made in a single center, because the reproducibility required with respect to the conditions of photography at different stages of a treatment can be satisfactory. The current need for multicenter studies to assess wounds limits this method of evaluation, and tracings should be preferred. Techniques involving photographs appear to benefit from a certain degree of reliability and reproducibility, only if strict rules are respected.14,19
Video image analysis
This method employs a video camera to film the wound.20 The recording of the image is then analyzed by a computer using a special software program, which permits correction of the figures obtained for wound dimensions to compensate for the concave or convex nature of the wound. The technique is more accurate than the analysis of photographs, and is simple, rapid, and inexpensive.
A comparison of measurements using rulers, tracings or photographs is shown in Table III.21

Table III.
Comparison of three techniques
to measure the surface area
of a wound.21
* The lowest percentage corresponds to large wounds and the highest percentage to small wounds.
WOUND VOLUME
Graduated ruler
The depth of a wound is not accessible to the measurement systems we have described above, because most wounds are three-dimensional (3D). It is necessary to employ specific techniques. The most simple consists in using a sterile blunt-tipped rod, which enables an assessment of the maximum depth of the wound.22,23 The technique involving the use of a cotton tip is easier in practice. However, such measurements are often inaccurate, and determination of the deepest point of the wound is subjective.
Kundin5-24 developed a mathematical formula to assess the volume V of a wound through its surface area A, using the two largest diameters (length L and width W) and the depth (D): V = A x D x 0.327, where A = L x W x 0.785. Thomas and Wysocki23 showed that these measurements were comparable to those obtained with tracings and photographs in the case of small wounds, and were consistently underestimated in the event of large or irregular wounds (particularly those with a sinuous shape). Variation in the measurement of the same wound, with the patient in the same position, nevertheless demonstrated standard deviations of 40% regarding wound volume when using these methods.25
Wound molds using silicone rubber
This high-precision and simple method, because of the ability of silicone rubber to harden and be stored, uses profilometric analysis followed by computerized volume assessment.26,27 The first stage consists in making a negative imprint of the wound using silicone rubber of a type frequently used in dentistry for its safety. Two products are commonly used: Silflo® and xanthoprene. The mixture obtained by mixing the silicone rubber with its catalyst has a viscous consistency and is applied into the wound using a spatula. It will shape all the wound contours to a very fine extent, penetrating into the smallest crevices. After 2 to 3 minutes’ polymerization, and thus hardening, it is easy to remove as a single piece corresponding to the negative shape of the wound. It is possible to store and archive this mold, as it will be unaffected by time. It is then scanned by a laser beam, which recognizes the location of each point using a positional detector. The vertical position of the laser spot (about 30 μm in diameter) can be deduced using double triangulation (Stil, Marseille, and Digital Surf, Besançon) or after refocalization of the beam (Optilas, Evry, France). Parallel linear scanning of the mold surface creates a certain number of profiles, the sum of which enables the calculation of wound volume. When assessing the volume of a leg ulcer, it is recommended to perform laser scanning along the axis of the leg, so as to cancel out the usual concave shape of the wound in this site. This method also permits in some cases a precise definition of wound contours by automatic detection, which is achieved by comparing altitude at each point with that of adjacent healthy skin.
The time course of a wound or its healing is a dynamic process. Monitoring thus requires repeated measurements over time. This method makes such measurements possible, particularly because of the safety of the silicone rubber used and the painless and nontraumatic nature of its application.
Weighing alginate molds
The use of an alginate mould enables the measurement of wound volume by weighing or water displacement.28 However, this method has certain limitations, particularly because of possible alterations in the alginate mold depending on its water content, conditions of storage, and of wound volume.
Stereophotogrammetry
Stereophotogrammetry29 allows the measurement of contours, surface area, and volume of a wound. It is based on determining the depth of the wound by is viewing from two different angles. The first models of this device were difficult to manipulate30, but new, simpler models are now available.29 The accuracy ensured by this method is about 3.5% regarding measurement of the surface area and 5% regarding volume. This method, developed by Bulstrode in 1986,29 is not widely used. The time necessary for each evaluation is a further limitation to its everyday use.
Direct measurement of volume using physiological saline and a polyurethane film
Berg31 recalled the value of this simple method which consists in placing a transparent adhesive film over a wound, and then injecting physiological saline below the film. The quantity of saline corresponds to the wound volume.
In practice, the wound is covered with a sterile polyurethane film and then filled up with physiological saline injected using a needle that pierces the film. Evaluation of this method has shown that accuracy of more than 20% is rarely possible,25 principally because some amount of liquid is absorbed by the wound, and losses by leakage occur around the adhesive, through detachment of the film from the wound perimeter. Furthermore, it is sometimes impossible to place the patient in a satisfactory position to fill the wound with a liquid. The existence of tissue detachment also constitutes a limitation to this technique, as does the potential risk of infection, discomfort for the patient, and the risk of trauma to the wound which is inherent to any technique involving direct contact.
Analysis of structured light
This method enables the measurement of the surface area and volume of a wound without direct physical contact. Parallel lines of colored light are projected onto the wound surface area.4 A video camera connected to a computer, records any distortion to the light beams. The dimensions of the wound are then calculated by triangulation. The accuracy of this method is similar to the previous one, but its implementation is simpler.32
Ultrasound
This technique takes advantage of the difference path length of an ultrasound wave reflecting at the bottom of the wound as compared with the adjacent normal skin. Healing may be assessed using this technique,33 as was demonstrated in a clinical study of wounds caused by punch biopsies in volunteer subjects. In this study, the depth and internal diameter of the wound were assessed by ultrasound at intervals, while its outer surface area was measured by planimetry after first taking a tracing. This technique appears to be of value only if the wound is of a small size, because it is necessary for the wound edges to lie within the field of the ultrasound beam, as they serve as a reference to measure wound depth. Application of the probe must not flatten these edges, and appropriate precautions must be taken to avoid this. Several ultrasound scans should be taken (usually three), from which mean values of the parameters are determined. Ultrasound may also be useful to monitor wound dimensions following cryosurgery, or to better assess the quality of perilesional tissue.34,35
In vivo measurement using interferometry and fringe projection
A new technology based on interferometry principle has been developed in the Laboratory of Engineering of Besançon-France (Humbert P, unpublished data) in order to quantify the volume of ulcers in vivo. The 3D reconstruction of profiles of the wound is based on Fouriertransform method of fringe-pattern analysis (Figure 1).
The system is composed of a CCD camera and a projection module. The resolution of the system depends on the fringe width and on the angle between the optical axis of the camera and the optical axis of the projector. The deformation of the fringes over the reference plan is proportional to the height separating the object and the reference plan. Thus, an appropriate algorithm allows the reconstruction of the 3D profile from the projected fringes on the object, in this case the wound.
This system has a resolution of 10 μm for a 5 x 5 cm2 area. The search for the perimeter and the volume of the wound is based on the method previously described by Zahouani et al.26
A comparison between the above quoted measurement techniques is shown in Table IV.25
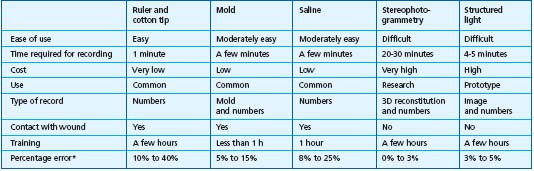
* The lowest percentage corresponds to large wounds and the highest percentage to small wounds.
Table IV. Comparison of five methods to measure wound volume.25
COLORIMETRY OR THE RED-YELLOW-BLACK CONCEPT
The technology for this concept was developed by Hellgren and Vincent36,37 and consists in taking account of the color characteristics of an ulcer, which are a function of its clinical stage. Necrotic lesions are black, a fibrinous surface looks yellow, and granulation tissue is red. This clinical description has been accepted worldwide as an indication of the stage and prognosis of an ulceration.38,39 Thus computerized colormetry analysis (CWA: computerized wound analysis) was developed to ensure more objective measurements.40 A photograph of the wound is taken, together with a gray scale placed alongside the lesion to control the quality of the photograph. Photographic data are transmitted to a computer. The image is digitalized and reconstituted in the form of colored pixels. The color of each pixel is expressed in red, blue, and green values of intensity (each from 0 to 255). This method has been the subject of validation studies. In practice, the clinician takes the photographs using a camera recommended by the CWA Institute in Sweden, the promoter of the technique. Images are then sent to this center where they are processed blind. The results are returned within 6 weeks. A detailed guide is provided regarding the best way for taking the photo, as the reliability of the results depends upon its quality.
CONCLUSION
The clinical follow-up of wound healing requires data on the geometry of the lesion. This quantification is necessary to ensure an objective assessment. The techniques most widely employed in clinical studies involve the tracing of wound contours using transparent film. Only a rigorous training in this technique made it possible to lend credence to the results obtained. More sophisticated techniques that increase the accuracy of wound volume measurements are currently available, but are at present only employed in a research setting.
REFERENCES
2. Vowden K. Common problems in wound care: wound and ulcer measurement. Br J Nurs. 1995;4:775-779.
3. Mayrovitz HN. Shape and area measurement considerations in the assessment of diabetic plantar ulcers. Wounds. 1997;9:21-28.
4. Schubert V. Measuring the area of chronic ulcers for consistent documentation in clinical practice. Wounds. 1997;9:153-159.
5. Kundin J.I. A new way to size up wounds. Am J Nurs. 1989;89:206-207.
6. Bohannon RW, Pfaller BA. Documentation of wound surface area from tracings of wound perimeters. Phys Ther. 1983;63:1622-1624.
7. Gowland Hopkins NF, Jamieson CW. Antibiotic concentration in the exsudate of venous ulcers: the prediction of ulcer healing rate. Br J Surg. 1983;70:532-534.
8. Majeske C. Reliability of wound surface measurements. Phys Ther.1992;72:138-141.
9. Coleridge Smith PD, Scurr JH. Direct method for measuring venous ulcers. Br J Surg. 1989;76:689.
10. Kantor J, Margolis DJ. Efficacy and prognostic value of simple wound measurements. Arch Dermatol. 1998;134:1571-1574.
11. Kantor J, Margolis DJ. Is planimetric wound measurement really necessary? The efficacy and prognostic value of simple wound measurements. Wound Repair Regener. 1998;6:A245.
12. Liskay AM, Mion LC, Davis BR. Comparison of two devices for wound measurement. Dermatol Nurs. 1993;5:437- 441.
13. Redden RA, Blum B, Kilpadi D, Feldman D. Quantitative assessment of wound healing rate. Wound Repair Regener. 1998;6:A246.
14. Griffin JW, Tolley EA, Tooms RE, Reyes RA, Clifft JK. A comparison of photographic and transparency-based methods for measuring wound surface area: research report. Phys Ther. 1993;73:117-122.
15. Palmer RM, Ring EFJ, Ledgard L. A digital video technique for radiographs and monitoring ulcers. J Photographic Sc. 1989;37:65-67.
16. Teot L, Griffe O, Cherenfant E, Breuer JL. Photographie des plaies : standardisation, stockage, pièges à éviter. J Plaies Cicatris. 1996;4:25-30.
17. Minns J, Whittle D. A simple photographic recording system for pressure sore assessment. J Tissue Viability. 1992;2:126.
18. Mignot J. Techniques morphométriques d’évaluation de la cicatrisation d’un ulcère. Rev Prat. 1996;46:S18-S22.
19. Etris MB, Pribbles J, LaBrecque J. Evaluation of two wound measurement methods, in a multicenter, controlled study. Wounds. 1994;6:107-111.
20. Solomon C, Munro AR, Van Rij AM, Christie R. The use of video image analysis for the measurement of venous ulcers. Br J Dermatol. 1995;133:565-570.
21. Plassman P. Measuring wounds. J Wound Care. 1995;4:269-272.
22. Covington JS, Griffin JW, Mendiius RK, Tooms RE, Clifft JK. Measurement of pressure ulcer volume using dental impression materials: suggestions from the field. Phys Ther. 1989;69:690-693.
23. Thomas AC, Wysocki AB. The healing wound: a comparison of three clinically useful methods of measurement. Decubitus. 1990;3:18-25.
24. Kundin J.I. Designing and developing a new measuring instrument. Preoperative Nurse Quart. 1985;1:40-45.
25. Plassman P, Melhuish JM, Harding KG. Methods of measuring wound size: a comparative study. Wounds. 1994;6:54-61.
26. Zahouani H, Assoul M, Janod P, Mignot J. Theoretical and experimental study of wound healing: application to leg ulcers. Med Biol Eng Comput. 1992;30:234-239.
27. Humbert P, Assoul M, Mignot J. Technique volumétrique des plaies. J Plaies Cicatris. 1998;12:53-54.
28. Stotts NA, Salazar MJ, Wipke-Tevis D, McAdoo E. Accuracy of alginate molds for measuring wound volumes when prepared and stored under varying conditions. Wounds. 1996;8:158-164.
29. Bulstrode CJK, Goode AW, Scott PJ. Stereophotogrammetry for measuring rates of cutaneous healing: a comparison with conventional techniques. Clin Sci. 1986;71:437-443.
30. Erikson G, Eklund AE, Tolergard K. Evaluation of leg ulcer treatment with stereophotogrammetry. Br J Dermatol. 1979;101:123-131.
31. Berg W, Traneroth C, Gunnarson A. A method for measuring pressure sores. Lancet. 1990;335:1445-1446.
32. Plassman P, Jones BF. Measuring leg ulcers by color-coded structured light. J Wound Care. 1992;1:35-38.
33. Pugliese PT, Moncloa F, McFadden RT. Ultrasound evaluation of wound volume as a measure of wound healing rate. In: Altmeyer P, Le-Gammal S, Hoffmann K, eds. Ultrasound in Dermatology. Berlin, Germany: Springer-Verlag; 1992:267-272.
34. Rippon MG, Springett K, Walmsley R, Patrick K, Millson S. Ultrasound assessment of skin and wound tissue: comparison with histology. Skin Res Technol. 1998;4:147-154.
35.Wertheim D, Malhuish J, Williams R, Harding K. Ultrasound imaging of the leg in patients with chronic wounds. Skin Res Technol. 1999;5:53-55.
36. Hellgren L, Vincent J. Evaluation techniques for the assessment of wound healing. In: Westerhof W, ed. Leg Ulcers: Diagnosis and Treatment. Amsterdam, The Netherlands: Elsevier Science Publishers BV; 1993;381-384.
37. Vincent J, Bengtsson U, Engström N, et al. Computerized wound analysis. In: Wadström T, Holder IA, eds. Molecular Pathogenesis of Surgical Infections. Stuttgart, Germany: Gustav Fischer; 1994:257-272.
38. Stotts NA. Seeing red and yellow and black. The three-color concept of wound care. Nursing 1990;20:59-61.
39. Thomas S. Wound Management and Dressings. Pharm Press. 1990:81.
40. Engström N, Hansson F, Hellgren L, et al. Computerized wound image analysis. In: Wadström T, Eliasson I, Holder I, Ljung A, eds. Pathogenesis of Wound and Biomaterialassociated Infections. London, UK; Springer; 1990:189-192.
